Blood lipid composition: interpretation and diagnosis
The content of various fats and their ratios in the blood is an important indicator of a person’s health. In some cases, it needs close monitoring, and sometimes correction. Let's figure out where the fats in the blood come from and how to keep track of them.
The role of fats in the body
The membranes of all cells in our body are a double lipid layer. Nerve fibers covered with a layer of myelin (a substance consisting of 75% fat) conduct impulses hundreds of times faster than “naked” fibers.
Without fats, fat-soluble vitamins D, E, K, A do not work (therefore, it is better to season carrot salad with vegetable oil). Hormones are built on the basis of the cholesterol molecule - sex hormones and glucocorticosteroids. And even the folds of fat on the body, from the point of view of nature, have a deep meaning: they are a shock absorber, insulation, and a reserve in case of hunger.
And at the same time, excess fat is a recognized risk factor for many diseases, from atherosclerosis to diabetes. Physical deposits of fat around and inside organs make them difficult to function. In addition, fat is a hormonally active substance, and its excess interferes with the functioning of the endocrine system, disrupting the balance.
The main fats that enter the body from the outside are triglycerides (neutral fats) and cholesterol. Triglycerides are used primarily as a storage substance and substrate for energy production. Cholesterol is the basis for the synthesis of steroid hormones, bile acids and vitamin D.
Types of lipoproteins in the blood
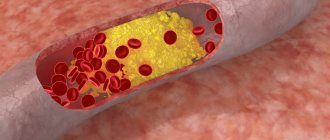
Fat cannot travel in the blood in the form of an ordinary drop, like in soup. Fats are transported in the body in the form of lipoproteins (LP) - compounds of fats and proteins. After absorption, fat molecules form conglomerates with protein molecules, and some of the proteins are a kind of label - the address to which fats must be delivered. The more protein there is in a lipoprotein, the higher its density will be.
If you take a blood test for a lipid profile (lipid spectrum), you will see the following names there:
- LDL
- low density lipoproteins. There are few proteins, a lot of fats, the direction of movement is from the liver to the tissues in which lipids should be used. - VLDL
is very low density lipoprotein. The ratio is shifted even more towards lipids, mainly “spare” ones, and these particles are sent to adipose tissue to replenish it. - HDL
is high density lipoprotein. These particles contain a lot of proteins, and they carry cholesterol “out” from the body - its excess will be eliminated through the liver. - TC
is total cholesterol, i.e. contained in all types of drugs in total. Every day, cholesterol comes from food, is produced by the body itself, and is excreted in bile. Therefore, there is the term “cholesterol balance” - 5.2–5.5 mmol/l in the blood. At this level, the risk of atherosclerosis is minimal, and there will be enough cholesterol to build all the necessary substances. - TG
is the sum of triglycerides in all medications.
Good, bad and too good
It seems that we need to fight to ensure that there are many PAPs and fewer of everyone else. Then cholesterol and triglycerides will move towards exit through the bile, and not towards accumulation in the form of atherosclerotic plaques and fat folds. In popular literature, HDL is often called “good cholesterol,” and LDL and VLDL are “bad” (although, strictly speaking, this is not exactly cholesterol).
Lipid profile parameters
The laboratory measurement value for total cholesterol and its fractions is mmol/l. Indicators included in the lipid profile:
Normal blood cholesterol levels
- OX (Cho);
- HDL;
- LDL;
- VLDL;
- HM;
- TG;
- KA (IA).
TC – total cholesterol level. KA – coefficient (otherwise, index) of atherogenicity. When assessed by electrophoretic method, fractions are divided:
- alpha lipoproteins or HDL;
- beta lipoproteins – LDL;
- prebeta lipoproteins – VLDL.
The CA value is a laboratory marker that reflects the degree of danger of atherosclerotic changes in blood vessels. It is calculated using the formulas: KA = (LDL + VLDL) / HDL or IA = (Cho – HDL) / HDL.
What reduces HDL levels
There are genetic reasons for reducing HDL, but it is worth paying attention to the possibilities that can be controlled and bring HDL to a healthy norm.
Consumption of artificial trans fats
Artificial trans fats, found in margarine and many processed foods, are inflammatory and harmful to our health.
A study of 27 young women found that consuming partially hydrogenated soybean oil resulted in a 10% reduction in HDL levels compared to consuming palm oil. []
A study of 40 healthy adult women compared the effects of consuming trans fatty acids from natural sources with the effects of consuming industrial fats. The result of this comparison was the conclusion that industrially produced trans fats contributed to a decrease in the amount of HDL in the blood. []
Smoking
Cigarette smoking has undoubtedly been shown to be a significant factor in increasing the risk of heart disease. Smoking cigarettes reduces high-density lipoprotein (HDL) levels, and cigarette smoke itself can directly damage the HDL molecule, making it impossible for the molecule to protect the heart and blood vessels from cholesterol and inflammation. []
Diseases
Several health disorders that fall under the category of metabolic syndromes are associated with low levels of HDL in the blood. These disorders include type 2 diabetes , insulin resistance , central obesity (excess belly fat), high blood pressure and high triglycerides . []
In addition, most autoimmune diseases: rheumatoid arthritis , lupus, psoriasis, as well as periodontal disease and any infectious diseases reduce HDL levels. []
How to increase high density lipoprotein levels?
If laboratory tests show a lack of HDL, then the patient should make every effort to return the indicator to normal, and if LDL is also elevated, then this should be done as soon as possible.
Change your habits
If you have low levels of good cholesterol, the first thing you need to do is review your habits. It is necessary to stop smoking, as nicotine lowers the level of good cholesterol and provokes the development of cardiovascular diseases.
Alcohol consumption should be kept to a minimum - strong alcohol should be avoided, but one glass of good red wine can increase HDL levels and lower LDL.
In order to keep all organs and systems of the body healthy, one should not forget about physical activity. The best choice would be regular exercise, not only in the form of playing any sport, for example, swimming, cycling, but also visiting the gym, as well as dancing, active games - football or volleyball. 40-60 minutes a day is enough for good cholesterol levels to begin to increase. However, the effect will only be with regular exercise at least 3 times a week.
If such training is not possible due to excess weight, then you can start with walking, starting with 20 minutes and gradually increasing the duration to 50–60 minutes.
Regular physical activity will reduce the level of bad cholesterol in the body
Overweight
If you are overweight, HDL will gradually decrease as you lose weight. If you lose weight by 3 kg, the level of good cholesterol will increase by 1 mg/dc. To do this, it will be necessary not only to reconsider your diet, but also to increase physical activity. You should not strive to lose weight too quickly - 1-2 kg per week will be an excellent achievement, in this case the weight will not return, and the body will not suffer from sudden surges in blood sugar.
Proper nutrition
Since 20% of all cholesterol enters the body through food, dietary modification can increase the level of good cholesterol.
First of all, you must adhere to the following rules:
- Increase your intake of the right fats. To do this, your diet should include avocados, olive oil, nuts, fatty fish, beans and legumes, flax seeds, fruits rich in fiber (apples, pears, plums), soy, dark chocolate, whole grains, liver, chicken and turkey. .
- Avoiding consumption of trans fats. Trans fats are a kind of pure bad cholesterol. By consuming products with it, we get deposits on the walls of blood vessels. They are found in confectionery and sausages, mayonnaise, margarine, spreads, fast food products, and instant food. Avoiding such foods reduces the risk of heart attack and diabetes by half.
- 3Increase your vitamin intake. Nicotinic acid (vitamin B3 or PP, niacin) can increase HDL levels faster than medications. Large amounts of it are found in eggs, dairy products, peanuts, and mushrooms. If necessary, your doctor may prescribe niacin in supplement form.
- Beverages. It is best to eliminate coffee from your diet and replace it with green tea, rich in polyphenols and antioxidants. Just 2-3 cups of green tea is enough for HDL levels to begin to rise. Cranberry juice, rich in polyphenols, will also be beneficial. Drinking 200 ml of fruit drink or juice for a month will help increase HDL levels by 7-9%.
A balanced and healthy diet is an excellent method to bring cholesterol back to normal.
Medications
A decrease in HDL levels may occur due to the use of certain pharmacological agents. These include:
- Anabolic steroid,
- Beta blockers,
- Progestins,
- Benzodiazepines.
If the patient uses such drugs, then medical consultation is necessary; perhaps they can be replaced with natural remedies.
Normal lipid status
The norms for total cholesterol do not depend on gender. For men and women from 20 to 45 years old, the indicators should fall within the range of 3.2-5.2 mmol/l. If the result is equal to or greater than 6.7 mmol/l, then the patient is diagnosed with hypercholesterolemia.
At values below the norm of 3.2 mmol/l – hypocholesterolemia. Both disorders are considered pathologies. Reference values for high-density and low-density lipoproteins differ by gender and age category.
Normal indicators
The values of triglycerides and very low density lipoproteins for men and women are identical:
- TG – 0.41-1.8 mmol/l;
- VLDL – 0.26-1.04 mmol/l.
For the atherogenicity coefficient, only inflated values are of diagnostic value. The higher the KA, the higher the risk of atherosclerosis.
CA norm table
Preparing to donate blood for a lipid profile
Preliminary preparation for analysis is necessary to obtain accurate results. 2-3 days before the prescribed procedure, it is recommended to refuse foods rich in animal fats and alcoholic beverages (including weak alcohol), and stop taking any medications other than those necessary for medical reasons.
The day before the procedure:
- reduce physical activity;
- limit sugar intake.
Blood sampling is performed strictly on an empty stomach. The fasting regime should be at least 8 hours.
Deviation from normal levels of LDL and HDL
Non-standardized lipoprotein values should be considered only in conjunction with triglyceride values and the level of total cholesterol in the blood. When HDL cholesterol is elevated with normal levels of TC and other fractions, this indicates good lipid metabolism. An unfavorable combination is when the level of LDL and TC is increased, and the level of HDL is decreased.
The following indicators accompany chronic diseases:
- hepatobiliary system (hepatosis, cirrhosis, cholecystitis, cholangitis, etc.);
- renal apparatus (pyelonephritis, nephritis, etc.);
- endocrine system (diabetes mellitus, hypothyroidism);
- cardiovascular system (hypertension, atherosclerosis, coronary heart disease, pericarditis, myocarditis, endocarditis, etc.).
As well as some autoimmune and oncological pathologies. If there are no such diagnoses, then the cause may be an unhealthy lifestyle:
- unhealthy diet (predominance of animal fats in the diet, deficiency of vegetables and fruits);
- alcohol and nicotine addiction;
- sedentary lifestyle;
- long-term stress.
In this case, the results of the lipid profile should be regarded as a high risk of developing atherosclerosis and heart disease. With a decrease in HDL, “bad” cholesterol settles on the inner wall of blood vessels, forming cholesterol spots, from which atherosclerotic plaques eventually form. Such growths inside the vessel block blood flow, which causes heart attack, stroke, and dry gangrene of the lower extremities.
Hypocholesterolemia is also harmful to the body. Lack of cholesterol threatens hemorrhagic stroke, destruction of cell membranes, anemia (anemia), osteoporosis, neuropsychological disorders and depression.
With cholesterol deficiency, the synthesis of sex hormones is disrupted. As a result, libido decreases, men experience problems with potency, women's menstrual cycles become disrupted, and there is a risk of infertility.