- Home /
- Branches /
- Rheumatology /
- Hemorrhagic vasculitis
11/01/2021 The article was checked by rheumatologist Borodin O.O. , is for general informational purposes only and does not replace specialist advice. For recommendations on diagnosis and treatment, consultation with a doctor is necessary.
- At the Yauza Clinical Hospital, laboratory (coagulogram, increased levels of the enzyme antistreptolysin-O, IgA) and instrumental (biopsy) research methods are used to diagnose hemorrhagic vasculitis (Henoch-Schönlein disease, purpura).
- Based on the results of the examination, as well as taking into account the clinical picture of the disease, the rheumatologist will develop an individual treatment regimen for the patient, if necessary, using innovative methods of extracorporeal hemocorrection.
- 140 cases per 1 million population - incidence rate of hemorrhagic vasculitis
- More than 60% of cases of hepatitis in adults are accompanied by involvement of the joints, 50% of the kidneys, and 65% of the digestive tract.
- In 95% of cases, timely treatment of Henoch-Schenelein disease contributes to the patient’s complete recovery
sign up for a consultation
About the development of the disease
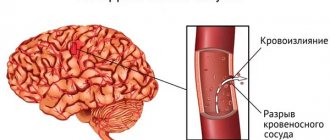
Hemorrhagic vasculitis or Schenelein-Henoch disease is a disease in which autoimmune damage to small arteries occurs - they become fragile, their permeability increases, which causes impaired microcirculation, microthrombosis, multiple small hemorrhages (hemorrhages) as in the skin (hemorrhagic rashes on the skin and mucous membranes) , and in internal organs (gastrointestinal tract, kidneys, joints).
Most often the disease develops in childhood (6-7 years), but can also affect adults. Boys get sick 1.5 times more often than girls.
General and skin symptoms
Symptoms of hemorrhagic vasculitis usually appear suddenly without a prodromal stage. The clinic grows over several weeks. In most cases (especially in adults), a high temperature rises or a low-grade fever is maintained. Patients feel unwell, weak, and have a headache. These are the initial signs of intoxication. The diagnosis is still unclear, since many diseases occur this way.
A more typical sign is a variety of rashes on the body. It can appear on the back of the feet, buttocks, and legs. Less often on the stomach, arms, back. Usually symmetrical in nature.
For hemorrhagic vasculitis, skin manifestations on the face, neck, palms and soles of the feet are uncharacteristic. This sign is taken into account in differential diagnosis.
According to the description, the elements of the rash are different:
- bright red small blisters;
- papules that turn pale when pressed;
- possible location of red papules on the mucous membrane of the mouth and pharynx;
- purple nodules;
- minor bruises.
The diameter of small elements of the rash reaches 1 cm. They last up to four days, then turn pale and disappear. The next wave of skin manifestations should be expected after 7–10 days.
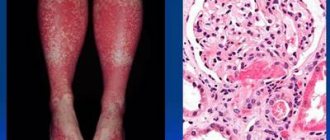
Initial manifestations most often appear as a small petechial rash, localized on the legs and tops of the feet.
Gradually the rash reaches the thighs and buttocks
Much less often the arms, back and stomach are involved in the process. At the same time, patients feel severe itching in the area of the rash, on the surface of the head covered with hair, around the eyes.
On examination, swelling of the lips, eyelids, and perineum is noted. The rash area is painful when touched. After the spots disappear, pigment spots remain, and during relapse they begin to peel.
Causes
The exact cause of hemorrhagic vasculitis (HV) has not yet been clarified, however, most scientists are inclined to the multi-etiological theory of the development of pathology. The leading factors provoking the development of the disease are:
- viral and bacterial infections,
- chronic infections,
- food or drug allergies,
- vaccines.
The mentioned reasons provoke a malfunction of the immune system, which begins to produce pathogenic immune complexes (IgA) that affect the inner lining of small vessels and contribute to the development of inflammation and microthrombosis.
Mechanism of vascular damage
The main factor of damage in hemorrhagic vasculitis is special complexes formed from immune cells. They are called anaphylotoxins for their destructive properties. Under normal conditions they disintegrate. In a sick person, complexes accumulate and become antigens.
Deposition on the inner wall of blood vessels with a change in permeability causes blood circulation problems:
- platelets are activated;
- the plasma content of specific antithrombin decreases;
- the process of fibrinolysis is blocked.
As a result, a mass of microthrombi is formed in small vessels against the background of allergic inflammation and reduced blood clotting.
Symptoms of hemorrhagic vasculitis
There are several forms of hepatitis B:
- Skin or simple : characterized by the appearance of a specific itchy rash on the lower extremities and buttocks (small pinpoint hemorrhages that rise above the skin and do not disappear with pressure). Over time, the red rash darkens and disappears, leaving areas of increased pigmentation.
- Joint: patients complain of pain in the area of large joints (knees, elbows, hips), their swelling and dysfunction.
- Abdominal : nausea and vomiting, severe abdominal pain (often cramping), possible intestinal bleeding, development of intestinal gangrene (due to thrombosis).
- Renal : urine becomes pink or red due to the admixture of red blood cells, its quantity decreases, protein appears in tests, which are signs of the development of glomerulonephritis and the threat of developing chronic renal failure.
- Fulminant : characterized by the development of DIC syndrome and high blood loss.
Often the disease begins with an increase in body temperature to 38-390C, and patients also note general weakness and increased fatigue. Characteristic wave-like course of the disease.
Clinical classification
Clinicians distinguish the following forms of the disease:
- simple or cutaneous - the whole process is limited to skin manifestations;
- skin-articular - in addition to the characteristic skin rashes, there are signs of inflammation of the joints;
- skin-abdominal - against the background of skin changes, symptoms of dysfunction of the stomach and intestines appear;
- renal - rare, accompanied by damage to the renal vessels with impaired filtration and urine excretion;
- mixed (combined) - there are changing symptoms of different forms.
Based on the type of disease, the following are distinguished:
- fulminant form - characterized by a rapid course, lasts several days, occurs in children under 5 years of age;
- acute - the disease has a sudden onset and lasts up to 30 days;
- subacute - lasts up to three months;
- protracted - clinical manifestations last for six months;
- recurrent - characterized by the repetition of symptoms at least four times in the next few years;
- chronic - the clinical picture of the disease lasts several years with periodic exacerbations.
Diagnosis of hemorrhagic vasculitis
At the Yauza Clinical Hospital, patients with suspected Henoch-Schönlein disease are prescribed the following set of examinations:
- general blood analysis;
- general urine analysis;
- coagulogram;
- determination of the level of antistreptolysin-O, IGA in peripheral blood;
- tissue biopsy of the affected organ or part of the body, followed by histological examination of the biopsy.
To make a diagnosis of hemorrhagic vasculitis, the patient must have two or more diagnostic criteria:
- specific rashes not associated with low platelet levels;
- manifestation of the disease before the age of 20 years;
- widespread abdominal pain that worsens after eating, intestinal bleeding;
- granulocytic infiltration of the walls of microvasculature vessels, which is confirmed histologically.
Tests and diagnostics
The diagnosis of hepatitis B is made by identifying specific clinical syndromes, first of all, the presence at the time of examination/history of skin hemorrhagic bilateral rashes and establishing a connection between the onset of breastfeeding and infectious diseases, an allergic history, and changes in diet. There are no specific laboratory tests. Laboratory research:
- OAC - thrombocytosis and nonspecific changes common to any inflammatory process, accelerated ESR, leukocytosis.
- OAM—hematuria/proteinuria.
- Biochemical blood test - blood for CRP, liver tests, creatinine, urea.
- Coagulogram - hypercoagulation is noted, accompanied by a decrease in the activity of antithrombin III and plasmin, and a decrease in chlorides.
- Immunogram - an increase in the concentration of IgA in the blood serum.
- Fecal occult blood test (positive for gastrointestinal bleeding).
In confirming the clinical diagnosis, a leading role is played by a skin biopsy and an immunohistochemical study to reveal the fixation of IgA-containing immune complexes in the vascular wall. If necessary, an ultrasound of the kidneys and abdominal organs and an ECG are prescribed.
Differential diagnosis is necessary with vasculitis in autoimmune diseases ( rheumatoid arthritis , Crohn's disease , systemic lupus erythematosus , ulcerative colitis ), vasculitis of infectious etiology, infections (hepatitis B and C, infectious subacute endocarditis , tuberculosis ), drug allergies and malignant neoplasms.
Therapeutic measures
At the Yauza Clinical Hospital, treatment of hemorrhagic vasculitis is aimed at achieving the following goals:
- elimination of clinical signs of pathology;
- reducing the risk of complications;
- preventing damage to vital organs;
- complete recovery of the patient or achievement of stable long-term remission.
To do this, our rheumatologist develops an individual treatment regimen for each patient, which includes:
- bed rest for at least 3 weeks;
- avoiding contact with allergens;
- diet therapy;
- prescribing enterosorbents, antihistamines, antispasmodics, hemostatic agents and antiplatelet agents;
- in some cases, the use of hormones and cytostatics is justified.
To reduce the destructive influence of circulating immune complexes and enhance the effectiveness of drug therapy, patients with hepatitis B undergo extracorporeal hemocorrection.
How does the disease progress depending on the degree of activity?
To choose the correct therapy for hemorrhagic vasculitis, the doctor needs to know the degree of activity of inflammatory phenomena in the blood vessels. According to the clinic and the simplest laboratory tests, it is customary to distinguish 3 degrees:
- Grade I - the patient’s condition is satisfactory, the temperature is not elevated or slightly above 37, there are moderate non-widespread skin rashes, the ESR in the blood is not higher than 20 mm/hour, there are no other manifestations.
- Stage II - the patient’s condition is moderate, skin manifestations are intense, body temperature is over 38 degrees, there are signs of intoxication (muscle and headaches, weakness), there are clear signs of articular syndrome, abdominal and kidney symptoms are moderate. In the blood test: leukocytosis with eosinophilia and neutrophilia, ESR increases to 40 mm/hour, the ratio of protein fractions is disturbed towards a decrease in albumin.
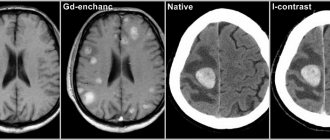
- Degree III - the patient’s condition is objectively assessed as severe, there is a constant high temperature, intense symptoms of intoxication. The patient suffers from the simultaneous manifestation of skin, articular, renal and abdominal syndromes. Possible brain damage. Blood test: high leukocytosis due to neutrophils, ESR exceeds 40 mm/hour, possible decrease in red blood cells, hemoglobin and platelets (anemic syndrome).
The ankle and knee joints are most often affected, rarely the elbows and wrists.
Skin vasculitis
Skin vasculitis is a group of diseases of a multifactorial nature, in which the leading symptom is inflammation of the blood vessels of the dermis and subcutaneous tissue.
The difficulty in covering this topic is that until now there is no generally accepted classification or even agreed upon terminology of vasculitis. Currently, about 50 different nosological forms have been described, and understanding this diversity is not easy. The diversity of clinical manifestations and insufficiently studied pathogenetic mechanisms have led to the fact that under different names only a variant of the main type of skin lesion may be hidden. Also, in addition to primary vasculitis, which is based on inflammatory damage to the blood vessels of the skin, there are also secondary vasculitis (specific and nonspecific), developing against the background of a certain infectious (syphilis, tuberculosis, etc.), toxic, paraneoplastic or autoimmune (systemic lupus erythematosus, dermatomyositis etc.) process. It is possible to transform skin vasculitis into a systemic process with damage to internal organs and the development of severe, sometimes life-threatening complications.
Skin vasculitis is a polyetiological disease. The most common connection is with a focal infection (streptococci, staphylococci, mycobacterium tuberculosis, yeast, viruses, etc.). Hypersensitivity to a number of drugs, in particular to antibiotics and sulfonamide drugs, is of particular importance. Often, despite a carefully collected anamnesis and examination, the etiological factor remains unclear. Among the risk factors for vasculitis, one should take into account: age (children and the elderly are most vulnerable), hypothermia, excessive insolation, severe physical and mental stress, trauma, surgery, liver disease, diabetes, hypertension. The pathogenetic mechanism for the development of skin vasculitis is currently considered to be the formation of circulating immune complexes with their subsequent fixation in the endothelium, although this has not been definitively proven for all diseases of this group.
Skin vasculitis is a heterogeneous group of diseases, and their clinical manifestations are extremely diverse. However, there are a number of common features that unite these dermatoses:
1) inflammatory nature of skin changes; 2) symmetry of rashes; 3) tendency to edema, hemorrhage and necrosis; 4) primary localization on the lower extremities; 5) evolutionary polymorphism; 6) connection with previous infectious diseases, medication, hypothermia, allergic or autoimmune diseases, and impaired venous outflow; 7) acute or worsening course.
Skin lesions with vasculitis are diverse. These may be spots, purpura, nodules, nodes, necrosis, crusts, erosions, ulcers, etc., but the main clinical differential sign is palpable purpura (hemorrhagic rash that rises above the surface of the skin and is felt on palpation).
There is no generally accepted classification of vasculitis. Vasculitis is systematized according to different principles: etiology and pathogenesis, histological picture, severity of the process, features of clinical manifestations. Most clinicians use predominantly morphological classifications of cutaneous vasculitis, which are usually based on clinical changes in the skin, as well as the depth of location (and, accordingly, the caliber) of the affected vessels. There are superficial (damage to the vessels of the dermis) and deep (damage to the vessels at the border of the skin and subcutaneous tissue) vasculitis. Superficial ones include: hemorrhagic vasculitis (Henoch-Schönlein disease), allergic arteriolitis (polymorphic dermal angiitis), leukoclastic hemorrhagic Miescher-Storck microbiota, as well as chronic capillaritis (hemosiderosis): Majocchi's annular telangiectatic purpura and Schamberg's disease. To the deep: cutaneous form of periarteritis nodosa, acute and chronic erythema nodosum.
Hemorrhagic vasculitis is a systemic disease that affects small vessels of the dermis and manifests itself as palpable purpura, arthralgias, gastrointestinal (GIT) lesions and glomerulonephritis. It occurs at any age, but boys aged 4 to 8 years are at greatest risk. Develops after an infectious disease, after 10–20 days. The acute onset of the disease, with fever and symptoms of intoxication, is most often observed in childhood. The following forms of hemorrhagic vasculitis are distinguished: cutaneous, cutaneous-articular, cutaneous-renal, abdominal-cutaneous and mixed. The current can be lightning fast, sharp and protracted. The duration of the disease varies - from several weeks to several years.
The process begins symmetrically on the lower limbs and buttocks. The rashes are papular-hemorrhagic in nature, often with urticarial elements, and do not disappear with pressure. Their color changes depending on the time of appearance. The rashes occur in waves (once every 6–8 days); the first waves of the rash are the most violent. Articular syndrome appears either simultaneously with skin lesions or after a few hours. Large joints (knees and ankles) are most often affected.
One of the variants of the disease is the so-called necrotic purpura, observed during the rapid course of the process, in which necrotic skin lesions, ulcerations, and hemorrhagic crusts appear.
The greatest difficulties are caused by the diagnosis of the abdominal form of hemorrhagic vasculitis, since skin rashes do not always precede gastrointestinal phenomena (vomiting, cramping pain in the abdomen, tension and pain on palpation, blood in the stool).
The renal form is manifested by impaired renal activity of varying degrees of severity, from short-term unstable hematuria and albuminuria to a pronounced picture of acute glomerulonephritis. This is a late symptom and never occurs before the skin is affected.
The fulminant form of hemorrhagic vasculitis is characterized by an extremely severe course, high fever, widespread rashes on the skin and mucous membranes, viscerapathies, and can result in the death of the patient.
Diagnosis of the disease is based on typical clinical manifestations; in atypical cases, a biopsy is performed. In the abdominal form, surgical supervision is necessary. Observation by a nephrologist is recommended for three months after resolution of purpura.
The term “allergic arteriolitis” Ruiter (1948) proposed to name several related forms of vasculitis, differing in clinical manifestations, but having a number of common etiological, pathogenetic and morphological features.
The pathogenetic factors of the disease are considered to be colds and focal infections. The rashes are usually located symmetrically and are polymorphic in nature (spots, papules, vesicles, pustules, necrosis, ulcerations, telangiectasia, blisters). Depending on the predominant elements, three forms of the disease are distinguished: hemorrhagic type, polymorphic-nodular (corresponds to three-symptomatic Gougerot-Duperre disease) and nodular-necrotic dermatitis (corresponds to Werther-Dümling nodular-necrotic dermatitis). When the rash regresses, cicatricial atrophies and scars may remain. The disease is prone to relapse. Often before the rash, patients complain of malaise, fatigue, headache, and at the height of the disease - pain in the joints (which sometimes swell) and in the abdomen. Diagnosis of all types of the disease is difficult due to the lack of typical, characteristic symptoms. Histological examination reveals fibrinoid lesions of small-caliber vessels with the formation of infiltrative accumulations of neutrophils, eosinophils, lymphocytes, plasma cells and histiocytes.
The clinical course of hemorrhagic leukoclastic microbid Miescher-Storck A sign that makes it possible to distinguish this disease as an independent one is the presence of a phenomenon - leukoclasia (disintegration of the nuclei of granular leukocytes, leading to the formation of nuclear dust) during histological examination. Thus, hemorrhagic leukoclastic microbide can be interpreted as a dermatosis caused by chronic focal infection (intradermal tests with streptococcal antigen are positive), occurring with severe leukoclasia.
Chronic capillaritis (hemosiderosis), in contrast to acute purpura, is characterized by a benign course and is exclusively a skin disease.
Schamberg's disease is a lymphocytic capillaritis characterized by the presence of petechiae and brown purple spots, occurring most often on the lower extremities. Patients are concerned solely as a cosmetic defect.
Majocchi purpura is characterized by the appearance on the lower extremities of pink and liquid-red spots (without previous hyperemia, infiltration), slowly growing to form ring-shaped figures. In the central part of the spot, slight atrophy and achromia develop, and vellus hair falls out. There are no subjective sensations.
Periarteritis nodosa is characterized by necrotizing inflammation of small and medium-sized arteries of the muscular type, followed by the formation of vascular aneurysms and damage to organs and systems. Most common in middle-aged men. Of the etiological factors, the most important are drug intolerance (antibiotics, sulfonamides), vaccination and persistence of HbsAg in the blood serum. The disease begins acutely or gradually with general symptoms - increased body temperature, rapidly increasing weight loss, pain in the joints, muscles, abdomen, skin rashes, signs of damage to the gastrointestinal tract, heart, peripheral nervous system. Over time, polyvisceral symptoms develop. Particularly characteristic of periarteritis nodosa is kidney damage with the development of hypertension, which sometimes becomes malignant with the occurrence of renal failure. There are classic and cutaneous forms of the disease. Skin rashes are represented by nodules - single or in groups, dense, mobile, painful. The formation of nodes along the arteries is typical, sometimes they form strands. Localization on the extensor surfaces of the legs and forearms, on the hands, face (eyebrows, forehead, corners of the jaw) and neck. They are often not visible to the eye and can only be determined by palpation. Necrosis may develop in the center with the formation of long-term non-healing ulcers. Periodically, the ulcers may bleed for several hours (a symptom of a “bleeding subcutaneous node”).
Sometimes the only manifestation of the disease may be reticular or branched livedo (persistent violet-red spots), localized on the distal parts of the extremities, mainly on the extensor surfaces or lower back. It is typical to detect nodules along the course of livedo.
Diagnosis of the disease is based on a combination of damage to a number of organs and systems with signs of significant inflammation, fever, changes primarily in the kidneys, heart, and the presence of polyneuritis. There are no laboratory parameters specific for this disease. Dynamic clinical observation of the patient is crucial for diagnosis.
Acute erythema nodosum is a panniculitis that is characterized by the presence of painful pink nodules on the extensor surface of the lower extremities. Accompanied by fever, malaise, diarrhea, headache, conjunctivitis and cough. Among adults, erythema nodosum is 5–6 times more common in women, with a peak age of 20–30 years. The disease is based on hypersensitivity to various antigens (bacteria, viruses, fungi, neoplasms and connective tissue diseases). Half of the cases are idiopathic. Diagnosis is based on history and physical examination. A complete blood count, chest X-ray (detects bilateral adenopathy in the hilar region), a throat swab, or a rapid streptococcal test should be performed.
Chronic erythema nodosum is a group of different types of dermohypodermatitis nodosum. Women aged 30–40 years are most often affected. Nodes of various sizes appear on the legs with reddened skin over them, without a tendency to necrosis and ulceration. Inflammatory phenomena in the area of the rash and subjective sensations (arthralgia, myalgia) are mild. Clinical variants of chronic erythema nodosum have their own characteristics, for example, the tendency of the nodes to migrate (Beferstedt's erythema migrans) or the asymmetry of the process (Vilanova-Pinol hypodermitis).
Tactics for managing a patient with skin vasculitis
- Classify the disease (characteristic clinical picture, anamnesis, histological examination).
- Search for an etiological factor, but in 30% of cases it cannot be established (search for foci of chronic infection, microbiological, immunological, allergological and other studies).
- Assessment of the general condition and determination of the degree of disease activity: general blood and urine analysis, biochemical blood test, coagulogram, immunogram. Degree of vasculitis activity: I. Rashes are not abundant, body temperature is not higher than 37.5, general symptoms are insignificant, ESR is not higher than 25, C-reactive protein is not more than ++, complement is more than 30 units. II. The rash is abundant (extends beyond the lower leg), body temperature is above 37.5, general symptoms are headache, weakness, symptoms of intoxication, arthralgia; ESR is higher than 25, C-reactive protein is more than ++, complement is less than 30 units, proteinuria.
- Assessment of signs of systemicity (research according to indications).
- Determination of the type and regimen of treatment depending on the degree of activity: Art. I. — treatment on an outpatient basis is possible; II Art. - in the hospital. In all cases of exacerbations of skin vasculitis, bed rest is necessary, since such patients usually have pronounced orthostasis, which should be observed until the transition to the regressive stage. A diet excluding irritating foods (alcoholic drinks, spicy, smoked, salty and fried foods, canned food, chocolate, strong tea and coffee, citrus fruits) is recommended.
- Etiological treatment. If it is possible to eliminate the causative agent (drug, chemicals, infection), then resolution of the skin lesions follows quickly and no other treatment is required. But we must remember that when sanitizing foci of infection, an increase in the vascular process may be observed.
- Pathogenetic treatment.
- Preventive measures: medical examination, prevention of provoking factors (infections, hypothermia, insolation, stress, etc.), rational use of medicines, employment, physical therapy, sanatorium treatment.
Treatment of hemorrhagic vasculitis
- Glucocorticosteroids (prednisolone up to 1.5 mg/kg) alleviate the manifestation of skin-articular syndrome, but do not shorten the disease or prevent kidney damage. Prescribed in severe cases and under the cover of heparin, because they increase blood clotting.
- Nonsteroidal anti-inflammatory drugs (NSAIDs) in usual therapeutic dosages. The choice of a specific drug is not of fundamental importance (indomethacin, diclofenac, acetylsalicylic acid).
- Anticoagulants and antiplatelet agents. Heparin for a common process: 300–400 units/kg/day. The duration of the course should be at least 3–5 weeks. Under coagulogram control.
- Therapeutic plasmapheresis, when the manifestations of the disease are not eliminated by the listed means.
- Nicotinic acid in tolerable doses intravenously.
- You should not use: antihistamines (possibly only at the very beginning of the disease), calcium supplements, all vitamins.
Treatment of skin vasculitis
1) NSAIDs (naproxen, diclofenac, Reopirin, indomethacin, etc.); 2) salicylates; 3) Ca preparations; 4) vitamins P, C, antioxidant complex; 5) vasodilators (xanthinol nicotinate, pentoxifylline); 6) 2% solution of potassium iodide, 1 tbsp. l. 3 times a day (erythema nodosum); 7) anticoagulants and antiplatelet agents; detoxification methods IV drip; 9) glucocorticosteroids (GCS) 30–35 mg/day for 8–10 days; 10) cytostatics; 11) ultra-high frequency therapy, diathermy, inductothermy, ultrasound with hydrocortisone, ultraviolet irradiation.
2) salicylates; 3) Ca preparations; 4) vitamins P, C, antioxidant complex; 5) vasodilators (xanthinol nicotinate, pentoxifylline); 6) 2% solution of potassium iodide, 1 tbsp. l. 3 times a day (erythema nodosum); 7) anticoagulants and antiplatelet agents; detoxification methods IV drip; 9) glucocorticosteroids (GCS) 30–35 mg/day for 8–10 days; 10) cytostatics; 11) ultra-high frequency therapy, diathermy, inductothermy, ultrasound with hydrocortisone, ultraviolet irradiation.
External treatment. For erosive and ulcerative rashes
1) 1–2% solutions of aniline dyes; 2) epithelializing ointments (solcoseryl); 3) ointments containing glucocorticoids, etc.; 4) lotions or ointments with proteolytic enzymes (Chymopsin, Iruksol); 5) Dimexide applications;
For knots - dry heat.
Treatment should not end with the disappearance of clinical manifestations of the disease. It continues until laboratory parameters are completely normalized, and in the next six months to a year, patients are given maintenance treatment
Literature
- Adaskevich V.P., Kozin V.M. Skin and venereal diseases. M.: Med. lit., 2006, p. 237–245.
- Kulaga V.V., Romanenko I.M., Afonin S.L. Allergic diseases of the blood vessels of the skin. Lugansk: “Etalon-2”, 2006. 168 p.
- Berenbein B. A., Studnitsin A. A. et al. Differential diagnosis of skin diseases. M. Medicine, 1989. 672 p.
I. B. Mertsalova, Candidate of Medical Sciences RMAPO, Moscow
Contact information about the author for correspondence
How is the treatment carried out?
Treatment of hemorrhagic vasculitis begins with the doctor’s recommendations on the regimen and diet.
In case of exacerbation, strict bed rest is necessary. It is advisable to hospitalize the patient in a hospital, since correction and selection of medications are necessary. They are often administered by drip and intramuscular injection.
Outside of exacerbations, patients should not be in the sun and physical activity should be limited.
The diet for hemorrhagic vasculitis should exclude foods that cause allergies and increase blood clotting.
Not recommended for use in food:
- coffee and cocoa;
- candies;
- citrus fruits;
- eggs;
- spicy seasonings, mayonnaise;
- red varieties of berries;
- fried and smoked meat and fish dishes.
Chocolate is considered a strong food allergen
With the development of abdominal syndrome, the patient is prescribed nutrition with intravenous administration of special solutions. Dietary dishes are prepared according to the principle of table No. 1 (exacerbation of peptic ulcer disease).
Typically, hemorrhagic vasculitis is treated and observed in a clinic by a rheumatologist. Medicines of different groups are used.
To prevent hypercoagulability, the following is prescribed:
- disaggregants (Curantil, Trental);
- Heparin (dose is calculated based on the patient’s weight);
- as an activator of the fibrinolysis process - nicotinic acid in injections.
To relieve inflammation, corticosteroids are used, possibly a combination of tablets and intramuscular injections.
To limit the autoimmune process, cytostatics (Azathioprine, Cyclophosphamide) are rarely used. They are prescribed only in severe cases, for example, with autoimmune glomerulonephritis.
The dosage is selected individually in each case. You cannot change or cancel it yourself.
According to indications, plasmapheresis and transfusion of blood components are performed.
Complications and prognosis
The outcome of hemorrhagic vasculitis in children is generally favorable. Recovery after the onset is observed in more than half of the patients. A long-term recurrent course of the disease is possible, with the frequency of relapses ranging from once over several years to monthly. However, over time, as a rule, the disease becomes monosyndromic: only a skin rash (less often with articular syndrome) or chronic kidney damage develops. At the same time, kidney function remains intact for a long time. The outcome of chronic renal failure is observed extremely rarely, with a mixed form of glomerulonephritis or a rapidly progressing variant.
Sources:
- Rajendra Bhimma, MBChB. Henoch-Schonlein Purpura. — Medscape, Mar 2021.
- Judith Marcin, MD. Henoch-Schönlein Purpura. — Healthline, Jul 2019.
- Union of Pediatricians of the Russian Federation. Federal clinical guidelines for the provision of medical care to children with Henoch-Schönlein disease. — 2015.