Every woman after a certain age faces a natural and irreversible process - menopause. But this new period of life is sometimes overshadowed by the complications of menopause: pain, increased sweating and nervousness, weight gain, depression and bleeding. Why do such problems arise and, most importantly, how to treat them, how to deal with them? Let's figure it out.
Bleeding during menopause: what is it?
During menopause, women often experience bleeding, which can vary in intensity, abundance, pain and consequences. Bleeding during this period is any spotting that should alert the patient. They are not normal and require consultation with a doctor. For many women, menopause is a time when they forget about themselves, intimate life, and visits to the gynecologist. And the appearance of such discharge is a “bell” that should prompt the fair sex to take care of her health.
Menopause has 3 stages: premenopause (menstruation can still sometimes “happen”), menopause itself (when the last “critical days” begin) and postmenopause (the period that occurs after the last menstruation). In all these stages, the appearance of bloody discharge is quite possible. But bleeding during menopause must be treated adequately, clearly selected by a doctor. There is no need to solve this problem yourself. Even if the bleeding was one-time, you still need to be examined.
All about bleeding after menopause
Menopause is the last menstruation in a woman's life. Doctors usually determine this point on the long road of life retrospectively - there was no bleeding for 12 months, which means that that same menstruation was the point of menopause. The average age of menopause in our country is 52 years. For some it happens earlier, for others later.
Sometimes entering this difficult period is accompanied by unpleasant changes in the nature of bleeding. Sometimes sparingly, sometimes abundantly; sometimes often, sometimes rarely. It is not always easy to know whether these changes are normal. We talked in detail about how and why this happens in the article “Cycle disorders after 40 years.”
On the threshold of menopause, you should sound the alarm and consult a doctor for help if:
- menstruation turned into heavy bleeding with large clots;
- menstruation lasts more than 7–10 days;
- menstruation comes at very short intervals - less than 21 days;
- intermenstrual bleeding appeared.
However, in postmenopause, any bleeding is a reason for an urgent visit to a specialist. Even minor bleeding a year or more after the last menstruation may timidly indicate existing troubles.
Why is this happening?
Here is a list of the most common reasons:
Polyps.
As a rule, these are benign formations that grow in the uterine cavity. The polyp can attach quite tightly to the wall of the uterus or grow on the very surface of the endometrium, literally hanging on to the snot. Sometimes the polyp has such a long stalk that it allows it to “peek out” from the cervix. In such cases, the gynecologist sees the polyp during a routine examination on the chair. Although, in fairness, much more often we see with the naked eye polyps that grow from the cervix, and not from the uterine cavity.
Endometrial atrophy.
In deep postmenopause, due to extremely low levels of female sex hormones, the endometrium can become very thin and fragile. This is not at all dangerous; bleeding is usually scanty and does not pose a threat.
Endometrial hyperplasia.
The endometrium has become too thick. We talked in detail about this disease, but in postmenopause this is always a particularly alarming story. Especially if bleeding started first, and then we saw hyperplasia during an ultrasound.
Synechia of the uterine cavity.
Synechiae are fusions. Due to severe endometrial atrophy, the uterus “stuck together.” In postmenopause, this is a variant of the norm, but doctors are often very worried and fussed, for fear of missing a serious problem. In the case of synechiae, the bleeding is usually small, and the ultrasound picture can look scary and resemble severe hyperplasia.
Endometrial cancer.
Unfortunately, this is the most common cause of postmenopausal bleeding. The good news is that endometrial cancer presents itself very early, when there are excellent opportunities for radical treatment. If you don’t sit in an embrace with a hog queen and a red brush for a couple of years, the prognosis is quite positive.
Cervical cancer.
If we diagnose cervical cancer only when a woman presents with postmenopausal bleeding, it is very, very late. But if we take cytological smears from the cervix (from age 21) and do an HPV test (from age 25–30) at least every 3–5 years, we will never miss this disease. Cervical cancer spends about 10 years in the pre-stages, when it is very easy to help. Advanced cancer, which already manifests itself with bleeding from the disintegrating neck, is practically incurable.
We diagnose correctly
Every postmenopausal patient with bleeding is immediately sent to a gynecologist. After a conversation with clarification of details, study of the drug history (hello to self-medication with dietary supplements and phytoestrogens), the doctor conducts an examination on the chair. This usually makes it possible to understand where the blood is coming from: an injury in the vagina, a problem with the cervix, or whether blood is leaking through the cervix from the uterine cavity.
Endometrial biopsy
- a special instrument, as thick as a ballpoint pen, is inserted into the uterine cavity to obtain pieces of the endometrium. A simple and virtually painless procedure that does not require hospitalization, pain relief, or serious preparation.
Transvaginal ultrasound
- the easiest and fastest way to navigate the situation.
Liquid sonohysterography
- introducing a small amount of liquid into the uterine cavity followed by an ultrasound helps to understand dubious situations “polyp or not polyp?”
Hysteroscopy
- a method that allows you to look into the uterine cavity. Office hysteroscopes - thin and flexible - allow you to clarify the situation on an outpatient basis and even take small fragments of tissue for biopsy under vision control. This is a highly informative diagnostic method, especially with questionable ultrasound results. To remove polyps or other more serious medical interventions, you will need a hysteroresectoscope - a larger device that is inserted into the uterine cavity after dilation of the cervix under anesthesia.
Curettage of the uterine cavity
- a way to stop bleeding and obtain material for histological examination. It is performed in a gynecological hospital under anesthesia. An alternative is manual vacuum aspiration of the contents of the uterine cavity, which is performed on an outpatient basis. The choice of method depends on the equipment of the clinic, the severity of the patient’s condition, and concomitant pathology.
How will we be treated?
The choice of treatment depends on the diagnosis. Postmenopausal polyps are removed with mandatory histological examination. Atrophic processes in the endometrium can be treated with medications. Simple hyperplasia also requires drug treatment, but taking into account the high risks in postmenopausal women - under the control of regular endometrial biopsies.
Endometrial cancer is usually treated surgically - the uterus (along with the cervix!), fallopian tubes, ovaries and nearby lymph nodes are completely removed. Further tactics depend on how advanced everything is. If the disease is recognized at an early stage, no further treatment is required. In other cases, radiation therapy, hormone therapy, or chemotherapy are performed.
Any bleeding in postmenopause is a reason to consult a doctor and undergo diagnostic and treatment procedures. There is no need to wait for it to “go away on its own.” Even if the bleeding goes away sooner or later, an unrecognized disease during this time can go too far.
Oksana Bogdashevskaya
Photo depositphotos.com
Classification of bleeding during menopause
Bleeding during menopause is different and can be divided into types. This:
- Organic. Such bleeding is associated with diseases of the kidneys, liver, reproductive and circulatory systems.
- Iatrogenic. Such bleeding occurs due to the fact that the patient is taking some medications.
- Uterine bleeding of a dysfunctional type. They are due to the fact that there is an imbalance in the functioning of the reproductive system, problems with hormones.
You can also distinguish the following uterine bleeding during menopause:
- Menorrhagia - such bleeding is characterized by a duration of more than 7 days and a large amount of discharge. Bloody discharge occurs according to a specific cycle. The woman already knows when to expect them.
- Metrorrhagia. Bleeding of this type is characterized by a small volume of blood, but occurs spontaneously.
- Menometrorrhagia. Such discharges appear without cyclicity, at any time, but they have a large volume of discharge.
- Polymenorrhea. This is discharge that cannot be considered menstruation, but at the same time appears with a certain cyclicity. Usually their interval is 21 days, but no more.
In any case, treatment for bleeding during menopause should be prescribed exclusively by a doctor after a thorough examination. Regardless of what type of bleeding is present, this condition cannot go unnoticed.
Uterine bleeding during menopause (hormone replacement therapy and endometrial safety)
Information prepared by Doctor of Medical Sciences Ya.Z. Zaidieva for distribution to AGE members in the fourth quarter of 2007, based on her work and materials from a number of recent articles in the journal. Maturitas and Climacteric.
UTERINE BLEEDING IN CLIMATERIA (hormone replacement therapy and endometrial safety)
Uterine bleeding during menopause remains a fairly pressing problem, since it can be associated with serious problems for a woman’s health - endometrial hyperplasia and cancer. The inability to control uterine bleeding during this difficult period of hormonal changes in the body is often associated with the difficulty of determining the underlying mechanism of their development in each specific case. The uterine mucosa (endometrium) is of mesenchymal origin and includes two layers: basal and functional. The last layer has the ability to change under the influence of sex hormones and a number of other factors and consists of glandular epithelium, stroma and a dense network of blood vessels. During menopause, gradual atrophy of the functional layer occurs, but the basal layer retains hormonal receptors, has “memory”, plasticity and regenerative properties, i.e. even after menopause it remains a “target” for sex hormones. At the same time, the endometrium has real autonomy, contains an enzymatic apparatus and an immune system, is capable of local steroidogenesis (formation at the local level of estradiol, estrone sulfate, androgens and prolactin), and also produces prostaglandins, growth factors and their receptors. Along with the level of sex hormones in the blood, local production of biologically active substances and cellular regulators affects the proliferation and differentiation of endometrial cells and the occurrence of menstrual bleeding during the reproductive period or a natural menstrual-like reaction (LMLR) when exogenous sex hormones are prescribed. In menopause, the mechanism of action on the endometrium of exogenously administered sex hormones is similar to the endogenous influence of those in women of reproductive age. By binding to their own receptors, estrogens are able to have a direct stimulating effect on the endometrium, as well as an indirect effect through the activation of growth factors. Histologically, the proliferative effect of estrogens is characterized by an increase in the number of mitoses in the nuclei of the glandular epithelium, fibroblasts and vascular endothelium, while the degree of their proliferative effect depends on the type of estrogen and its concentration in the blood. In turn, the level of estradiol in the blood is determined by many factors: the dose of estrogen, method of administration, acceptability, and the activity of metabolic processes in the liver. Progestogens also cause characteristic changes in the endometrium: they suppress the synthesis of estrogen receptors, increase the formation of protein that binds insulin-like growth factor, increase the synthesis of the enzyme 17-dehydrogenase, which promotes the conversion of the more active estradiol into the less active estrone, reduce the residence time of estrogens in the cell nucleus, and regulate processes apoptosis. Histological evidence of the progestogenic effect is the secretory transformation of the endometrium, which was previously exposed to the influence of estrogens, i.e. proliferation, which prevents the development of hyperplasia. Progestogens exert their effect only in the presence of receptors for them, the synthesis of which, in turn, is stimulated by estrogens. . Possible causes of abnormal bleeding in menopause: - Organic pathology (endometrial polyps, endometritis, adenomyosis, atrophy, endometrial cancer, submucous fibroids) should be excluded first. — Hormonal imbalance: dysfunctional uterine bleeding (DUB), as a rule, occurs due to the development of relative hyperestrogenism against the background of a sharp decrease in progesterone levels (“estrogenic” breakthrough bleeding). The occurrence of abnormal bleeding during a particular HRT regimen is most often associated with incorrect selection of therapy or insufficient examination of the woman. — Pathology of the functional layer of the endometrium associated with disturbances of its homeostasis and/or angiogenesis. Capillary rupture (fragility, anomaly) can occur as a result of inflammatory processes (chronic endometritis) or mechanical factors (compression - in the case of fibroids, polyps). It should be emphasized that these disorders are often combined, so a violation of angiogenesis (anomaly in the structure and function of blood vessels) can be observed with hormonal imbalance. After the onset of menopause in women, adipose tissue and, to a lesser extent, skin fibroblasts become the main sources of estrogen formation through conversion from androgenic precursors formed in the adrenal glands, due to the presence in these structures of a fairly high activity of cytochrome P-450 aromatase. The expression of aromatase in adipose tissue increases significantly with age (in the presence of obesity - 10 times), which may play a compensatory role and mitigate the clinical manifestations of estrogen deficiency. However, in postmenopausal women with obesity, the concentration of estrogen in the blood can reach values sufficient for the development of hyperplasia and even endometrial cancer. In addition to excess body weight, the causes of acyclic uterine bleeding can be many factors: dysfunction of the liver, thyroid gland (hypothyroidism), taking medications (anticoagulants, steroids, barbiturates), thrombophilia, etc.
Principles of hormonal therapy in menopause. With long-term use of estrogens without the counteracting influence of progestogens, the risk of developing endometrial hyperplasia and/or cancer increases. Therefore, when prescribing estrogens in women with an intact uterus, progestogens should be used to protect the endometrium from their proliferative effects. Progestogens are not prescribed to women after a hysterectomy, except in cases of common forms of endometriosis, when it is impossible to be sure that all heterotopias will be removed after surgery. Progestogens do not provide “protection” against breast cancer; on the contrary, some types of progestogens may increase the risk compared to estrogen monotherapy. Low-dose estrogens are also not recommended to be prescribed without progestogens, due to an increased risk of developing endometrial hyperplasia and cancer. Treatment of urogenital disorders with vaginal products (Ovestin in suppositories or in the form of a gel) does not require the administration of progestogens, since they do not have a systemic effect. The selection of hormonal therapy is carried out taking into account the nature and severity of menopausal symptoms, the woman’s health as a whole, so, recently, increasing attention has been paid to the need for a gynecologist to assess risk factors for cardiovascular diseases, including arterial hypertension, diabetes, etc. The phase of menopause, the woman’s age and her attitude towards the presence of cervical cancer are also taken into account. Before prescribing HRT, examination of the condition of the endo- and myometrium is mandatory (see Appendix). As already noted, in premenopause, a sharp decrease in progesterone levels is first observed, therefore, if the main symptom in a woman is DUB, monotherapy with progestogens is carried out (Dydrogesterone (Duphaston) at a dose of 20 mg or Utrozhestan at a dose of 300 mg daily for 14 days). If a woman stops responding to this MPR therapy or develops menopausal symptoms, she should switch to a combination therapy regimen. In perimenopause, a combined cyclic therapy regimen is used, which includes, in addition to estrogens in a dose of 2 mg, progestogens in an adequate dosage for 10-14 days monthly (Klimonorm, Femoston 210, Divina, etc.). In preparations for cyclic HRT regimen, as a rule, progestogens seem to dominate, which ensures MMPR in 80-90% of cases, however, the severity of the progestogenic effect on the endometrium differs among different types of progestogens. For example, a sign of insufficient progestogenic activity may be a cervical relapse that occurs a few days before taking the last tablet of the drug. To evaluate it, there is the Kaufman test, during which the so-called “transformation” dose of progestogen is measured, against the background of which its complete secretory transformation occurs according to a histological examination of an endometrial biopsy that has previously undergone proliferation under the influence of a standard dose of estrogen. For example, the transformation dose of levonorgestrel (LNG) is 3.5 mg/cycle, dienogest - 6.3 mg/cycle, cyproterone acetate - 20 mg/cycle. LNG, which is a derivative of 19-nortestosterone and is part of the combination drug Klimonorm at a dose of 0.15 mg for 12 days of each cycle of therapy, has the most powerful progestogenic effect on the endometrium compared to other progestogens. In this regard, this drug is preferable in women with inflammatory processes and simple endometrial hyperplasia, confirmed by diagnostic curettage, and adenomyosis in history or currently, in the presence of DUB, as well as small subserous or interstitially located myomatous nodes. The main parameters of normal PVD against the background of cyclic HRT include: the timely day of its start; moderate duration and intensity; regularity (predictability). MPRs that occur against the background of a cyclic therapy regimen on days 11-13 from the start of taking progestogen for 3 or more cycles are considered natural. This treatment regimen is appropriate for perimenopausal women, but the resumption of menstruation after several years of amenorrhea is usually perceived negatively by women. At present, cyclic therapy is not recommended for use beyond 3 to 5 years in postmenopausal women, as several recent studies suggest a slight increase in endometrial cancer with longer use. The transition from a cyclic regimen to a continuous regimen is carried out under the following conditions: - the patient is most likely already postmenopausal (age 50 years); - when using the cyclic regimen of HRT, MMPR was always noted; in the case of irregular bleeding, their cause should be clarified (!); - the patient stops “responding” with ZMPR to the cyclic regimen of HRT. When switching from a cyclic to a continuous regimen of therapy, you should take a break for 4-6 weeks, perform an ultrasound, evaluate menopausal manifestations or other indications, the presence or absence of spontaneous menstruation. In the absence of menstrual bleeding, if indications for HRT remain and the M-echo value is 5 mm, you can switch to a continuous therapy regimen. In the presence of menstrual bleeding, in addition to ultrasound, the levels of FSH, E2 are determined to clarify the phase of menopause, and possibly, according to indications, the level of CA-125, after which the issue of further management of the patient is decided. If the M-echo value is 5 mm, additional examination is performed: hormonal curettage (progestogens for 10 days) and repeat ultrasound after MPR; according to indications, vacuum curettage (Paipel) or hysteroscopy with separate curettage of the endometrium and cervix. In postmenopause, it is necessary to use a continuous combined regimen of estrogen/progestagen therapy (Angelik, Indivina, Femoston 15, etc.), with these drugs there is no MPR due to the development of endometrial atrophy. This effect is achieved by daily intake of progestogens in doses sufficient to prevent mitosis in glandular cells, but not so high as to cause secretory transformations simultaneously in the glands and stroma. However, the negative side of this treatment regimen is the fairly high frequency of irregular bleeding in the first months of therapy (according to various sources, from 10 to 70%).
Since progestogen is added only to “protect” the endometrium in women with an intact uterus, it seems logical to administer it directly into the uterus to prevent systemic effects. The Mirena LNG-IUS has been used for this purpose for many years in combination with various types of estrogens (oral or transdermal) as part of a combined continuous HRT regimen. Thus, in a recent 5-year study of Mirena in combination with 1.25 mg of conjugated equine estrogens, high adherence of patients to this therapy was revealed (up to 80%) and amenorrhea in 93% of cases; not a single case of endometrial hyperplasia was noted. This is explained by the high progestogenic activity of LNG, which was mentioned above, although it is released into the uterus in an extremely low dose - only 20 g per day. Mirena can be used for contraception in late reproductive age, and then, when menopausal symptoms appear, natural estrogens are added in one form or another, i.e. contraception turns out to be “built-in” into the HRT regimen during the transition period, when a woman still has the ability to conceive. A combined continuous HRT regimen using transdermal forms of estrogens in the form of patches and gels (Divigel, Klimara, Estragel) and intravaginal forms of progestogens (Utrozhestan at a dose of 100 mg in the form of suppositories daily) is preferable in women with already developed menopausal metabolic syndrome, insulin resistance and diabetes 2 type. As mentioned above, monitoring the condition of the endometrium in obese women requires special attention. Abnormal bleeding during various HRT regimens. It should be emphasized that the bioavailability and metabolism of steroid hormones are characterized by individual differences, in addition, there are receptor characteristics of the endometrium. In this regard, the activity of proliferative processes, as well as the usefulness of the secretory transformation of the endometrium and the degree of atrophic processes in it in a particular woman, when using the same (standard) doses of the same sex hormones, may vary, which in some cases contributes to the development of abnormal bleeding. Against the backdrop of a cyclic HRT regimen, these include: - heavy or prolonged bleeding on the expected days of IMPR, as a rule, they are associated with taking progestogens; - acyclic uterine bleeding.
Against the background of a continuous combined HT regimen: - bleeding after a long period of amenorrhea; - bleeding lasting more than 6 months after starting hormonal therapy.
As already noted, against the background of a continuous combined HRT regimen, minor bleeding often occurs during the first 3-6 months of treatment, which may not be associated with its pathology, but due to: adaptation of the endometrium to exogenously administered hormones; endometrial atrophy; a decrease in the bioactivity of sex hormones in the body of a particular woman, as already mentioned. Breakthrough bleeding often occurs when the level of estradiol in the blood plasma is sufficiently high (more than 40 pg/ml). If bleeding persists after 6 months of therapy or is heavy and prolonged, additional examination is required. Further development of ultra-low-dose drugs (estradiol dose 0.5 mg) will help reduce the incidence of these manifestations and increase the acceptability of therapy.
Diagnostics.
Determination of the condition and diagnosis of endometrial pathology is carried out using the following methods: - Ultrasound (endovaginal sensor); — Doppler ultrasonography (echography); — Vacuum curettage (Pipell); — Hysteroscopy + separate diagnostic curettage. Ultrasound is an important method for primary screening of the condition of the endometrium, and the following must be remembered: - against the background of cyclic HRT, it is carried out immediately after MMPR (normal M-echo ≤5 mm); — against the background of a continuous HT regimen, the likelihood of endometrial cancer with M-echo ≤4 mm is minimal; — the thickness of the M-echo against the background of HRT is 1-2 mm greater than in the population; — diagnostic value of the method 90%; — the prognostic value of Doppler ultrasonography is higher than ultrasound; - endometrial cancer can occur regardless of the thickness of the endometrium, i.e. against the background of his atrophy. Thus, transvaginal ultrasound is an accurate method for determining the presence/absence of endometrial pathology. However, when identifying a thick “echoic” endometrium, ultrasound is not informative enough to determine the nature of its pathology, due to low specificity and a high probability of diagnostic error. In this regard, only histological analysis is the “gold” standard in assessing the condition of the endometrium. Indications for endometrial biopsy: Cyclic regimen: - heavy and prolonged withdrawal bleeding; — “breakthrough” bleeding for 2 or more cycles;
Continuous combined regimen: - continued heavy “breakthrough” bleeding for 4-6 months; - the appearance of “breakthrough” bleeding after prolonged amenorrhea. As a rule, after the prescription of hormonal therapy, the first ultrasound is performed 3-6 months later. This visit to the doctor is necessary not only to monitor the condition of the endometrium, but also to determine the effectiveness and acceptability of therapy, i.e. confirmation of the correct choice of drug. Then, in the absence of any pathological symptoms against the background of HT, there is no need to perform ultrasound more often than once a year, when the necessary assessment of the balance of benefits and risks of its further use is carried out.
The creation of new drugs for hormone replacement therapy, reducing the dose of the estrogen component, and selecting an adequate progestogen component make it possible to achieve reliable “protection” of the endometrium and reduce the frequency of “breakthrough bleeding”, increases adherence to this therapy, and helps preserve the health and quality of life of women.
Why does spotting occur during menopause?
There can be many reasons for bleeding during menopause. Some of them are quite harmless, but there are others that indicate a serious illness. As a rule, a woman cannot figure this out on her own, as this requires a detailed consultation with a doctor. But treatment of uterine bleeding during menopause is required almost constantly, and how it will proceed depends on the reasons.
The causes of bleeding during menopause can be:
- Hormonal disorders.
- Taking certain medications, including hormonal and contraceptive medications.
- Early onset of menstruation, absence of labor or a large difference between them, refusal to breastfeed.
- Heredity.
- Uterine fibroids.
- Uterine cancer.
- Ovarian dysfunction.
- Endometriosis.
- Endometrial hyperplasia.
- Polyps that are on the endometrium.
- Vaginitis
- Tumors, ovarian cysts.
- Ovarian cancer.
- Cervical cancer.
Uterine bleeding: symptoms and types
The main symptom is heavy bleeding, which can appear both during menstruation (the volume is much larger than normal) and in the middle of the cycle. In addition, heavy bleeding or bleeding of varying intensity may also occur after a long absence of menstruation. That is, severe uterine bleeding is a violation of duration, volume and regularity.
Pathology can occur at any age:
- from 12 to 18 years - bleeding during puberty or juvenile age;
- from 18 to 45 years - discharge during reproductive age;
- from 45 to 55 years - discharge during the climatic period.
Severe uterine bleeding: general symptoms
- excessive discharge (for example, completely soaking a pad or tampon within an hour, as well as constantly changing pads at night);
- signs of anemia;
- hypotension;
- low blood pressure;
- pale skin and dizziness;
- fatigue;
- uterine discharge with clots;
- the duration of discharge is more than a week;
- painful sensations in the abdomen and lower back;
- discharge after sexual intercourse.
Each clinical case is individual and has its own symptoms, which also depend on the type of pathology.
What symptoms are typical for bleeding?
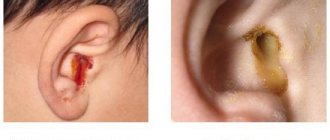
Treatment of bleeding during menopause is a process that requires a careful study of the symptoms of the disease. The main sign of pathology is the presence of bloody discharge. They can be very abundant, and sometimes quite scanty; often such bleeding resembles a “daub”, in which the discharge of blood is insignificant. Sometimes they contain mucus. The color can also be different: from bright scarlet to dark brown. But regardless of this, even a small amount of blood should be considered bleeding. It also happens that the blood changes color from red to black. All these symptoms are extremely dangerous and can indicate the presence of infections, tumors and various problems.
Particularly dangerous symptoms of bleeding are considered to be fever, dizziness, pale skin, cold sweat, a prolonged period of discharge, sharp pain in the lower abdomen, a feeling of heaviness and “fullness” of the space in the lower abdomen. The worst and most dangerous symptom is sudden, heavy bleeding, in which the blood is bright scarlet, not thick, but rather liquid. In this case, the bleeding does not stop and increases, and there is a sharp, throbbing pain in the abdomen. Such conditions require emergency hospitalization and can even lead to the death of the patient.
Publications in the media
The perimenopausal period is a period of a woman’s life characterized by the natural age-related decline of the functions of the reproductive system. Includes the premenopausal period, menopause and 2 years of the postmenopausal period. The premenopausal period is the period from 45 years to the onset of menopause. Menopause - amenorrhea, the first cessation of menstruation and another 6-12 months after it in women over 45 years of age, reflecting natural age-related changes in the reproductive system; On average, the last menstruation occurs at the age of 50.8 years. The postmenopausal period is the period that begins after menopause and lasts until the death of the woman. Physiology of perimenopause and menopause. Changes in the menstrual cycle: irregularity after 40 years, followed by cessation of menstruation.
• Acceleration of oocyte death and atresia of primordial follicles. A small number of maturing follicles leads to increased intervals between cycles or loss of cycles with oligomenorrhea. There is no ovulatory release of FSH and LH, and ovulatory cycles are replaced by cycles with corpus luteum deficiency, then by anovulatory ones. • Changes in hormonal regulation •• Decreased estrogen production, although estrogenic activity is detected for many years after menopause (estrogens mainly come from the adrenal glands, a much smaller part is produced by the ovarian stroma). It is believed that with age, the absolute number of primordial follicles gradually decreases, so by the time of menopause they are practically absent, the development of the next follicle is slowed down or does not occur, which is accompanied by a decrease or absence of estrogen production. In obese women, there is an increased formation of estrone from its precursor androstenedione •• Increased production of gonadotropins through a negative feedback mechanism (FSH from 40 years, LH from 45 years). After menopause, the content of LH increases by 3 times, and FSH by 14 times •• The hormonal activity of the ovarian stroma does not change - androstenedione (the precursor of estrone) and a small amount of testosterone are secreted. • The amount of estrogen is insufficient for proliferative changes in the endometrium, so menstruation usually stops at the age of 50–52 years. • In the absence of the corpus luteum, progesterone synthesis sharply decreases. Lack of progesterone and excess estrogen is one of the causes of dysfunctional uterine bleeding (DUB) and endometrial hyperplasia. • Between the ages of 40 and 55, some women develop excess estrogen, manifested by DUB. Excess estrogen is not associated with ovulation. Reasons for increasing the level of endogenous estrogens: •• Increased androstenedione content in functionally active and inactive endocrine tumors, liver diseases and stress •• Increased estrone production in obesity, hyperthyroidism and liver diseases •• Increased secretion of estrogens by ovarian tumors •• Hypoprogesteronemia. Reaction of target organs to reduced estrogen content • The vagina becomes less distensible, especially in the upper sections, the mucous membrane becomes pale, thinned and dry • The labia minora look pale and dry, the content of adipose tissue in the labia majora decreases • Muscles and ligaments of the pelvis , supporting the uterus and vagina, lose tone, which often leads to uterine prolapse • The endometrium becomes loose, atrophic, with multiple petechial hemorrhages; the number of endometrial glands is significantly reduced. The myometrium atrophies, the uterus decreases in size. Fibroids, if present, decrease in size, but do not completely disappear • The mammary glands lose their elasticity and shape due to the deposition of adipose tissue and atrophy of the glandular tissue • Bone substance gradually loses calcium, resulting in osteoporosis, often accompanied by pain, curvature of the spine and frequent bone fractures • Change of hair type to male due to the relative predominance of androgens.
Clinical picture. According to the nature of the manifestations, menopausal disorders can be divided into several groups • Vasomotor symptoms in most women last 1-2 years, but can last up to 5 years •• “Hot flashes” ••• Sudden redness of the skin of the face, neck and chest, accompanied by a feeling of intense heat and sweating. Duration from several seconds to several minutes. They occur more often and are more pronounced at night or during stressful situations ••• The severity of the climacteric syndrome is determined by the number of “hot flashes”: mild form - up to 10 “hot flashes” per day, general condition and performance are not impaired; moderate severity - 10–20 “hot flashes”, headache, dizziness, pain in the heart, deterioration of general condition and decreased performance; severe form - more than 20 “hot flashes” per day, significant or complete loss of ability to work ••• Treatment with estrogen reduces the frequency and severity of “hot flashes” •• Other symptoms - hyperhidrosis, changes in blood pressure, headaches, chills, palpitations • Emotional and mental: irritability , drowsiness, weakness, anxiety, depression, forgetfulness, inattentiveness, decreased libido • Dry skin, brittle nails, wrinkles, dryness and hair loss • Changes in the menstrual cycle •• Oligomenorrhea followed by amenorrhea •• If uterine bleeding occurs after a 12-month period of amenorrhea , it is necessary to exclude endometrial pathology (polyps, hyperplasia or neoplasia) • Osteoporosis is a degeneration of bone tissue with a restructuring of its structure, characterized by a decrease in the number of bone crossbars per unit volume of bone, thinning, curvature and complete resorption of some of these elements, causing an increased tendency to fractures. Increased bone resorption persists for 3–7 years after menopause •• Clinical picture ••• Compression fractures of the spine (most often - TVIII-LIII) ••• Fracture of the femur with a characteristic localization in the neck and intertrochanteric areas of the femur ••• Fractures of the distal parts of the radius and other bones •• Incidence ••• Approximately 25% of women over 60 years of age not receiving estrogen replacement therapy will experience vertebral compression fractures ••• Approximately 32% will experience one or more hip fractures during their lifetime ••• On average, 16% of women with hip fractures die within 4 months after injury from pneumonia or pulmonary embolism • Atrophic changes •• Atrophic vaginitis, vulvovaginal itching, dyspareunia •• Dysuria, frequent and strong urge to urinate, urinary incontinence •• Cystitis • With an excess of endogenous estrogens, •• DUBs •• Endometrial neoplasia occur. For every abnormal bleeding in women over 35 years of age, an endometrial biopsy should be performed to exclude adenomatous hyperplasia and endometrial carcinoma.
TREATMENT Management tactics • Hormonal therapy •• Replacement therapy is used according to indications in the perimenopausal period •• Sometimes progesterone is prescribed in combination with estrogens • Psychotherapy is indicated for all women, especially in the pathological course of the perimenopausal period • Exercise therapy, warm pine baths, walks in the fresh air, sanatorium -resort treatment • Diet - it is necessary to exclude spicy, salty foods, plant foods (vegetables, fruits) are recommended • Sedative therapy • Vitamin therapy • Prevention and treatment of osteoporosis, cardiovascular complications. Hormonal therapy • Estrogen replacement therapy •• Estrogen therapy helps maintain skin turgor (the skin looks young), does not restore the tone of the muscles of the vagina and pelvic floor •• Absolute contraindications ••• Acute liver diseases ••• Chronic dysfunction of the liver ••• Acute thrombosis vessels ••• Neuro-ophthalmological vascular diseases ••• Ovarian tumors and cysts ••• Cystic mastopathy ••• Recurrent endometrial polyposis ••• Malignant neoplasms of any localization •• Relative contraindications ••• Convulsive syndrome ••• Arterial hypertension ••• Hereditary hyperlipidemia ••• Migraine. • Hormonal therapy in patients after oophorectomy under the age of 40 years or with gonadal dysgenesis •• Long-term cyclic therapy with low doses of estrogens (0.625 mg of estrogens daily from the 1st to the 25th of each calendar month) and progestins (medroxyprogesterone) 10 mg daily from the 16th to 25th day of each calendar month •• Long-term cyclic therapy (estradiol + levonorgestrel, estradiol + cyproterone). • DUB during perimenopause •• Cyclic progestin therapy is recommended to prevent the effect of excess estrogen on the endometrium •• For the treatment of vegetative-vascular manifestations in women with ongoing menstruation, both cyclic hormonal drugs (estradiol + levonorgestrel, estradiol + cyproterone) and non-hormonal methods are used . • Menopause •• When indicated, sequential use of estrogens and progestins in postmenopausal women (as well as in women under 40 years of age). It is recommended to start with a low dose of estrogen and increase the dose as needed to relieve symptoms; progestin is taken from the 16th to the 25th of the calendar month •• A combined drug containing estrogen and progestin (estradiol + dienogest) - used continuously ••• Estrogen therapy helps increase HDL levels ••• Progestin therapy effectively reduces HDL concentrations ••• Atrophy the mucous membrane of the vaginal vestibule, vagina and urethra in late menopause is effectively treated with topical agents (ovestin, estriol - suppositories, tablets, cream) or low doses of oral estrogens •• An alternative to estrogen therapy. Medroxyprogesterone is quite effective in relieving hot flushes when estrogens are contraindicated. Prevention and treatment of osteoporosis . Preventing osteoporosis is easier than treating it. Medications can only slow down the rate of bone loss, but are ineffective at restoring bone substance. • Prevention - early estrogen replacement therapy •• If treatment is started within 3 years from the last menstruation, osteoporosis does not occur •• If treatment is started later than 3 years after the last menstruation, osteoporosis does not occur, but new bone tissue does not form either •• Doses of estrogen ••• Horse estrogens 0.625–1.25 mg daily ••• Ethinyl estradiol 0.025–0.05 g daily ••• Estrone sulfate 1–2 mg daily: •• Additionally, calcium is prescribed in a dose of 1–1.5 g /day • Treatment - see Osteoporosis. Prevention of cardiovascular diseases . The risk of MI in premenopausal women is significantly lower than in men of the same age. This risk is increased in women after menopause. Taking estrogen during menopause significantly reduces LDL and serum cholesterol and increases HDL concentrations. It is recommended to use combination drugs containing estrogens with gestagens • Proginova • Cycloproginova • Estradiol + cyproterone • Gynodian-depot • Femoston • Primella cycle. in postmenopause • Cliogest • Primella-plus. Reduction . DUB - dysfunctional uterine bleeding.
Note. There are artificial menopause - cessation of menstruation after any intervention (for example, oophorectomy, removal of the uterus, X-ray irradiation, medication) and pathological menopause - cessation of menstruation due to a pathological process (uterine tumor, endocrine disorders). Possible causes: genetic predisposition, ovarian failure as a consequence of a secondary autoimmune reaction in rheumatoid arthritis or an inflammatory reaction in mumps.
ICD-10 • M80.0 Postmenopausal osteoporosis with pathological fracture • M81.0 Postmenopausal osteoporosis • N92.4 Excessive bleeding in the premenopausal period • N95 Menopausal disorders and other disorders in the perimenopausal period
How to diagnose pathology?
Menopausal bleeding requires careful diagnosis using the most modern methods. Only they can accurately establish the diagnosis, the cause, and only then can treatment be prescribed. First of all, you will need a detailed medical history, in which the doctor will find out the symptoms, history of the onset of menstruation, childbirth, abortion, surgery and other manipulations. The doctor may also ask about breastfeeding and the presence of gynecological diseases in close relatives. A thorough gynecological examination is required, during which smears are taken from the vagina. Based on initial examinations, the following diagnostic procedures can be prescribed:
- Testing for a hormonal panel, blood testing and blood clotting.
- Additional studies of the liver, kidneys, and thyroid gland.
- Testing for tumor markers, liver tests.
- A vaginal or transvaginal ultrasound is performed.
- A biopsy is performed and biological material is examined to detect cancer.
- An MRI of the pelvic organs is performed
Depending on the results of the study, additional examination procedures may be prescribed. Sometimes the diagnosis of uterine bleeding requires consultation not only with a gynecologist, but also with an endocrinologist, mammologist, oncologist, therapist, and hematologist. If a woman has a number of concomitant diseases, then this problem must be solved comprehensively, using all available specialists.
Juvenile bleeding
At puberty, DUB is characterized by a delay of menstruation for 1.5-3 months, followed by heavy bleeding for more than 7 days. The intensity of bleeding is indicated by the presence of clots and symptoms of anemia (pallor, weakness, dizziness, tachycardia). The diagnosis is not complicated, however, taking into account the physiologically determined irregularity of the rhythm and volume of menstruation in the first 2 years after menarche, you may miss the moment of starting conservative treatment and verification of such congenital endocrinopathies as polycystic ovaries and adrenal cortex dysfunction.
Therefore, mothers should contact their daughters to a gynecologist-endocrinologist if they have doubts about the abundance and regularity of menstruation, the structure of the girl’s skeleton, the nature of hair growth, and the condition of the skin.
Treatment of DUB
To eliminate this type of pathology, gynecologists perform hemostatic procedures, after which they restore the menstrual cycle and exclude the development of a relapse. Depending on the volume of blood lost, surgical or conservative treatment is selected. If hemoglobin exceeds 100 g/l, then conservative treatment is preferred and uterine contractions and hemostatic drugs are used. If there is no result, experts prescribe progesterone medications, which eliminate the pathology within a week after administration and discontinuation.
Surgical treatment is indicated for significant blood loss and when hemoglobin drops below 70 g/l. In this case, the patient experiences a faint state and feels numbness in the limbs. Specialists perform separate diagnostic curettage and hysteroscopy. These treatment methods are contraindicated in the presence of blood diseases (consultation with a hematologist is required). Complex treatment includes taking vitamins B12, B6, C, P. Medicinal preparations with folic acid and iron must be used. Transfusion of fresh plasma and red blood cells will help eliminate complications due to blood loss.
Diagnosis of DMC
Before choosing a treatment strategy, the following is carried out:
- Monitoring ovulation using ultrasound.
- Ultrasound of the pelvic organs, adrenal glands, thyroid gland.
- Taking hormonal tests (total testosterone, LH, FSH, progesterone).
- Checking blood clotting time and taking a blood test.
- Consultation with an ophthalmologist, neurologist, gynecologist, endocrinologist.
How to stop bleeding during menopause?
Treatment of uterine bleeding during menopause depends on the cause. Abnormal uterine bleeding during menopause can be one that requires immediate intervention, or it can be one that requires inpatient or outpatient treatment with conservative methods. If the bleeding is profuse, the abdominal pain is severe, and the woman feels extremely unwell, an ambulance should be called. Next, you need to lie down and put something cold on your stomach. You should not take any medications yourself or try to use traditional methods to stop bleeding.
If abnormal uterine bleeding during menopause is systematic, but does not pose a clear immediate threat to the patient’s life, it requires treatment. It can be conservative or surgical. It all depends on the reasons. If the problem is hormonal, drug treatment is used to stabilize it. If the cause is uterine fibroids, then resection of this organ can be performed. This means that the uterus will be removed. Sometimes the method of ultrasonic abalization is used, in which the fibroids are removed from the uterus. Uterine artery embolization is sometimes used. In this case, the tumor is deprived of blood supply and disappears.
Hyperplasia is treated with laser radiation, liquid nitrogen, and electric current. For endometriosis and polyps, curettage is often used, which stops bleeding and allows material to be taken for examination.
If adenomyosis occurs, then resection of the damaged areas or the uterus is performed.
If there are malignant tumors, they are usually removed along with the organs on which they originated.
Diagnosis of uterine bleeding
When a woman with uterine bleeding consults a gynecologist, he follows a certain algorithm of actions:
- Initial assessment of the severity of the condition (intensity and nature of bleeding, volume of blood loss). Achieved through the collection of complaints, questioning, examination on a chair in the mirrors, palpation.
- Determination of the location of bleeding: vagina, cervix, urethra.
- Identifying a possible connection between bleeding and medication use or concomitant disease.
- Laboratory tests. They include a general blood test, a biochemical blood test, a study of the blood coagulation system, a hormonal examination (female sex hormones, thyroid hormones, for formations in the ovaries - CA-125, HE-4), additional examinations are prescribed according to the situation.
- Transvaginal ultrasound with color Doppler mapping. Carried out by inserting a special sensor into the vagina, it allows you to examine the pelvic organs, measure standard parameters, evaluate blood flow parameters in areas of interest, and compare with norms.
- Assessment of endometrial thickness and structure. Determined using ultrasound. Excessive thickening (> 5 mm in postmenopause) and heterogeneity are signs of endometrial pathology and oncological alertness.
- Hysteroscopy. Examination of the uterine cavity using a thin instrument with a video camera - a hysteroscope. It is most often performed under intravenous anesthesia. Allows you to see all formations and sources of bleeding.
- An endometrial biopsy is performed during hysteroscopy if endometrial cancer is suspected. This is a gentle collection of material for histological examination, which avoids complications such as uterine perforation. .
- Separate curettage of the walls of the uterine cavity and the cervical canal is performed in each case of uterine bleeding during menopause. This is a diagnostic and at the same time therapeutic manipulation, which involves removing the inner layer of the uterus in order to stop bleeding and obtain tissue for histological examination, which allows identifying cancer cells.
Complications of bleeding: what are they?
Heavy bleeding during menopause can have various complications. You should not perceive them as something insignificant and frivolous. Women during menopause often do not want to see a gynecologist and undergo treatment. They believe that if their periods stop, then their life and youth are over. But this is not so: even at this time you can live an active sex life, enjoy and be happy. Therefore, you need to undergo a gynecological examination twice a year. After all, bleeding can have consequences:
- They are life-threatening if they occur suddenly, are very abundant, and can lead to large blood loss.
- They can be a sign of malignant tumors, because if there is prolonged bleeding for no clear reason, then it could be cancer. And the sooner it is detected, the easier it is to cure. Otherwise, a woman may miss precious time and the opportunity to recover.
- If there are benign tumors (fibroids, cysts), no one can exclude the possibility that they will not develop into malignant ones. They need to be removed.
- Hormonal imbalance and constant bleeding will lead a woman to a state of constant stress, nervousness, and inability to have a sexual life.
- Constant bleeding negatively affects all organs and systems of a woman.
Uterine bleeding during menopause is a serious reason to think about your health.
Menopause is “autumn” in a woman’s life. And this period can be pleasant, eventful and easy. It should not be marred by bleeding. But in case of such trouble, you should not be afraid, but you should immediately consult a doctor.
Climax
Menopause
3944 08 September
IMPORTANT!
The information in this section cannot be used for self-diagnosis and self-treatment.
In case of pain or other exacerbation of the disease, diagnostic tests should be prescribed only by the attending physician. To make a diagnosis and properly prescribe treatment, you should contact your doctor. Menopause: causes, symptoms, diagnosis and treatment methods.
Definition
Menopause, or menopausal syndrome, is a complex of vegetative-vascular, mental and metabolic-endocrine disorders that occur in women against the background of fading (or sudden loss) of the hormonal function of the ovaries and general aging of the body.
Causes of menopause
The female ovaries perform an endocrine function (production of sex hormones) and reproductive (formation of an egg). The main sex hormone of a woman of reproductive age, produced mainly by the ovaries, is estradiol - it prepares the female body for conception, controls the development of tissues necessary for implantation of the embryo, the time of ovulation, participates in the normal course of pregnancy and hormonal regulation of childbirth, lactation, etc. Under Under the influence of estradiol during puberty, the final formation of the ovaries, uterus, fallopian tubes, vagina and external genitalia occurs. It stimulates the development of the mammary glands, affects the formation of the bone skeleton, affects peripheral blood vessels, causing their expansion and increased heat transfer, enhances the formation of fat and its distribution, typical of the female figure.
Under the influence of estradiol, the emotional and mental state of women changes.
As the female body ages, ovarian function fades, and accordingly, the production of estradiol gradually decreases. They exhibit a proliferation of connective tissue and are almost halved in size. In women 50–60 years old, the surface of the ovaries becomes coarsely lumpy, and vascular sclerosis forms.
The ovaries turn into flat fibrous plates. Hormone production stops.
Estrogen-sensitive receptors are located in the tissues of the uterus, vagina and mammary glands, in the bladder, urethra, bone and muscle tissue, skin, mucous membranes, heart and blood vessels. Therefore, with estrogen deficiency, changes are observed in these organs. A decrease in estradiol production first leads to menstrual irregularities (prolongation of the cycle, irregular menstruation), and then to a complete cessation of menstruation. The size of the uterus and its cavity decreases, the wall of the uterine body becomes thinner, and the endometrium atrophies.
According to scientific data, only 20% of women do not experience problems during menopause, while for the rest, the decrease and cessation of estrogen production causes various disorders.
Classification
Clinical and hormonal stages of aging of the reproductive system:
Premenopause
begins at 40–45 years of age and is characterized by cycle variability.
Menopause
- absence of menstruation for 12 months.
- premature menopause (before 40 years),
- early (40-44 years),
- timely (45-55 years),
- late (over 55 years old),
- Iatrogenic (secondary), resulting from bilateral oophorectomy (removal of the ovaries), as well as radiation or chemotherapy.
Postmenopause
is the period after menopause, lasting 5–8 years, when menopausal syndrome manifests itself.
Late postmenopausal phase
- vasomotor symptoms become less pronounced.
Symptoms of menopause
The aging process of the body and the gradual decline in ovarian function in different women may vary in duration and be accompanied by different manifestations.
There are specific
manifestations, which include sexual, urogenital, musculoskeletal, psycho-emotional, vasomotor, and
systemic
manifestations - bone loss, visceral obesity, blood lipid imbalance, impaired glucose tolerance, etc.
Due to a lack of estrogen, women complain of hot flashes, increased sweating, and chills. A sudden sensation of heat that occurs in the upper torso and lasts up to 5 minutes, often accompanied by redness of the skin, sweating, and sometimes a rapid heartbeat. Doctors say that during a hot flash, a significant number of women experience decreased cerebral blood flow.
The average duration of hot flashes is 7-8 years, but can be longer (up to 10 years).
Women report sleep disturbances - frequent awakenings, insomnia, difficulty falling asleep and early awakenings. Increased anxiety and mood lability appear. Atrophic changes develop in the mucous membrane of the vagina, vulva, urinary tract, connective tissue and pelvic muscles. A woman may feel dryness, itching, discomfort, sometimes pain in the vagina, and sexual dysfunction. Urinary disorders often occur (frequent urination, predominance of night urination, pain in the bladder, involuntary release of urine with an unbearable urge to urinate).
Changing metabolism of bone tissue with a predominance of destruction over the processes of its formation leads to a decrease in bone strength, which increases the risk of fractures.
Women feel depressed, anxious, their concentration decreases, and their memory deteriorates.
Diagnosis of menopausal syndrome
The diagnosis is established on the basis of a combination of complaints and information received from the patient, physical examination data, laboratory and instrumental data.
Anamnesis collection includes information about the presence of:
- hereditary pathologies (oncological diseases, thromboembolic events, diabetes mellitus, cardiovascular diseases, osteoporosis, fractures);
- complications of pregnancy (gestational diabetes mellitus, preeclampsia, arterial hypertension);
- bad habits;
- concomitant somatic, endocrine and systemic diseases;
- surgical interventions;
- gynecological pathology;
- current or previous drug therapy.
The doctor conducts a visual examination of the external genitalia and bimanual vaginal examination, palpation of the mammary glands, measures waist circumference to determine abdominal/visceral obesity, determines body weight and height to calculate body mass index as an indicator of metabolic disorders.
In case of difficulties in determining the stage of reproductive aging, a hormonal examination is carried out:
- luteinizing hormone (LH);