Quick Transition Treatment of Amyopathic Dermatomyositis
Amyopathic dermatomyositis is a form of dermatomyositis, a rare disease belonging to the group of inflammatory myopathies.
In amyopathic dermatomyositis, inflammatory and degenerative skin changes characteristic of dermatomyositis are observed. But, unlike dermatomyositis, there are no signs of damage to skeletal and smooth muscles (progressive symmetrical muscle weakness of the proximal limbs).
Amyopathic dermatomyositis affects women more often than men (3:1). The onset (first clinical manifestation) of the disease is usually observed at the age of 20-40 years.
Causes
The exact causes of amyopathic dermatomyositis have not yet been established. It is assumed that the triggers of the disease may be immune, genetic and environmental factors. Amyopathic dermatomyositis is classified as an autoimmune disorder because patients with this diagnosis experience abnormal production of autoantibodies by the immune system, leading to inflammatory and degenerative changes in the skin.
It is also possible that the root cause of the development of pathology may be infections (Coxsackie virus, parvoviruses, HIV, echoviruses, Toxoplasma, Borrelia), malignant neoplasms, and certain medications (statins, penicillamine, phenylbutazone). However, these data are still probabilistic statements and are still being studied.
General information
Dermatomyositis , or in other words, Wagner's disease , is a severe diffuse progressive systemic disease of connective tissue that affects skeletal and smooth muscles, the microcirculatory system of blood vessels, internal organs and skin.
Leads to the replacement of functional structures with fibrous ones. The clinical picture is expressed in the form of motor dysfunction, vasculitis , edema, erythema , hyperkeratosis and may be:
- acute , starting with fever and a memorable development of symptoms, without treatment leads to death after 2-3 months, caused by complete immobilization and severe cardiopulmonary failure;
- subacute - with a gradual increase over several years of muscle weakness, arthralgia , erythema, changes in internal organs;
- chronic - with a benign outcome, having a cyclical course and long-term remissions, characterized by the presence of local atrophic and sclerotic changes in the muscles and skin, and compensated changes occur in the internal organs.
As a result, dermatopolymyositis leads to complications - fibrosis, calcification , atrophy and purulent infections.
Wagner's disease is rare - 2-6 adults and 1-2 children per 100 thousand people. The pathology is more common in countries in southern Europe. The incidence increases in the spring-summer season, which is associated with insolation - more intense exposure to sunlight.
Symptoms
- Heliotropic rash (erymatous spots with a purple tint in the periorbital area, around the eyes) in combination with edema;
- Gottron's papules (nodules and plaques of red and purple color on the interphalangeal and phalangeal joints);
- Gottron's symptoms (erymatous rash with a purple tint, affecting the extensor surface of the elbow and knee joints);
- itching, dryness, peeling on the areas of the skin affected by the rash;
- peeling, cracks on the skin of the fingers and palms on the inside;
- erythema (redness) of the scalp;
- poikiloderma (dystrophic changes in the skin with telangiectasia, areas of atrophy, hypo- and hyperpigmentation);
- photosensitivity;
- hair thinning;
- redness of the periungual fold, growth of skin around the nail bed.
Pathological anatomy
Rice.
1. Microslide of altered skeletal muscle in dermatomyositis: necrosis of muscle cells (1) and inflammatory infiltration (2) are pronounced. In dermatomyositis, autopsy shows generalized damage to skeletal muscles. The muscles are swollen, pale, gray or yellowish-brown, with areas of necrosis, fibrosis and calcification (see). Microscopically morphol. changes in muscles are very variable and depend on the stage and pace of the disease, as well as the age at which the disease arose. There is focal protein degeneration (see) and vacuolar degeneration (see) of myocytes, followed by necrosis and macrophage reaction from the stroma (Fig. 1). The lesions are surrounded by an infiltrate consisting predominantly of small lymphocytes and plasma cells located around the vessels or diffusely between muscle fibers. Subsequently, interstitial fibrosis develops, against the background of which there is an intensification of regenerative processes on the part of myocytes. The intensity of interstitial fibrosis depends on the nature of the course, duration and stage of the disease. Fibrosis is more often observed in acute massive necrosis of muscle cells, which develops when treatment is started late. As a result of the disease, atrophy of muscle fibers develops (see Muscle atrophy), alternating with focal compensatory hypertrophy.
Electron microscopically, with an exacerbation of the process, focal degeneration of muscle cells and the formation of cytoplasmic hyaline bodies are observed.
Thickening of the endothelium and basement membrane of intramuscular arterioles and capillaries is observed. Quite often, virus-like inclusions are found in endothelial cells, reminiscent of those in systemic lupus erythematosus (see).
Foci of necrosis and edema with mucous degeneration (see), as well as fibrosis and calcification are found in the skin and subcutaneous tissue.
Changes similar to changes in skeletal muscles are found in the myocardium, but much less pronounced. Endocarditis and pericarditis are extremely rare. Possible fatty liver. Basically, visceral changes are reduced to moderate inflammatory-sclerosing processes in the stroma, vasculitis (see Vasculitis) and minor damage to the smooth muscles that make up the organs.
With D., changes are noted in the motor terminal nerves and their endings. Dystrophic and regenerative processes are observed in them. There is also a relationship between the severity of changes in muscles and nerve fibers.
For pathomorphol, changes in D. in children are characterized by a predominance of destructive panvasculitis, which is not limited only to muscles or skin, but also extends to the gastrointestinal tract. tract, heart, lungs, peripheral nerves, etc. Intimal hyperplasia and fibrosis of the vascular wall lead to occlusion and hypoxic changes in organs.
Diagnostics
The doctor interviews the patient, conducts a physical examination, collects a complete history of the disease, and gives directions for the necessary studies.
The diagnosis of amyopathic dermatomyositis is established for patients in whom skin lesions characteristic of dermatomyositis are confirmed by biopsy results. However, laboratory and instrumental diagnostic methods did not reveal clinical signs of muscle tissue damage.
Additionally, such patients may be tested for the presence of malignant neoplasms (dermatomyositis is associated with cancer) or interstitial lung disease.
Etiology
Etiology unknown. A number of authors consider dermatomyositis as a sensitization reaction to various antigens (microbial, tumor, etc.). This concept is supported by the wedge, manifestations of the disease, such as erythema nodosum (see Erythema nodosum), urticaria (see), eosinophilia (see), often observed at the onset of the disease. Norton (W. Norton) et al. (1970), Klug and Sonnichsen (N. King, N. Sonnichsen, 1973) discovered virus-like cytoplasmic inclusions in the affected tissues (in the cytoplasm of skin fibroblasts, in the endothelium of capillaries of the skin and muscles, sarcoplasm of muscle fibers) and on this basis consider the possible role of viruses in etiology D.
Treatment of amyopathic dermatomyositis
Treatment of amyopathic dermatomyositis is aimed at controlling skin manifestations. The first line of therapy includes protection from sun exposure (use of sunscreens), as well as the use of topical steroids and antihistamines aimed at reducing erythema and itching. If treatment fails, oral corticosteroids and antihistamines are prescribed.
If there is no positive effect, the patient may be prescribed injections of corticosteroids, antimalarial (hydroxychloroquine) or cytostatic (methotrexate) drugs, immunosuppressants (mycophenolate), and intravenous immunoglobulin.
Patients diagnosed with amyopathic dermatomyositis require constant medical supervision and health monitoring to promptly identify signs of muscle tissue inflammation.
Features and advantages of treatment of amyopathic dermatomyositis at the Rassvet clinic
The Rassvet clinic employs a multidisciplinary team of highly qualified specialists in all areas. All our doctors are well trained and have extensive practical experience necessary to diagnose and treat not only typical diseases, but also rare diseases and syndromes.
Patients with suspected amyopathic dermatomyositis undergo all necessary studies, are prescribed therapy aimed at reducing the symptoms of the disease and improving the patient’s quality of life, and provide maximum support at all stages of treatment.
Pathogenesis
The pathogenetic process begins with a nonspecific effect - hypothermia, excessive solar insolation , vaccination , acute intoxication , trauma and other exogenous factors. It is associated with the presence of infectious agents introduced into the genome of muscle cells, changes in neuroendocrine reactivity or genetic predisposition - the presence of HLA histocompatibility antigens associated with B8 or DR3 .
With dermatomyositis, an immune-inflammatory reaction develops, aimed at the destruction of altered intranuclear structures of muscle and skin cells. Due to cross-reactions, cell populations related to antigens are involved in immune damage. Microphage mechanisms of elimination of immune complexes from the body lead to activation of fibrogenesis and systemic inflammation of small vessels. The hyperreactivity of the immune system is aimed at destroying the intranuclear structure of the virion; it is manifested by the presence in the bloodstream of antibodies Mi2, Jo1, SRP, as well as autoantibodies to nuclear proteins and other soluble antigens.
Clinical picture
There is no generally accepted classification of Dermatomyositis. There are idiopathic, primary, and symptomatic, secondary, Dermatomyositis, which develops in response to tumor antigens, and Dermatomyositis in children.
Secondary dermatomyositis is not fundamentally different from primary dermatomyositis in its clinical picture. According to Williams (R. Williams, 1959), secondary D. is observed in 17% of cases; among patients with D. over 40 years of age, the frequency of secondary D. increases to 50%. D.'s symptoms may precede the manifestations of the tumor by months or even years. Most often, D. is observed in tumors of the lung, prostate, ovary, uterus, mammary gland, and colon. Individual cases of D. have been described in malignant lymphomas, as well as in benign and malignant thymomas. According to the nature of the course, acute, subacute and hron forms D are distinguished. The acute form is characterized by fever with chills, rapidly increasing generalized damage to skeletal muscles, progressive dysphagia (see), dysphonia (see), damage to the heart and other organs. Acute D. is rarely observed in adults. The subacute form has a slower course. The disease most often begins with gradually increasing muscle weakness, the edges are revealed during physical examination. stress (climbing high steps, washing clothes, etc.), less often with the phenomena of dermatitis. Later, damage to the muscles of the shoulder and pelvic girdle intensifies, dysphagia and dysphonia occur. After 1 - 2 years from the onset of the disease, a detailed picture of D. is usually observed with severe damage to the muscles and visceral organs. Chron, the form of D. occurs cyclically, the processes of atrophy and sclerosis of muscles and skin predominate for a long time, isolated muscle groups of the distal extremities (muscles of the forearms, shins) may be involved in the process. Muscle damage is often combined with chronic recurrent dermatitis (see).
rice. 4. Some clinical manifestations of dermatomyositis - periorbital erythema and edema (symptom of “spectacles”), puffiness of the face, bluish-pink coloration of the skin and lips;
Skin lesions in dermatomyositis are polymorphic: erythema (see) and swelling (see) predominate, mainly on exposed parts of the body. Petechial, papular, bullous rashes are observed (see Rash), telangiectasia, foci of pigmentation and depigmentation, hyperkeratosis, etc. Skin, ch. arr. over the affected muscles, swollen, doughy or dense. Erythema is often localized on the face, neck, chest, over the joints, on the outer surface of the forearm and shoulder, on the anterior surface of the thighs and legs; It is highly persistent and is often accompanied by peeling and itching. A peculiar periorbital edema and erythema is characteristic (color Fig. 4) - a symptom of “spectacles”. Trophic disorders, dry skin, longitudinal striations and brittleness of nails, hair loss, etc. are often observed. More than half of the patients have simultaneous damage to the mucous membranes in the form of conjunctivitis (see), stomatitis (see), hyperemia and swelling of the pharynx, as well as vocal folds. Skin syndrome usually precedes the appearance of other signs of D., including muscle damage, but in some patients there are practically no changes in the skin (polymyositis itself).
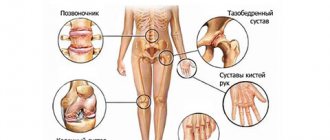
The cardinal sign of D. is damage to skeletal muscles. Typically, the muscles of the proximal limbs, shoulder and pelvic girdle, neck, back, pharynx, upper esophagus, and sphincters are affected. Muscle pain appears, especially with movement and palpation; muscles are dense or doughy, increased in volume. Steadily progressing muscle weakness is expressed in a significant limitation of active movements. Patients cannot stand up, sit down, raise their leg on a step (the “bus” symptom), hold an object in their hand, comb their hair, get dressed (the “shirt” symptom), and fall easily when walking; if the muscles of the neck and back are affected, they cannot lift their head from the pillow or keep it in an upright position (the head falls on the chest); when the facial muscles are damaged, a mask-like appearance of the face appears. At the height of the development of the disease (in acute and subacute cases), patients are almost completely immobilized; movements are preserved only in the hands and feet.
Involvement of the pharyngeal muscles in the process causes dysphagia (choking when swallowing, liquid food pours out through it). Aspiration of food is possible. Damage to the intercostal muscles and diaphragm leads to limited mobility and decreased vital capacity of the lungs (see). When the muscles of the larynx are damaged, a nasal tone of voice and hoarseness appear; damage to the muscles of the eye leads to diplopia (see), ptosis (see); damage to the sphincter muscles leads to disruption of their activity. Then atrophy of the affected muscles or a picture of myositis ossificans develops (see Myositis). Calcinosis in D. is secondary and has a reparative nature. Foci of calcification are most often localized in the most affected muscles of the shoulder and pelvic girdle and in the subcutaneous tissue in the form of plaques or massive deposits. Foci of calcification located superficially can be opened with the release of a lime mass.
The damage to the nervous system noted in D. gave the Senator (H. Senator, 1888) reason to call the disease neurodermatomyositis. Changes are observed mainly in the peripheral and autonomic nervous system; defeat c. n. With. is observed rarely and is expressed in the form of asthenic depressive and asthenic syndromes (see Asthenic syndrome). The EEG reveals pathological rhythms of biopotentials. Some authors note the possibility of developing meningitis and encephalitis with seizures.
Damage to the peripheral nervous system can manifest itself as radicular pain, pain in the nerve trunks, mono- and polyneuritis (see Polyneuritis). With polyneuritis, sensitivity is impaired, especially in the distal parts of the arms and legs. The decrease in sensitivity, like its increase, is not profound. Reflexes are usually reduced, sometimes unevenly. Decreased or lost tendon reflexes may result from combined damage to the muscles and peripheral motor neuron.
Autonomic disorders are varied - a tendency to hypotension, tachycardia, impaired thermoregulation, anorexia, etc.
Almost half of the patients have focal or diffuse myocarditis (see), sometimes with cardiac arrhythmias and symptoms of congestive heart failure. Endocarditis and pericarditis are rare.
Lung damage is manifested by vascular or interstitial pneumonia, resulting in pulmonary fibrosis (see Pneumosclerosis). Isolated cases of the development of pulmonary calcification have been described. Pulmonary failure occurs relatively rarely and is caused mainly by damage to the respiratory muscles and diaphragm.
Damage to smooth muscles went intestinal. tract leads to hypotension of the esophagus and intestines. Some patients experience decreased appetite, abdominal pain, and gastroenterocolitis (see). Gel.-intestinal. bleeding and intestinal perforation in adult patients are rare. Moderate enlargement of the liver is observed in approximately 1/3 of patients.
Cases of severe glomerulonephritis with hypertension and renal failure in D. are very rare, more often kidney damage is manifested by transient proteinuria (see).
Rare symptoms of D. also include generalized lymphadenopathy and enlarged spleen. In some cases, lesions of the fundus vessels have been described.
Of the general symptoms of the disease, the most common is weight loss, sometimes significant (10-20 kg). Febrile temperature is noted during an acute course or exacerbation of D.; in subacute and chronic cases, subfebrile temperature is recorded.
Arthritis is rare. Approximately 25% of patients experience arthralgia (see) and swelling of the periarticular tissues. Joint dysfunction is associated with muscle damage. Sometimes D. is combined with Raynaud's syndrome (see Raynaud's disease).
Laboratory studies in the acute and subacute course of the disease show moderate anemia, neutrophilic leukocytosis, less often leukopenia, eosinophilia), accelerated ROE, increased alpha-2-1 and gamma globulins. An indicator of the severity and prevalence of muscle damage is an increase in the activity of enzymes in the blood - creatine phosphokinase, glutamic and pyruvic transaminases, lactate and malate dehydrogenases, as well as the appearance of creatine in the urine. With hron, during D., changes in laboratory test data are not so clear and pronounced. A number of patients have an increased titer of rheumatoid factor. Antinuclear antibodies and lupus cells are found extremely rarely.
According to Pearson (S. M. Pearson, 1972), an electromyographic study (see Electromyography) reveals a characteristic triad: spontaneous fibrillation and positive potentials of muscle currents; a polyphasic complex of potentials with low amplitude that appears during voluntary muscle contraction, volleys of high-frequency action potentials (“pseudomyotonia”) after mechanical irritation of muscles.
Complications
The most common and dangerous complication, which ranks first among the causes of death in acute dermatomyositis, is severe aspiration pneumonia (see), which develops as a result of aspiration of food masses with impaired swallowing. Constant hypoventilation of the lungs (see Pulmonary ventilation) due to damage to the intercostal muscles and diaphragm creates the preconditions for the development of bacterial pneumonia. In some cases, severe damage to the respiratory muscles with a sharp limitation of chest excursion can lead to increasing respiratory failure (see) and asphyxia (see). In immobilized patients, trophic ulcers (see), bedsores (see) may occur. Possible development of exhaustion. Heart and kidney failure in D. are relatively rare.