Bacterial vaginosis - first symptoms and treatment regimen
Bacterial vaginosis (gardnerellosis, vaginal dysbiosis, vaginal dysbiosis) is a common disease in women associated with a disruption of the normal microflora of the vagina and an increase in the number of other microbes, including gardnerella.
The nature of the disease depends on many factors, so when your health improves, the symptoms completely disappear. The disease is not sexually transmitted and does not affect men. Unprotected sexual intercourse has a certain role in the occurrence of the disease. Frequent changes of partners contribute to changes in the vaginal microflora.
Causes
To date, science does not fully have information about what actually provokes the development of non-inflammatory syndrome. However, the relevance of this problem is increasing every year.
Factors that provoke the development of the disease include:
- weakening of local and general immunity;
- poor nutrition;
- long-term antibacterial and hormonal therapy;
- frequent douching;
- the use of local contraceptives (condoms, creams and suppositories) that contain 9-nonoxynol;
- frequent change of sexual partners;
- wearing synthetic underwear;
- endocrine and gynecological pathologies;
- failure to comply with basic rules of personal hygiene;
- intestinal diseases.
Currently, bacterial vaginosis is one of the most common diseases among women of active reproductive age (from 23 to 33 years). According to statistics, about 30-35% of women suffer from vaginosis, but only half of the total number of patients know about their problem due to the presence of a characteristic odor. The rest, as a rule, don’t even know about it.
Main risk factors:
- Change of sexual partner;
- Having more than one partner;
- Sexual contact woman to woman;
In the first three cases, the main factor in the development of bacterial vaginosis is the mixing of microflora.
- Tight synthetic underwear;
- Douching and foreign bodies in the vagina (intrauterine devices, uterine caps, abuse of tampons);
- Hormonal imbalance;
- Conditions after abortions and other surgical interventions in the pelvic area;
- Pregnancy;
- Menopause;
- Condition after childbirth;
- Condition after menarche in pubertal girls;
- Systematic intake of hormonal, antibacterial and other drugs;
- Stressful conditions;
- Decreased local immunity.
Symptoms
Often the only symptom of bacterial vaginosis is the presence of copious vaginal discharge with an unpleasant smell of stale fish, which can bother you for a long time. At the beginning of the disease, the discharge is thin, white or grayish.
The general symptoms of bacterial vaginosis are as follows:
- discharge with an unpleasant odor (fishy), which occurs as a result of the breakdown of amines produced by anaerobic bacteria.
- copious, homogeneous, creamy vaginal discharge of a grayish-white color, adhering to the walls of the vagina.
- sometimes vulvovaginal irritation appears in the form of itching and burning, discomfort during sexual intercourse.
- signs of vaginal inflammation (addition of vaginitis) are observed in half of the patients.
- rarely - urination disorders and pain in the perineum.
If the disease continues for a long time, more than 2 years, then the following symptoms occur:
- the color of the discharge becomes dark green;
- leucorrhoea changes its consistency, becomes more viscous or resembles a curdled mass;
- Also, the following signs are characteristic of discharge due to vaginal dysbacteriosis: over time they become thick and sticky, and their distribution along the vaginal walls is even. Leucorrhoea is easily removed from the walls with a cotton swab;
- with a long-term process, a number of patients complain of minor or moderate itching/burning in the vulva area (see vaginal itching);
- pain during sexual intercourse (see pain during intercourse);
- the volume of vaginal discharge reaches 0.02 liters per day (taking into account that the normal amount of leucorrhoea is no more than 2 - 4 ml);
- in a number of situations, pathogenic flora joins the described infectious process, which contributes to the development of vaginitis;
- Sometimes urinary disorders occur (frequent and painful urination in women).
A distinctive feature of the disease is the absence of visible signs of inflammation. That is, upon visual examination, a physiological pink color of the vaginal mucosa is observed. Only in some cases, single reddish dots are observed in menopausal women.
Triad: intestines, vagina, urinary system.
It is important to understand that the vagina is closely connected with the organs that surround it. These are the intestines and urinary system. This means that in addition to vaginal mucus, plasma part of the blood, cells covering the vagina, bacteria and microorganisms that live inside the vagina, it can also normally contain bacteria of the intestinal group.
The intestines and urethra are not completely isolated from the vagina, and during the circulation of blood and lymph, the migration and transfer of all kinds of microorganisms occurs, this is normal, there is nothing to worry about.
The main danger lies in intestinal dysfunction. For example, if there is a violation of nutrition and normal bowel movements (constipation or diarrhea), the vagina can react very sharply, because at this moment the growth of opportunistic bacteria can be observed and discharge and discomfort may appear.
There may also be a reverse reaction, with genital infections, when there is a pronounced inflammatory process, in turn, the urinary system suffers and intestinal function is disrupted.
It is important to understand that the vagina is only an accumulating reservoir, therefore, with frequent relapses of bacterial vaginosis and poor effectiveness of treatment, intestinal microflora should be diagnosed.
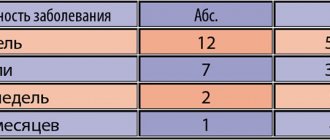
Severity
According to the severity of vaginal dysbiosis, there are:
| Compensated or 1st degree | there is no microflora in the smear, epithelial cells are present without changes and the possibility of infection with other pathogenic microorganisms remains. |
| Subcompensated or 2nd degree | the content of Doderlein bacilli decreases, gram-negative and gram-positive flora increases, there are from 1 to 5 “key” cells, a slight increase in leukocytes - up to 15 - 25. |
| Decompensated or 3rd degree | there are no lactic acid bacteria, there is a clinical picture of the disease, “key” cells entirely, various pathogenic and facultative or conditionally pathogenic microorganisms. |
According to the flow, acute, torpid or erased and asymptomatic vaginal dysbiosis is distinguished.
Diagnostics
A preliminary diagnosis of bacterial vaginosis can be made already during a gynecological examination. After the examination, discharge is taken from the posterior inferior vaginal vault.
The diagnosis can be made if 3 of the 4 listed signs are present:
- specific nature of the discharge;
- acidity >4.5 (normal 3.8-4.5);
- positive amino test;
- presence of “key” cells. The so-called “key cells” are mature epithelial cells (the superficial layer of the vaginal epithelium), on the entire surface of which microbes are densely and in large numbers attached.
Completing one of the 4 tests is not sufficient to make a diagnosis.
How to treat bacterial vaginosis?
Initially, a woman is prescribed antibiotics to treat bacterial vaginosis: they have a detrimental effect on nonspecific bacteria and clear the vaginal mucosa of them.
The drugs of choice are Metronidazole, Tinidazole, Clindamycin, as they are active against anaerobes. Local use of antibiotics is preferable to avoid systemic side effects, but in some cases the gynecologist is forced to resort to tablet forms.
The treatment regimen is selected individually:
- Tinidazole 2.0 in tablet form is taken orally 1 time per day for 3 days;
- Metronidazole in the form of a 0.75% gel is administered into the vagina once a day for 5 days;
- Clindamycin suppositories 100 mg are administered into the vagina once a day for 3 days;
- A cream containing 2% Clindamycin is injected into the vagina once a day for 7 days;
- Metronidazole 2.0 tablets are taken orally once.
During antibacterial therapy and a day after its completion, it is necessary to avoid drinking alcohol, even in minimal doses. The drugs disrupt the metabolism of ethyl alcohol in the body, which causes the accumulation of toxic metabolites and severe intoxication. In its course, it resembles a severe hangover: the woman experiences severe weakness, limbs shake, blood pressure rises, a severe throbbing headache occurs, and painful nausea and vomiting develop.
Clindamycin cream contains fat, so it can damage the condom or latex contraceptive membrane. All local forms of drugs are administered immediately before bedtime to prevent them from flowing down the vaginal walls.
If antibiotics are intolerant or there are contraindications to their use, the first stage of treatment is carried out with local antiseptics:
- Hexicon 1 suppository is administered 2 times a day for 7-10 days;
- Miramistin in the form of a solution is irrigated into the vagina once a day for 7 days.
Preparations for bacterial vaginosis, used in the second stage of treatment, contain lactobacilli and create favorable conditions for restoring the vaginal microflora. They are used 2-3 days after completion of antibacterial therapy:
- Acylact 1 suppository 2 times a day is inserted into the vagina for 5-10 days;
- Bifiliz 5 doses are taken orally 2 times a day for 5-10 days.
Antifungal suppositories for bacterial vaginosis are usually not prescribed. The need for them arises if candidiasis, a fungal infection, joins the opportunistic microflora. In this case, Clotrimazole suppositories are prescribed intravaginally once a day for 6 days.
Vaginal dysbiosis and sexual partner
Most often, a violation of the vaginal microflora in a woman does not cause any problems for her sexual partner, even with regular sexual activity without the use of contraception. In some cases, when there is severe vaginal dysbiosis, a man may develop the phenomena of balanoposthitis and nonspecific urethritis. But this usually only happens if the man already had a predisposition to these diseases; they will not develop in a completely healthy body.
No disease of the sexual partner, with the exception of sexually transmitted diseases, has an effect on the vaginal microflora in a woman. Treatment of vaginal dysbiosis in women does not require mandatory treatment of the sexual partner, unless at least one of them is diagnosed with a sexually transmitted infection.
Treatment during pregnancy
How to treat bacterial vaginosis in case of pregnancy? In the first trimester of gestation, systemic therapy for the disease is not performed (metronidazole and other drugs are toxic to the embryo). Local administration of etiotropic drugs in the early stages is used with caution.
Taking metronidazole or clindamycin begins in the second trimester and is carried out in short courses. Metronidazole 0.5 g. (2 tablets) twice a day for 3–5 days, and clindamycin is prescribed in a dosage of 0.3 g. 2 times a day for 5 days.
Pregnancy complications that may occur due to the disease include:
- miscarriage - loss of a fetus during the first 23 weeks;
- premature birth - when a baby is born before the 37th week of pregnancy;
- chorioamnionitis - infection of the chorion and amnion membranes (the membranes that make up the fetal sac) and amniotic fluid (the fluid surrounding the fetus);
- premature rupture of the amniotic sac - a bladder containing fluid in which the fetus develops;
- postpartum endometritis - infection and inflammation of the uterine tissue after childbirth.
If you are pregnant and experience symptoms of vaginosis, contact your gynecologist as soon as possible. Although the risk of complications is low, treatment will help reduce it further.
Vaginal dysbiosis in girls
Disorders of the vaginal microflora occur in girls who have not begun sexual activity with approximately the same frequency as in women who are sexually active. This is due to several other factors - hormonal instability, the formation of a cycle, as well as the anatomical features of the structure of the hymen.
Vaginal dysbiosis in girls rarely manifests itself as heavy discharge, since the openings of the hymen, as a rule, do not allow them to be removed from the vagina in the quantity in which they are formed. Therefore, stagnation of vaginal discharge develops, and the likelihood of developing inflammatory diseases in virgins is higher. On the other hand, when sexual activity begins with the first sexual intercourse, a large number of bacteria are thrown from the vagina into the bladder, and this can lead to the so-called “honeymoon cystitis”.
Treatment of vaginal dysbiosis in virgin girls is somewhat difficult due to the fact that the structure of the hymen does not always allow for proper treatment of the vagina with medications. In some cases, it is even necessary to resort to artificial disruption of the integrity of the hymen - hymenectomy.
At SM-Clinic, gynecologists, after conducting examinations and tests, will identify the exact causes of vaginal dysbiosis and prescribe effective comprehensive treatment that will lead to the restoration of normal vaginal microflora.
Prevention
The recommendations are as follows:
- using barrier methods of contraception, wearing underwear only made from natural fabrics;
- regular examination by a gynecologist and timely treatment of diseases;
- treatment of chronic pathologies of internal organs;
- strengthening the immune system in natural ways: physical activity, hardening, etc.;
- avoiding douching and other similar procedures.
Bacterial vaginosis is a pathology that reflects a decrease in the body’s level of defense at the moment. Often occurring asymptomatically, gardnerellosis is always detected during examination by a gynecologist. Only a doctor can prescribe the most effective tablets for bacterial vaginosis, suppositories or other forms. Don't delay treatment!