- Squamous cell carcinoma
- Diagnostics
- Treatment of squamous cell carcinoma
- Melanomas of the anal canal
- Nonepithelial malignant tumors of the anal canal
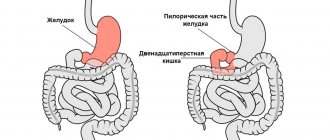
The anus (anal canal) is the end section of the large intestine and digestive tract. The anal canal is distinguished as an independent section of the digestive tract, due to the peculiarities of the anatomical structure and specific functions, the most important of which is the retention of feces and gases.
The length of the anal canal varies depending on the individual characteristics and physiological state of the anal sphincters, gender, age, weight and height of the patients and averages 3-4 cm. Despite the small size of the anal canal, malignant tumors arising in it have a wide variety of histological structure. Tumors of the anal canal are a relatively rare disease and their frequency is 1-6% of all malignant tumors of the rectum.
In the clinical classification of patients with anal tumors, a system is used that evaluates the presence of a primary tumor and its size, the presence or absence of lymph node involvement and distant metastases.
Depending on the spread of the tumor process, the stage of the disease is specified - from 0 to IV, which is important for planning treatment and determining the prognosis (outcome) of the disease.
What is anal cancer?
Cancer is a disease in which normal cells in the human body, through a series of genetic changes, lose the ability to control their growth.
When malignant growth occurs, they invade surrounding tissues (local invasion) and also spread to other areas of the body through blood vessels or lymphatics, where they can take root and grow (metastatic foci). The anal canal is a section of the gastrointestinal tract that connects the rectum to the external environment. The anal canal is surrounded by muscles that keep it closed, preventing intestinal contents from escaping during bowel movements.
Anal cancer arises from cells of the perianal skin or anal canal and is called squamous cell cancer. Malignant cells that do not spread deep into the skin are called high-grade dysplasia, "carcinoma in situ" or Bowen's disease.
Changes in sensation: orgasm and ejaculation with cancer
After cancer treatment is completed, in most cases the sensitivity of the penis is not lost and the patient is still able to experience orgasm, but the sensations may differ from pre-operative sensations. Some men may lose the ability to achieve orgasm, especially if hormone therapy was chosen as a treatment option.
- For example, if a patient has had a radical prostatectomy, he will no longer be able to ejaculate during orgasm. This is because the prostate and seminal vesicles, which are responsible for producing seminal fluid, are removed during surgery. Instead, the patient will experience a “dry” orgasm, in which he feels the orgasm coming but does not ejaculate. Sometimes during orgasm, a small amount of fluid may be released from the tip of the penis. This may be fluid from the glands lining the urethra.
- If the patient has undergone radiotherapy, brachotherapy, ultrasound or hormonal therapy, the amount of sperm produced may decrease. During or after radiotherapy, brachotherapy, ultrasound therapy, the patient may also notice blood in the semen. This is a common occurrence and should not cause concern, but the patient should still report it to their doctor. Some men who have undergone hormonal therapy note that the sensations during orgasm are somewhat dulled.
- If the patient has undergone transurethral resection of the prostate or radiation therapy, he may experience retrograde ejaculation. This means that during orgasm, sperm goes back into the bladder rather than exiting through the penis. Later, sperm is eliminated from the body through urination. It is safe and does not affect the pleasure of sex, but the sensations may be very different from those that the patient previously experienced.
After and during treatment, some men leak urine during orgasm or experience pain. Others note that the duration of sex decreases and they reach orgasm faster.
Who is at risk?
Anal cancer is usually associated with human papillomavirus (HPV). HPV causes warts around the anal canal and on the cervix in women. Having HPV is associated with a high risk of developing cervical cancer in women.
A risk factor is any factor that increases the likelihood of an individual developing a disease. In addition to human papillomavirus, other risk factors are:
- age – most people with anal cancer are over 50 years old;
- anal sex – persons who engage in anal sex have a high risk of disease;
- smoking – harmful chemical components of smoke increase the risk of developing most cancers, including anal cancer;
- decreased immunity – people with weakened immune systems, transplant patients, those taking immunosuppressive drugs and patients with HIV are at high risk;
- chronic foci of inflammation - people with long-term anal fistulas or open wounds have a slightly increased risk;
- pelvic irradiation – patients undergoing radiation therapy for cancer of the rectum, prostate, bladder, and cervix are at high risk.
Diagnostic methods
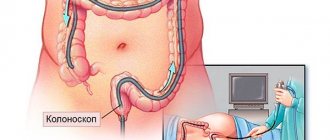
If anal cancer is suspected, the doctor conducts an examination, a digital examination, and then an endoscopic examination: anoscopy or sigmoidoscopy. If a pathological formation is detected on the mucous membrane, the doctor will perform a biopsy: remove a fragment of suspicious tissue and send it to the laboratory for histological and cytological examination.
To assess the stage of cancer, additional diagnostic methods are used: ultrasound, MRI, CT, PET scan, chest x-ray (to look for metastases in the lungs). Is it possible to detect anal cancer at an early stage? There are screening studies, but they are recommended only for people at high risk:
- with precancerous changes in the anus;
- in homosexuals;
- for anal warts (HPV);
- in women who have had cancer of the vulva, cervix;
- in HIV-infected people and after organ transplantation.
Digital examination of the rectum and cytological analysis help to detect a malignant tumor in the early stages. Sometimes a tumor is discovered by chance when the patient was initially treated for hemorrhoids. Anal cancer rarely metastasizes, and most often it can be successfully treated.
Diagnosis of anal cancer
The development of some forms of cancer can be completely prevented. The risk of developing cancer can be significantly reduced by reducing risk factors and conducting regular examinations.
Unprotected anal sex and infections associated with HPV and HIV should be avoided.
Condoms must be used during any sexual intercourse. Condoms do not completely eliminate the risk of infection, but they significantly reduce it. Quitting smoking reduces the risk of developing many forms of cancer, including anal cancer.
People who are at risk may undergo screening examinations. Diagnosis of anal cancer includes a PAP test (smear) and anoscopy. An anal PAP test is a type of test used to screen women with cervical cancer. A smear is taken from the anal canal with a special brush and the resulting cells are examined under a microscope. Anoscopy is an examination of the anal canal using a special medical instrument (anoscope), which allows the doctor to visually assess the condition of the walls of the anal canal. Every patient with an abnormal PAP test should undergo anal examination using anoscopy.
Patients at high risk of developing the disease should talk to their doctor about the need for screening. The risk group includes HIV-infected people, homosexuals, people with multiple sexual partners and women with a history of polyps or precancerous changes in the cervix.
Prostate and rectal cancer
According to the chief urologist of the Russian Federation, Doctor of Medical Sciences, Professor, Academician of the Russian Academy of Sciences Dmitry Yuryevich Pushkar, “every seventh man in the world suffers from prostate cancer.” In Russia, the incidence of prostate cancer is 12.9% of the total male population, the mortality rate is 7.4%:
- from 60 to 70 years of age, the percentage of patients diagnosed with prostate cancer is 6.1%;
- from age 71 the figure increases to 13%2.
Colon cancer, according to statistics, is noted in 5.9% of cases in men. When diagnosed early, this type of cancer has a 90% survival rate.
People diagnosed with cancer feel that life revolves around medical research, treatment, and doctor's appointments, and everything else becomes less important. Studies have shown that after a cancer diagnosis, problems with sexual function fade into the background or are ignored by the patient or his doctor. Sexual function is overlooked due to a frightening diagnosis. When the prospects become clear and the treatment bears fruit, sexual desire returns, but restoring sex after cancer can be complicated.
Symptoms of anal cancer
In most cases, early detection of anal cancer is possible. Anal cancer is localized in that part of the digestive tract where the doctor can easily see it and identify it during examination. Anal cancer is often accompanied by the following symptoms:
- bleeding from the rectum and anus;
- sensation of a foreign body in the anal canal;
- pain in the anus;
- constant or periodic itching;
- bowel disturbances (increase or decrease in the number of bowel movements) or the need to strain during bowel movements;
- ribbon stool;
- discharge (mucous or purulent) from the anus;
- enlarged lymph nodes (glands) in the perianal and inguinal areas.
It should be noted that these symptoms may be the result of less serious diseases, such as hemorrhoids, but only a doctor's examination can remove or confirm the diagnosis. If you experience any of these symptoms, contact a coloproctologist.
Classification of anal cancer
Anal cancer has several histological forms, this is due to the variety of types of epithelium (transitional, stratified squamous, glandular in the anal glands and cylindrical in the rectum) that covers the anal area.
- The most common form of epidermoid (squamous cell) cancer of the anus (55% of cases), this form develops from the outer tissues of the anal canal, distal to the rectal-anal line. A feature of this form is a predisposition to ulceration in the future.
- In the zone of transition of the epithelium from cylindrical to flat, proximal to the rectal-anal line, cloacogenic (basaloid) cancer of the anus is usually found (about 30% of cases).
- Adenocarcinoma (adenogenic cancer) develops from the cells of the glandular epithelium of the anal glands.
- Mucoepidermal carcinoma is an example of combined glandular-squamous cell carcinoma of the anus.
- The dark color of the tumor may indicate its origin from the skin and mucous membrane; such a tumor is classified as melanoma.
The following stages of anal cancer are identified: 0, I, II, IIIА, IIIВ, IV. In the most severe stage IV of cancer, metastases are usually observed in various organs and lymph nodes; as a rule, this process is irreversible and very rarely treatable.
Treatment of anal cancer
Treatment for most anal cancer cases is quite effective. There are 3 main types of treatment for anal cancer:
- surgical – surgery to remove the tumor;
- Radiation therapy – high doses of X-rays kill cancer cells;
- Chemotherapy – drugs are taken that kill cancer cells.
Combination treatment, including chemoradiotherapy, is currently the standard treatment for most anal tumors. Rarely, very small or early detected tumors can be removed surgically (local excision) with minimal damage to the obturator muscles (anal sphincter).
Survival prognosis
Anal cancer has a fairly high five-year survival rate. If treatment is started at the first stage, 71-77% of patients remain alive within 5 years, at the second stage - 59-67%, at the third - 35-58%. Metastases are rarely detected, but if they are present, the prognosis worsens sharply. This type of cancer is difficult to treat. The five-year survival rate for such patients is 7–15%.
| More information about treatment at Euroonco: | |
| Proctologist-oncologist | 5100 rub. |
| Chemotherapy appointment | 6900 rub. |
| Emergency oncology care | from 11000 rub. |
| Palliative care in Moscow | from 40200 per day |
| Radiologist consultation | 10500 rub. |
Book a consultation 24 hours a day
+7+7+78
What happens after treatment for anal cancer?
Carrying out follow-up (monitoring) is very important to assess the result of treatment and exclude relapse of the disease. Treatment for most carcinomas is quite effective. In addition, many recurrent tumors can be effectively treated if detected early. Regular and thorough examination by experienced specialists is the most important monitoring tool. If necessary, additional examinations may be prescribed. If any symptoms or problems appear, you should immediately report them to your coloproctologist.
Causes of erectile dysfunction
Erectile dysfunction can occur due to:
- worries about the cancer diagnosis and the prospects of difficult/ineffective treatment;
- pain, fatigue, weakness due to illness or treatment;
- wrong diet,
- progressive prostate adenoma,
- environmental conditions, contact with cadmium (rubber production, welding work),
- heredity,
- age.
The appearance of erectile dysfunction is more often observed against the background of two types of diagnosed cancer: prostate cancer and colorectal cancer (rectal cancer). Treatment for these types of cancer also causes erectile dysfunction and occurs most often in men 50 years of age and older.
Cancer and Fertility
It is important to understand that cancer treatment can affect fertility: after treatment, reproductive function may be impaired and, in some cases, lost. Russian surgeons performing radical prostatectomy operations recommend that patients freeze sperm before treatment to ensure the opportunity to have children after treatment ends. When frozen, sperm can be stored for 10 years, and sometimes longer.
It is not known for certain whether radiotherapy, brachytherapy or chemotherapy has any effect on the health of potential children conceived during the treatment period. However, couples are still advised to use contraceptive methods during and one year after therapy3.
Treatment: chemotherapy, radiation therapy, recovery
The main treatment for anal cancer is chemotherapy and radiation therapy. In the early stages, minimally invasive operations are possible. In this case, the tumor is removed within healthy tissue (1 cm from the edges) while preserving the function of the rectal sphincters.
To monitor the success of treatment, the removed fragment is subjected to histological examination under a microscope. If no cancer cells are found at its edges, this will mean that the ablastic rule has been met. The tumor was completely removed and the risk of its recurrence was minimized.
When choosing a surgical treatment plan, two factors are taken into account:
- The need for complete removal of carcinoma and all identified metastases.
- Preservation of the locking function of the rectal sphincters and the possibility of normal bowel movements.
As a rule, surgical operations are performed in the later stages of anal cancer, when the disease recurs.
Radical surgery means removal of the anal canal, extirpation of the rectum, excision of regional lymph nodes, removal of part of the anus and colostomy. Such surgical interventions are resorted to only in the most extreme cases.
A colostomy means the large intestine is brought out in the lower abdomen. Defecation occurs without the participation of the anal canal, which is removed and sutured. This option has to be resorted to in 25-40% of cases of anal cancer. As a rule, this is explained by late diagnosis.
At an early stage of the disease, it is possible to remove the tumor using the least invasive method, in particular with a laser. The decision to undergo surgery is made based on the results of chemoradiotherapy.
Squamous cell carcinoma of the anal canal is sensitive to ionizing radiation and chemotherapy, but the results of such treatment can usually be assessed only after 26 to 29 weeks.
Therefore, at least six months usually elapse between chemoradiotherapy and surgery (if necessary). This is a feature of anal cancer. His response to chemoradiotherapy can be accurately assessed not after 11 weeks, as in other cases, but after a much longer time.
For the effectiveness of radiation therapy, the targeting of the effect, and therefore the accuracy of diagnosis, is important. If the effectiveness of external radiation sources is unsatisfactory, brachytherapy is used. A miniature radiation source is placed inside the anal canal close to the tumor. Thus, the most targeted, local effect is achieved without damaging surrounding tissues. Starting from the 2nd stage of anal canal cancer, radiation irradiation of the inguinal lymph nodes is performed due to the high risk of their damage by metastases.
Chemotherapy for anal cancer is used in the form of a course of treatment using several drugs. It can be done before surgery (along with radiation therapy) to reduce the size of the tumor, after surgery (to reduce the risk of recurrence), or as an alternative to surgery.
Anal cancer has the peculiarity that it provides relatively greater opportunities for the use of conservative agents. Whereas in the treatment of malignant tumors of other localizations, surgical treatment is usually the main method.
Questions for the doctor
When choosing a treatment method, the patient should ask some questions to his doctor. We have prepared a checklist that will help you get all the necessary information:
- Is sex possible with cancer, are there any contraindications in my case?
- How can treatment for prostate/colorectal cancer affect my sex life?
- How soon after treatment can I return to sexual activity?
- What remedies are right for me to avoid erection problems as much as possible?
- How can I prepare for treatment for prostate/colorectal cancer?
- What happens if the treatment doesn't work? Are there any alternative treatments?
- What information resources can I use?
- Will I need psychological support?
- Will my partner need support?
- What experience do you have in performing such operations, and what are the statistics of successful restoration of erectile function among your patients?
Sexual compatibility of Cancer Woman with other signs
She is Cancer, He is Aries.
The dynamic nature of Aries, striving for self-affirmation, encounters a blank wall of opposition from Rakini with her jealousy and desire to “tie” him to herself. The union can only last if both Aries and Cancer are atypical.
She is Cancer, He is Taurus.
A typical and frequently occurring conjunction. Partners drag everything into their nest. The union is strong, with prosperity. Family is the embodiment of patriarchal comfort.
She is Cancer, He is Gemini.
Despite the seeming unthinkability of the union, this marriage is very typical. He relies on constant deception and self-deception. This is a union of very different souls.
She is Cancer, He is Leo.
The union is difficult for Leo. A real Leo will rarely be carried away by the Rakinya, but if he is already in her network, then he is lost. In sex, he is dissatisfied with Rakinya and tries to tear off the veil of mystery from her. The Rakina is satisfied with Leo, but the more he pleases her, the more she plays on his nerves.
She is Cancer, He is Virgo.
The union is possible, quite stable and durable, despite the fact that Rakinya gets tired of Virgo’s moralizing. This combination of a sensitive and phlegmatic nature (Cancer) and sobriety (Virgo) is based on mystery and “hide and seek”. Only in Virgo will Rakinya find a partner who will carefully take care of the children and will be very helpful in running the household.
She is Cancer, He is Libra.
The union is difficult, replete with great internal disagreements. The subtle, sensitive Rakin does not tolerate the Libra man who evaluates and balances everything. Libra does not like Rakini's displeasure. She may not show this outwardly, but the invisible crack is still felt. In addition, honest Libra does not like Cancer's deceit.
She is Cancer, He is Scorpio.
A union in which sexual compatibility is almost perfect. Selfish Scorpio will always know how to take advantage of Rakini's weak points. She, in turn, will be afraid of Scorpio. In such a marriage, the spouses quietly and for a long time gnaw at each other.
She is Cancer, He is Sagittarius.
The union is not bad (better than the opposite, when he is Cancer, she is Sagittarius). The Rakin attracts Sagittarius with her softness and spoiled nature. However, she will have lovers on the side and nevertheless tenaciously hold on to Sagittarius. Sagittarius will also deceive her. This marriage can survive on mutual deception for many years, but then it will still fall apart, unless it is strengthened by a community of mutual interests, mercantile ties, and business relationships.
She is Cancer, He is Capricorn.
A frequently occurring, but nevertheless unfavorable alliance for both parties. Each spouse pulls in their own direction. The tension in the relationship does not subside; frequent conflicts create completely unbearable situations. The partners are haunted by mutual misunderstanding, despite the fact that there is sexual attraction between them, which continues even after the divorce.
She is Cancer, He is Aquarius.
The union is difficult. The spouses live in different worlds and are connected, perhaps, only by their children. True, when children are born, a struggle begins for the right to own them, which is why the kids suffer greatly. Despite the mutual misunderstanding of the most basic emotional manifestations, this union can last a long time. Sexual relationships may start out daringly and are accompanied by very strange stories, but subsequently a repulsive force arises equal to the force of the former attraction.
She is Cancer, He is Pisces.
A very common combination. The Rakin is the only one who can not be jealous of Pisces. This is a classic union. Their home is usually a “full cup”; both bring everything into it. This marriage is a peace of mind, a “quiet haven.” Everyone in this family dreams of their own and does not interfere with the other.
Psychological support
American scientists conducted a study on the influence of internal psychological state on improving the effectiveness of cancer treatment. Practice has shown that a positive emotional attitude increases the chances of recovery in stages 2 and 3 by 55%, and in stage 4 by 25%6.
In Russia there are few support groups for patients with prostate cancer. One of them is a support group forum on the Doctor and Me portal. In addition to useful practical advice about living with cancer, forum visitors share problems and personal experiences. Despite the lack of attention to the problem of erectile dysfunction when diagnosed with cancer, treatment can be started after talking with a doctor or nurse.
The patient can also contact the psychological assistance service of the charitable non-profit project Help-Patient.ru. By calling the hotline 8-800-100-01-91 or by email, an experienced specialist will help cancer patients and their relatives when making decisions, provide information and psychological support in difficult life situations, give recommendations on what to do first, and provide the address the nearest oncology facility where medical care can be provided. The organization provides psychological assistance, not medical consultation.
Tips for communicating with your partner
Treatment may affect your sexual desire and erections, this is normal. It is also normal that it can affect your relationship with your partner. Here are some tips to help a couple cope with difficulties:
- Take your partner to doctor's appointments if possible. Having your partner present during the consultation will help him understand your feelings.
- Listen to your partner's experiences. Remember that this problem affects both of you.
- See a therapist/sex therapist to address issues affecting your sex life. Research shows that prostate cancer patients and their partners have improved overall satisfaction with their sex lives after multiple visits12.
- Don't avoid intimacy. If sex is problematic, you can always interact with each other in other ways, such as hugging, kissing, and caressing.
- Boost your self-esteem. After treatment, your appearance may change. To get rid of feelings of inferiority, feel desired in the eyes of your partner, and also increase your own self-esteem, you can work on your appearance (change your clothing style or hairstyle).
- Try not to isolate yourself, talk with your partner about your problems, ways to overcome them, emotions and sexual desires. Communication will help you become closer and feel confident in your abilities.
- Discuss with your partner the possibility of having sex with cancer, explain to him that it is completely safe to have sex with a cancer patient.