Medical editor: Zemereva N.Yu., physiotherapist November, 2020
When one or more joints become inflamed and swollen, and movement in them becomes painful or impossible, we speak of a disease such as arthritis.
The causes of arthritis are varied; depending on the etiological factor, various forms of arthritis are distinguished:
- rheumatoid;
- gouty;
- reactive or inflammatory;
- psoriatic.
Proper nutrition plays a major role in the treatment of joint inflammation and helps alleviate the course of the disease.
The effect of drug therapy for RA on the body
Traditional treatment of rheumatoid arthritis of both types (seropositive and seronegative), in addition to basic drugs that have a delayed effect (at the choice of a rheumatologist, gold drugs, cytostatics, antimalarials, sulfonamides, D-penicillamine), includes painkillers and hormonal drugs, which have many side effects. Proper nutrition is aimed at minimizing the harm caused by medications. On the other hand, the task of a nutritionist when selecting a menu is to ensure that the patient receives the maximum of nutrients and to exclude foods that cause an exacerbation of the pathology (more on this below).
Groups of auxiliary drugs and their effect on the body of a patient with rheumatoid arthritis:
- non-steroidal anti-inflammatory drugs (NSAIDs);
- corticosteroids.
On the left is a stomach ulcer due to long-term use of NSAIDs, on the right is bone loss (osteoporosis) due to long-term hormonal therapy
Nonsteroidal anti-inflammatory drugs (NSAIDs)
Medicines in this group have a negative effect on the mucous membrane of the stomach and intestines, provoking an exacerbation of the patient’s existing gastritis, stomach or duodenal ulcers, or causing their appearance with long-term use. The diet of a patient with RA should include foods (meals) that would protect the gastrointestinal tract from such aggressive effects.
Corticosteroids
Hormonal drugs have a destructive effect on most organs and systems of the human body, especially with long-term use. However, if the patient’s arthritis activity is off the charts, such remedies cannot be avoided. In such a situation, proper and balanced nutrition comes first, helping in a number of cases (increased blood sugar levels, increased blood pressure, irritation of the gastric mucosa up to the appearance of ulcers, increased blood viscosity and increased risk of blood clots, decreased bone density) to minimize the negative impact of treatment.
On a note. Banana is a fruit that can replace most antacids (neutralize the effect of gastric juice). In addition, it contains a lot of potassium and carotene, which is good for the heart, which often suffers from rheumatoid arthritis, as well as other vitamins, macro- and microelements. A couple of bananas a day can, in a fairly short time, regulate blood pressure and sugar levels, improve mood and have a beneficial effect on the stomach. However, if the prothrombin index is high, eating them is not recommended.
Principle 7: Eat with Gratitude
Rheumatoid arthritis, along with bronchial asthma and gastric ulcers, are diseases whose exacerbation can provoke stress and strong negative emotions.
The habit of eating with gratitude allows the patient to neutralize the effects of negative factors, because... In response to positive emotions, the body produces substances that have analgesic and anti-inflammatory properties. And a calm atmosphere promotes eating at a leisurely pace, which is extremely important and necessary for the stomach.
What does the body of a RA patient require?
As a rule, basic therapy for rheumatoid arthritis is aimed at suppressing the patient’s overly strong immune system. Most often, the drug of choice for rheumatologists is Metatrexate. Despite good tolerance by patients and smoothed side effects against the background of a pronounced positive effect, damage is still caused to the body. In such a situation, it must be supported with nutrition - introduced into the diet:
- Diet for rheumatoid arthritis - allowed and prohibited foods, recipes with photos
- ascorbic acid (acts as a hormonal stabilizer, a strong antioxidant);
- bioflavonoids (reduce the permeability of the vascular wall, bind free radicals);
- Niacin (helps the stomach and strengthens blood vessels).
Ascorbic acid or vitamin C is found in Brussels sprouts, broccoli, bell peppers, rose hips, persimmons, sea buckthorn, jacket potatoes, peaches, apricots, fresh green peas, and sauerkraut.
Bioflavonoids of various types are found in the following products: bee propolis, medicinal herbs - tansy, cornflower, knotweed, St. John's wort, immortelle (maximum concentration in juice), berries - blueberries, red grapes (especially the skin), lingonberries, strawberries, blackberries. Green tea is also rich in them.
Niacin (niacin or vitamin B3) can be obtained from tuna, turkey and chicken meat, liver, sunflower seeds, legumes, mushrooms, wheat and buckwheat sprouts, and yeast.
On a note. Even knowing where what nutrients are found, it is difficult to create the right menu on your own. You should not experiment on yourself - seek help from a rheumatologist and nutritionist.
What is prohibited
Some foods may aggravate RA symptoms, causing persistent pain. They need to be excluded from the diet at least for a while until stable remission is achieved.
What not to eat:
- dairy products with a high percentage of fat;
- fat meat;
- spices;
- canned food;
- sweets, including honey (limit to the very minimum; sugar should be avoided altogether);
- alcoholic drinks;
- nuts;
- nightshades - potatoes, eggplants, tomatoes;
- citrus;
- salt (limit as much as possible).
On a note. In case of exacerbation, the products listed above should be completely removed from the diet.
What is allowed
If RA is in the active phase, all foods that could worsen the patient's condition are excluded. There is very little left in the diet that can be eaten without danger:
- chicken and quail eggs;
- skim cheese;
- rice or buckwheat porridge;
- fatty sea fish (salmon, trout, salmon), as a source of omega-3 polyunsaturated fatty acids and vitamin D;
- turkey meat;
- low-fat river fish (pike perch);
- vegetable soups (see list of excluded vegetables);
- barley drink;
- baked apples;
- rosehip decoction;
- greenery;
- 1% kefir;
- herbal or green tea.
On a note. The listed products contain a lot of protein, a minimum of fat and carbohydrates. It is forbidden to fry dishes from them. Stewing in a small amount of oil is allowed, but boiling or steaming is preferable. Salt is completely excluded. It is permissible to add a little salt to prepared dishes.
What do doctors recommend?
Therapeutic diet No. 10 or the Dong diet involves reducing calories (the patient should consume no more than 1800 kcal per day) and completely eliminating red meat. Fast (simple) carbohydrates are removed from the diet as much as possible, the amount of protein is also reduced (but not less than 90 g per day), because in a certain percentage of patients it causes an exacerbation of the condition, the amount of fats, especially animals, is reduced (in total no more than 70 g per day) .
In fact, the Dong diet suggests that for 10 days the patient will eat rice and stewed vegetables with a small addition of chicken or turkey. Not everyone is able to withstand such a meager menu, but to relieve the pain syndrome you will have to make every effort and not break down. In the future, the diet is expanded to include fish meat, rabbit meat, and eggs.
On a note. For rheumatoid arthritis, meals are split - 6 times a day, or more often. The main thing is not to go overboard in calories. If the patient is overweight, such a diet will help get rid of several kilograms without much effort - it is no coincidence that doctors recommend it to obese patients.
Strict diet for RA
An approximate daily menu for a patient with rheumatoid arthritis is as follows (options are possible for the days of the week from allowed products):
- Diet for knee arthritis. What foods are good and what are bad for arthrosis?
- Breakfast: 2 boiled eggs, 2 whole grain breads, 10 grams of butter, herbal tea without sugar.
- Second breakfast: cottage cheese casserole, baked apple, herbal tea.
- Lunch: vegetable soup with buckwheat, 1 standard steamed turkey cutlet with a side dish of boiled rice, vegetable salad of cucumber, lettuce and 1 tbsp. olive oil.
- Afternoon snack: berry pudding or 2-egg omelette, dried fruit compote with a minimum of sugar or fructose.
- Dinner: a palm-sized piece of trout, steamed, a couple of lettuce leaves, a few slices of cucumber, 2 tbsp. boiled rice with a drop of olive oil, zucchini stewed with vegetables (carrots, onions), a cup of green tea.
- Before bed: a glass of low-fat kefir or natural yogurt without additives.
On a note. When creating a menu, always follow your doctor's advice. Although the diet is limited, if you use your imagination, you can prepare many tasty and healthy dishes from the permitted products. After the disease enters the stage of remission, the menu is allowed to expand.
Knowing what kind of food is allowed for rheumatoid arthritis, the patient will always be able to control the condition of his body. When the acute period has passed, consult your doctor about expanding your diet. At this time, you can add fresh herbs, vegetables and fruits (which ones will be advised by a specialist).
We also recommend reading:
Content
Rheumatoid arthritis is a complex autoimmune joint pathology that leads to irreversible joint deformation and loss of motor function. This disease is chronic and cannot be completely cured. However, the correct therapeutic complex, selection of medications, diet and exercises for rheumatoid arthritis can stop the inflammatory process and degenerative destruction of joint tissue, as well as avoid exacerbations of the disease.
Diagnostics
At first, exacerbations appear in the form of minute attacks, and sometimes last for several days. But abnormal changes in the immune system begin to occur long before obvious signs of illness. It is very important not to miss the initial symptoms of the disease and to visit the clinic on time. Patients often ask: their joints hurt, which doctor should they see? If you don’t know which doctor to visit, you can always ask about it at the reception desk or go to an appointment with a therapist who will examine you and give you a referral to the necessary specialists: a neurologist, rheumatologist, orthopedist and surgeon. Timely detection of the disease makes it possible to slow down its development and improve the patient’s quality of life. When visiting a doctor with a patient, the following is carried out:
- a conversation during which complaints, duration and characteristics of the disease are clarified;
- external examination and palpation are performed;
- a complete anamnesis is collected.
After this, the following laboratory tests are performed to diagnose autoimmune arthritis:
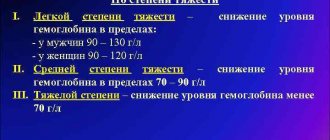
- Clinical blood test - a characteristic feature is an increased erythrocyte sedimentation rate; with the development of the disease, a decrease in hemoglobin occurs.
- Biochemical blood test - nitrogenous waste is detected, the functioning of the liver, pancreas, carbohydrate metabolism is assessed, and blood clotting is checked.
- Blood test for antibodies - their presence and concentration is detected.
- C-reactive protein indicates the development of an inflammatory process.
In addition, to make an accurate diagnosis of autoimmune arthritis, the following hardware tests are prescribed:
- Radiography is one of the important diagnostic methods: determines the presence of damage due to injuries; changes associated with inflammation; joint deformation; bone tissue growth; changes in the joint cavity.
- Ultrasound is often used to identify changes in large joints.
- CT scan – allows you to see the condition of soft tissues.
- MRI is widely used to monitor changes in ligaments, intervertebral discs, and muscle structures.
- Scintigraphy - this method is often used to diagnose arthritis (ICD-10 code M05-M99) and can detect the disease in the early stages.
- Arthroscopy – often used for the knee joint.
- Puncture - performed to take synovial fluid for the purpose of its subsequent study.
After the results of all studies are ready, consultations with specialists are made, an accurate diagnosis is made and appropriate treatment is prescribed.
Dietary goals
The basis of treatment for this type of arthritis is the need to take anti-inflammatory and immunosuppressive drugs, physiotherapeutic procedures and physical therapy. The diet will help strengthen the quality of therapy and prolong the period of symptom relief.
By changing their diet, many patients suffering from rheumatoid joint pathology note a noticeable improvement in their general condition. The main objectives of the diet are:
- Normalization of metabolism and functioning of the gastrointestinal tract. Metabolic abnormalities are not directly related to the development of this type of arthritis, but their presence can lead to excess weight, as well as a lack of beneficial microelements and vitamins. As a result, the joints become less resistant to destruction and are subject to constant pressure due to excess body weight.
- Elimination of symptoms of inflammation. It has been proven that certain foods can increase joint swelling, pain and inflammation. Proper nutrition for rheumatoid arthritis not only reduces pain, eliminates swelling and swelling, but also prevents the development of new exacerbations.
- Enriching the body with calcium and vitamins. In the fight against immune pathology of the joints, it is necessary to pay special attention to strengthening them and restoring the protective function of the body.
Causes of the disease
Inflammation of the joints of the musculoskeletal system is a pressing problem for modern people. Rheumatoid arthritis, which is a type of autoimmune disease, mainly affects people of working age after forty years, and it is five times more common in women than in men. The main causes of joint disease are considered to be:
- Genetic predisposition associated with abnormal chromosome structure. Blood relatives are four times more likely to have rheumatoid arthritis.
- Infections - viral diseases: rubella, herpes, retrovirus, Epstein-Barr. All of them are factors contributing to the development of the inflammatory process in the joints.
- Unfavorable environmental conditions: radioactive radiation, constant exposure to low temperatures, chemical pollution.
- Systematic stressful situations, emotional overload. Autoimmune arthritis in the female half of the population often occurs during pregnancy, after childbirth, abortion, and during menopause.
- Rapid increase in body weight.
- Alcohol and tobacco addiction.
All of the above factors contribute to the development of the inflammatory process, primarily in the cartilage tissue of the joints.
General recommendations
The diet for different forms of arthritis has its own characteristics. This diet involves a balanced diet taking into account the needs of the body in the presence of a certain pathology:
- The diet is prescribed for therapeutic and preventive purposes, therefore general recommendations and nutritional direction are prescribed by a rheumatologist. It is not recommended to choose a diet on your own without the advice of doctors.
- Since rheumatoid arthritis is a chronic pathology, nutritional rules must be followed at all times. During the exacerbation phase, dietary measures will be more strict, while during the period of remission, you can slightly diversify the diet.
- The calorie content of daily food should not exceed 2500 kcal. During periods of exacerbation, this figure drops to 1500–2000 kcal. Meals should be divided into 4-5 times a day in small portions.
- The volume of fluid consumed during the period of remission should not exceed 2 liters of water per day, in the acute form of the disease - no more than 1.5 liters. This is due to an increase in synovial fluid in the lining of the joint, which intensifies the inflammatory process. You also need to take into account the liquid consumed in drinks and food.
- It is necessary to exclude or minimize the consumption of fast carbohydrates, animal proteins and fats. For autoimmune rheumatoid arthritis, the diet should be rich in complex carbohydrates, proteins and fats of plant origin.
- If a patient requires weight loss, fasting and rapid weight loss are strictly prohibited. Losing more than 4 kg per month will lead to serious metabolic disorders.
- Foods that trigger allergies should be identified and avoided. Experts note a direct connection between the allergic reaction and the exacerbation of rheumatoid inflammation. An elimination diet will help you determine the list of allergen foods. You need to make a list of suspected provocateurs and alternately exclude them from the diet for 1–2 weeks, and then introduce them for 1 day. If the appearance of unpleasant symptoms coincides with the consumption of a product, this is an allergen. To be sure, you can do the experiment again.
- It is necessary to limit the consumption of salt, as it retains excess fluid in the body. The daily norm should not exceed 5–8 grams. When calculating the amount of salt consumed, you need to take into account salt-containing foods.
- Attention should also be paid to the methods of preparing food. Eat boiled, baked and steamed foods. It is better to completely exclude fried foods.
Medical myths. All about arthritis
This edition of Medical News Today's Medical Myths celebrates Arthritis Awareness Month and looks at some of the most enduring half-truths and outright prejudices about arthritis. Let's take a closer look at them.
Arthritis is a disease whose main manifestations are pain and inflammation in the joints. There are two main types: osteoarthritis (OA) and rheumatoid arthritis (RA).
Osteoarthritis is the most common form, according to the Centers for Disease Control and Prevention (CDC). The basis for OA is degenerative-dystrophic changes in the cartilaginous structures that are located between the bones in the joint, which is why osteoarthritis is often called “wear-and-tear arthritis” or “depreciation disease.”
Rheumatoid arthritis occurs when the immune system mistakenly attacks healthy tissue in its own body. The result is damage to the joints, but tendons, muscle and connective tissue may also be involved.
Arthritis is quite common. In particular, osteoarthritis is the leading cause of disability in older age groups. The Lancet estimates that this form of joint inflammation affects about 7% of the global population, representing more than 500 million people.
According to the World Health Organization, rheumatoid arthritis is less common, but is still found in 0.3-1% of the global human population. One of the features of RA is the tendency to manifest at an earlier age, compared to OA, usually between 20 and 40 years; In addition, rheumatoid arthritis often has a more severe impact on daily activities. In WHO materials about.
In addition to osteoarthritis and rheumatoid arthritis, there are several other forms of this disease, including:
- juvenile (adolescent) arthritis, a group of joint inflammatory diseases that begin in childhood or adolescence;
— spondyloarthropathy, the collective name for dystrophic lesions of the joints of controversial etiology;
- systemic lupus erythematosus, one of the autoimmune diseases in which many tissues and structures in the body are affected, including joints;
- gout, accumulation and deposition of crystalline salts of uric acid in the joints;
- infectious and reactive arthritis, inflammation of the joints as a result of the activity of pathogenic microorganisms;
- psoriatic arthritis, which affects almost a third of psoriasis patients.
So, about the myths associated with arthritis.
Only old people suffer from arthritis
Arthritis is more common in older age groups, but people of any age get sick. The National Institutes of Health's PubMed Central database provides analysis reports of the National Health Interview Survey, a national health survey developed by the National Center for Health Statistics and regularly conducted by the CDC. According to these data, 49.7% (ie less than half) of all cases of arthritis are diagnosed in people aged 65 years and older. 30.3% of cases occur in the age category of 45-64 years; 7.3% - in the category of 18-44 years, and in other cases (12.7%) arthritis is primarily diagnosed in people under 18 years of age. As for rheumatoid arthritis (RA), this form, as indicated above, most often manifests itself in the age category from 20 to 40 years.
If your joints hurt, it's arthritis.
Not at all necessary. Not all joint pain is caused by arthritis, and any discomfort in the joints should not be considered a sign of inevitably impending arthritis. There are many other causes of joint and periarticular pain, including tendinitis, bursitis, injuries, etc.
Exercise is contraindicated for those suffering from arthritis.
In general, exercise is not a contraindication for arthritis. On the contrary, an individually designed and thought-out gymnastic system helps maintain joint mobility and strengthen them. At the same time, a preliminary consultation with a doctor is an absolute necessity to agree on the nature, intensity and frequency of the expected loads.
From the American College of Rheumatology:
“Exercise can and should be practiced when you have arthritis. Arthritis patients who engage in regular exercise find less pain, more energy, better sleep quality and overall better daily functioning.”
Moreover, this organization recommends that exercise be considered "one of the fundamental principles of treatment of osteoarthritis of the elbows and knees."
Nightshade vegetables worsen arthritis
Nightshades, which include tomatoes, eggplants, potatoes, peppers and some other crops, are the subject of one of the most enduring myths about arthritis. Some people claim that eating these vegetables worsens arthritis symptoms.
For clarification, we turned to Dr. Brian Schultz, a sports medicine specialist and surgeon at the Cedars-Sinai Kerlan-Jobe Institute (Los Angeles, California). He told us: “There is no evidence that nightshade vegetables cause inflammation or worsen arthritis symptoms. However, the Arthritis Foundation recommends certain anti-inflammatory foods, including fatty fish rich in omega-3s, pigmented fruits and vegetables high in antioxidants, nuts, grains and legumes.”
Warmth is better than cold for sore joints
This is wrong. In fact, both heat and cold can relieve joint pain. From materials from Guy's and St Thomas's National Health Service (NHS, UK):
“When used correctly, heat can relieve pain and stiffness in joints and muscles. Cold can reduce joint inflammation and swelling.”
Foundation specialists explain that warming is best used before physical activity or exercise, when the joint is still stiff and movements are painful. But cooling can also help if the joint is inflamed and swollen after activity.
There is no cure for arthritis
This is partly a myth. Of course, not every case of arthritis can be prevented, since some risk factors, such as advanced age, do not depend on the individual and cannot be controlled. However, CDC experts insist that people can eliminate or minimize certain risk factors to effectively prevent arthritis or slow its progression.
In particular, overweight individuals are at increased risk for osteoarthritis of the knee joints. Normalizing and maintaining weight in an adequate range can reduce this risk. Another serious factor contributing to the development of rheumatoid arthritis is tobacco smoking. Quitting this addiction, which is dangerous in so many ways, reduces the risk of joint damage and provides a wide range of other health benefits.
Finally, given the likelihood of developing arthritis after injury, basic joint protection during sports or other types of physical activity significantly reduces the risk of arthritis manifesting in later life.
Once you have been diagnosed, you are powerless to do anything.
Fortunately, this is a myth. Despite the fact that there is often no etiopathogenetic treatment for the disease, its course varies depending on the type of arthritis. Today, medications are available that effectively reduce clinical manifestations and inhibit the progression of changes in many types of arthritis.
And it is worth emphasizing once again that even after establishing and confirming the diagnosis, it is quite possible (and necessary) to adopt a lifestyle that in itself serves as an obstacle to a further increase in symptoms: eliminate smoking, achieve a normal body weight, switch to a healthy diet and ensure you get enough sleep.
Glucosamine and chondroitin may treat arthritis
As a rule, arthritis is not amenable to etiopathogenetic treatment; this means that to date there is no therapy that would eliminate the causes and restore the affected joints to their original state.
Supplements with a high content of glucosamine and chondroitin (important natural components of synovial fluid and cartilage tissue. - Note by Lakhta Clinic ) can only alleviate the symptoms to some extent in some patients with osteoarthritis. Such additives are widely represented on the market and are in certain demand.
We asked Dr. Orrin Traum, a rheumatologist at Providence Saint John's Health Center in Santa Monica, California, for clarification on the origins of this myth. Here's what he says: “The Arthritis Cure, published by Dr. Jason Theodosakis, has become a best seller. There, in particular, treatment with glucosamine and chondroitin sulfate is promoted, but to this day these claims remain unfounded.”
(The book in question, which called glucosamine and chondroitin sulfate therapy "a medical miracle that can stop, reverse and even cure osteoarthritis," was first published in 1997 by a team of authors; the other two besides Theodosakis were Brenda Adderley and Barry Fox. - Approx. Lakhta Clinics ).
Many studies have been undertaken on the therapeutic efficacy of these substances, both individually and in combination. But there are no clear answers. For example, a large study under the auspices of the National Institutes of Health was carried out in 2008; The effectiveness of glucosamine and chondroitin against pain in osteoarthritis of the knee joint was studied. The comparator drugs were celecoxib (a non-steroidal anti-inflammatory drug available by prescription to relieve OA pain) and placebo. In this study, only celecoxib was significantly more effective than a placebo dummy, while “the effectiveness of the other drugs tested was not significantly different from placebo.” And yet the authors considered it necessary. However, this did not affect the general conclusions, since this subgroup turned out to be too small.
According to the National Center for Complementary and Integrative Health:
“Results of the study show that chondroitin is not effective against pain in osteoarthritis of the knee or hip. […]. It remains unclear whether glucosamine helps relieve pain in osteoarthritis of the knee, or whether similar supplements can reduce pain in other joints.”
Dr. Traum concludes: “It is possible that a small proportion of patients suffering from osteoarthritis pain may benefit from the combination of glucosamine and chondroitin. Because such supplements do not show significant side effects, clinical trials could provide clarity for those patients who avoid taking stronger traditional drugs."
Dr. B. Schultz agrees with this formulation of the question, emphasizing: “Some studies confirm the effectiveness, others refute it, but overall these supplements are relatively safe to take, and I usually recommend that my patients try them in order to evaluate the effectiveness in their own particular case.”
Changes in weather can worsen arthritis symptoms
There is a persistent belief that the symptoms of arthritis worsen in rainy and damp weather. We will finish our review on this topic.
Despite the fact that statements about the influence of weather on the course of arthritis sound quite mythical, they still find some confirmation. However, the available data are spotty and sporadic, and this is completely insufficient to draw general conclusions.
We asked Dr. John Tibery, Brian Schultz's colleague at the Cedars-Sinai Kerlan-Jobe Institute and an orthopedic surgeon who specializes in joint replacement and preservation. This is what he replied:
“There is no specific and sufficiently convincing scientific explanation for the phenomenon of the influence of weather on the arthritis clinic. There are several theories based on complaints from individual patients - those who insist that symptoms depend on changes in weather."
Dr. O. Traum supports this point of view: “Many of my patients say something similar when it is about to rain or when the weather is simply expected to change. Sometimes I even find that these complaints are more reliable than the weather forecast. Patients with inflammatory arthritis or swollen joints may often experience changes in barometric pressure, usually on the day before a weather change.”
The true mechanisms behind the dependence of arthritis symptoms on weather are unclear, but it appears that this dependence does occur—to some extent. Dr. Schultz mentions, in particular, the theory that "lower temperatures affect the degree of viscosity of intra-articular fluid, which can lead to greater joint stiffness."
What to take note
The last of the “myths” we examined especially eloquently suggests that, despite the prevalence of arthritis, we still have a lot to explore and clarify about this disease.
However, today there is no doubt that a healthy lifestyle, including a balanced diet and regular exercise, can dramatically reduce the risk of at least some types of arthritis or slow down their development, if it cannot be avoided.
As scientists advance research into this disease, so do therapeutic approaches. It is likely that someday we will even find an answer to the question of how weather affects the symptoms of arthritis.
Based on materials from Medical News Today
See also on the Lakhta Clinic website the articles “Arthritis and arthrosis”, “Rheumatoid arthritis”.
Prohibited Products
Dietary nutrition will be beneficial only if you completely remove from the diet foods that cannot be eaten with rheumatoid arthritis of the joints:
- white flour products;
- pickles and preserves;
- meat broths and any fatty meat, offal;
- semi-finished and smoked products;
- canned fish and meat;
- sauces, hot seasonings, mayonnaise and ketchup;
- salted, dried and smoked fish;
- nightshade vegetables (tomatoes, peppers, eggplants, pumpkin, potatoes);
- corn and wheat grits;
- full-fat milk and dairy products;
- sweets, chocolate, cocoa;
- alcohol.
Diet during exacerbation
The acute form of the disease requires strict adherence to avoidance of prohibited foods.
- Diet for rheumatoid arthritis - basic rules for successful treatment
Nutrition for rheumatoid arthritis during an exacerbation requires complete exclusion:
- gluten-containing products;
- Sahara;
- fatty meat products, liver and kidneys;
- fatty dairy products;
- allergenic products (citrus fruits, strawberries, tomatoes);
- juices, compotes, coffee and tea (due to limited fluid intake).
Fully or partially limited products
The diet for rheumatoid polyarthritis excludes fatty concentrated meat/fish broths, fatty red meats (pork) and waterfowl poultry (goose, duck), various types of offal (tongue, liver, brains), as well as meat products - sausages , semi-finished meat products, ham, ham. Animal fats, hydrogenated foods (mayonnaise, margarine), cooking oil, smoked, pickled, salted and canned foods are excluded from the diet. The consumption of confectionery products, chocolate, cocoa, products made from premium flour, starch and yeast-containing products, strong coffee, and black tea is not allowed.
It is prohibited to consume seafood (mussels, squid, crabs, oysters, shrimp), crustacean seasonings based on them, anchovies, red fish caviar, products of the nightshade family - eggplant, tomatoes/tomato products, potatoes, sweet peppers, paprika, seasonings/spices. Citrus fruits, grapes, avocados, raspberries, pomegranates, strawberries, wild strawberries, and currants are subject to restrictions. It is prohibited to include in the diet full-fat whole milk, legumes, fatty dairy products, vinegar, honey, snacks, jam, jam, alcohol and drinks containing carbon dioxide.
Table of prohibited products
| Proteins, g | Fats, g | Carbohydrates, g | Calories, kcal | |
Vegetables and greens | ||||
| eggplant | 1,2 | 0,1 | 4,5 | 24 |
| beans | 6,0 | 0,1 | 8,5 | 57 |
| peas | 6,0 | 0,0 | 9,0 | 60 |
| chickpeas | 19,0 | 6,0 | 61,0 | 364 |
| salad pepper | 1,3 | 0,0 | 5,3 | 27 |
| soybeans | 34,9 | 17,3 | 17,3 | 381 |
| tomatoes | 0,6 | 0,2 | 4,2 | 20 |
| beans | 7,8 | 0,5 | 21,5 | 123 |
| horseradish | 3,2 | 0,4 | 10,5 | 56 |
| lentils | 24,0 | 1,5 | 42,7 | 284 |
| sorrel | 1,5 | 0,3 | 2,9 | 19 |
Fruits | ||||
| figs | 0,7 | 0,2 | 13,7 | 49 |
Berries | ||||
| grape | 0,6 | 0,2 | 16,8 | 65 |
| cranberry | 0,5 | 0,0 | 6,8 | 26 |
| raspberries | 0,8 | 0,5 | 8,3 | 46 |
Mushrooms | ||||
| mushrooms | 3,5 | 2,0 | 2,5 | 30 |
Snacks | ||||
| potato chips | 5,5 | 30,0 | 53,0 | 520 |
Flour and pasta | ||||
| pasta | 10,4 | 1,1 | 69,7 | 337 |
Bakery products | ||||
| buns | 7,9 | 9,4 | 55,5 | 339 |
Confectionery | ||||
| jam | 0,3 | 0,1 | 56,0 | 238 |
| pastry cream | 0,2 | 26,0 | 16,5 | 300 |
Ice cream | ||||
| ice cream | 3,7 | 6,9 | 22,1 | 189 |
Chocolate | ||||
| chocolate | 5,4 | 35,3 | 56,5 | 544 |
Raw materials and seasonings | ||||
| mustard | 5,7 | 6,4 | 22,0 | 162 |
| mayonnaise | 2,4 | 67,0 | 3,9 | 627 |
| sugar | 0,0 | 0,0 | 99,7 | 398 |
Dairy | ||||
| baked milk | 3,0 | 6,0 | 4,7 | 84 |
| cream | 2,8 | 20,0 | 3,7 | 205 |
| sour cream 25% (classic) | 2,6 | 25,0 | 2,5 | 248 |
| sour cream 30% | 2,4 | 30,0 | 3,1 | 294 |
| Ryazhenka 6% | 5,0 | 6,0 | 4,1 | 84 |
Meat products | ||||
| pork | 16,0 | 21,6 | 0,0 | 259 |
| pork liver | 18,8 | 3,6 | 0,0 | 108 |
| pork kidneys | 13,0 | 3,1 | 0,0 | 80 |
| salo | 2,4 | 89,0 | 0,0 | 797 |
| beef | 18,9 | 19,4 | 0,0 | 187 |
| beef liver | 17,4 | 3,1 | 0,0 | 98 |
| beef brains | 9,5 | 9,5 | 0,0 | 124 |
| mutton | 15,6 | 16,3 | 0,0 | 209 |
| bacon | 23,0 | 45,0 | 0,0 | 500 |
Sausages | ||||
| smoked sausage | 28,2 | 27,5 | 0,0 | 360 |
Bird | ||||
| duck | 16,5 | 61,2 | 0,0 | 346 |
| goose | 16,1 | 33,3 | 0,0 | 364 |
Fish and seafood | ||||
| fried fish | 19,5 | 11,7 | 6,2 | 206 |
| smoked fish | 26,8 | 9,9 | 0,0 | 196 |
| Red caviar | 32,0 | 15,0 | 0,0 | 263 |
| squid | 21,2 | 2,8 | 2,0 | 122 |
| shrimps | 22,0 | 1,0 | 0,0 | 97 |
| mussels | 9,1 | 1,5 | 0,0 | 50 |
| canned fish | 17,5 | 2,0 | 0,0 | 88 |
| sardine in oil | 24,1 | 13,9 | — | 221 |
| salmon | 21,6 | 6,0 | — | 140 |
| mackerel | 18,0 | 13,2 | 0,0 | 191 |
| cod (liver in oil) | 4,2 | 65,7 | 1,2 | 613 |
Oils and fats | ||||
| animal fat | 0,0 | 99,7 | 0,0 | 897 |
| cooking fat | 0,0 | 99,7 | 0,0 | 897 |
Alcoholic drinks | ||||
| white dessert wine 16% | 0,5 | 0,0 | 16,0 | 153 |
| red dessert wine | 0,5 | 0,0 | 20,0 | 172 |
| vodka | 0,0 | 0,0 | 0,1 | 235 |
| cognac | 0,0 | 0,0 | 0,1 | 239 |
| liquor | 0,3 | 1,1 | 17,2 | 242 |
| beer | 0,3 | 0,0 | 4,6 | 42 |
Non-alcoholic drinks | ||||
| coffee | 0,2 | 0,0 | 0,3 | 2 |
| black tea | 20,0 | 5,1 | 6,9 | 152 |
| * data is per 100 g of product | ||||
Gluten-free diet
Abstaining from foods containing a special grain protein - gluten, is recommended for people with cyalkia (individual gluten intolerance). The development of this pathology against the background of autoimmune arthritis was noted.
However, a study by nutritionists and arthrologists conducted between two groups of 66 patients suffering from rheumatoid joint inflammation proved a direct link between the effect of gluten on the symptoms of arthritis. It is worth noting that these patients did not have any signs of cyalkia. According to this study, patients on a gluten-free diet showed increased activity of antibodies that reduce inflammation.
A gluten-free diet for exacerbation of rheumatoid arthritis allows you to include the following foods in your diet:
- boiled eggs, omelettes;
- boiled lean meat and fish;
- baked goods made from soy and bean flour;
- rice and buckwheat porridge;
- rice cakes;
- vegetable soups and salads;
- low-fat kefir and cottage cheese;
- baked apples;
- fruits;
- rosehip drink.
In addition to grain products, you need to exclude products containing yeast, malt sugar, pasta, sauces, mayonnaise, and processed foods. When buying tea, instant coffee, kefir and other food products, you must carefully study the composition for gluten content.
Physiotherapy
Physiotherapy is an integral part of complex treatment for arthritis (ICD-10 code M05–M99) of the joints. Some of them are used during the acute period of the disease. Procedures that are done for inflamed joints:
- electrophoresis with glucocorticoids;
- ultraviolet radiation.
They relieve inflammation and pain.
At other stages of the disease the following is prescribed:
- magnetic therapy;
- laser irradiation;
- phototherapy using lamps;
- massage and self-massage;
- mud baths;
- hydrotherapy.
Therapeutic gymnastics is very important for damaged joints. It helps improve their mobility and prevents the formation of adhesions. The patient should perform exercises daily from the very beginning of the diagnosis, excluding the time of exacerbation of the disease. In addition, patients with autoimmune arthritis should receive an annual course of sanatorium-resort treatment, and the use of essential medications is not canceled.
Dong Diet
The American Dong diet is based on avoiding fatty foods, red meat and dairy products. The food system also limits the consumption of fruits and nightshade vegetables.
It is recommended to include in the weekly diet menu for rheumatoid arthritis:
- red fish;
- chicken's meat;
- rice;
- baked and boiled vegetables;
- olive oil;
- greenery.
The diet course lasts for two weeks. This strict diet is an excellent nutrition option during an exacerbation period. Once symptoms have eased, there is no need for such strict restrictions.
Vegetarian diet
A plant-based diet is also effective in reducing symptoms of arthritis flare-ups. This effect is achieved by avoiding animal fats and proteins, and switching to foods rich in complex carbohydrates and fiber.
It is worth noting that raw plant foods are a source of many vitamins, including groups B, C and P, necessary for the production of the anti-inflammatory hormone cortisol.
Sometimes the menu includes eggs and lean fish rich in Omega-3 acid, calcium and vitamin D. This helps strengthen joints and prevent their destruction.
A plant-based diet is effective for those who need to lose weight to relieve pressure on their joints.
Vegetarian raw and mono diets can reduce inflammation in rheumatoid arthritis, but it is not recommended to adhere to them constantly. It is better to resort to such nutrition on fasting days.
Surgery
Experts resort to surgical intervention for arthritis only when all methods of conservative therapy have been tried. During surgical intervention, the use of two techniques is of greatest importance:
- synovectomy – removal of the articular synovial membrane;
- complete joint replacement with an endoprosthesis.
The decision to replace a joint is made by an orthopedist together with a rheumatologist. The operation is performed when the joint is very deformed and has lost its ability to move. And the most important thing is the patient’s desire to undergo surgery. In this case, the postoperative period is much more successful. An artificial prosthesis can last from 5 to 15 years. The patient needs to take care of the new joint and limit its mobility.
Chronic disease of joint tissues, which subsequently affects cartilage and bone structures, is a very serious illness. In the absence of proper therapy, it constantly progresses and leads to disability. Only comprehensive treatment and patient compliance with all doctor’s recommendations leads to remission.
Don't delay your visit to the doctor. Self-medication, as well as unauthorized withdrawal of medications, is unacceptable for this disease. They will result in deterioration of health and progression of the disease.
You can make an appointment at the Canon clinic on the website or by phone +7
Diets during remission
During periods of remission, strict restrictions can be lifted. However, you should eat prohibited foods no more than several times a week in limited portions.
The following products can be added to the menu during remission of rheumatoid arthritis:
- bread made from rye flour;
- beef, veal and pork in small portions;
- offal;
- coffee, tea, freshly squeezed juices, compotes;
- pasta;
- nuts;
- boiled potatoes.