Basic principles of diet for intestinal diseases
Pathologies and intestinal diseases occupy leading positions in the list of the most common diseases of our time. What is the reason? Large and dynamic cities dictate their own living conditions. The result of this is a fundamentally incorrect approach to one’s own nutrition: constant “snacks”, fast food and other harmful and low-quality food, eternal diets and starvation of girls who believe that the secret of beauty is painful thinness, frequent and uncontrolled use of antibiotics, regardless of whether they are needed or not.
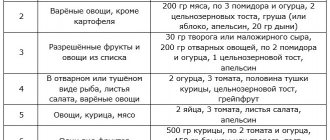
As a result, the intestinal microflora suffers greatly, and inflammation of the intestinal mucosa occurs.
Inflammatory bowel diseases, according to the nature of their course, can be divided into acute, when the disease is severe, usually short-term in duration, and chronic, characterized by a sluggish course of the disease with periods of exacerbation.
The inflammatory process that causes intestinal dysfunction can affect either the entire intestine or a specific part of it. By localization, inflammatory bowel diseases can be divided as follows:
:
- Enteritis
- an inflammatory process that is localized in the small intestine and can affect both a separate part of it and the entire organ.
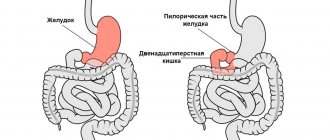
- Duodenitis
- inflammation of the duodenum, in most cases the disease begins from the first section, where the stomach passes into the intestines.
- Mesadenitis
- inflammation of the lymph nodes, which can provoke various pathologies of the mucous membranes.
- Colitis
- inflammation of the mucous membrane of the large intestine, which in most cases affects the entire organ, but inflammation of its individual parts also occurs.
Inflammatory phenomena occurring in the intestines have quite serious consequences. They lead not only to disturbances in its function, but also to organic pathology.
Due to intestinal diseases, the natural process of digesting food entering the body is disrupted. The disorders are accompanied by insufficient absorption of water and nutrients for the normal functioning of the human body. In addition, serious problems begin in the form of a disruption in the process of removing toxic metabolic products. The main symptoms of the appearance and development of intestinal diseases are
:
- Abdominal pain
- often a person cannot accurately indicate the location of the pain, but characterizes it as bursting or squeezing, pills bring only temporary relief, the condition resembles irritable bowel syndrome.
- Nausea after eating
- often this sign indicates inflammation of the duodenum or small intestine.
- Bloating
- most often indicates a lack of enzymes involved in the digestion process.
- Weight loss
- which most often indicates insufficient absorption of nutrients by the intestinal walls.
It is important to note that any inflammatory bowel disease requires immediate treatment, and diet for gastrointestinal diseases is an essential addition to treatment. Compliance with certain dietary restrictions can significantly improve your well-being, speed up recovery and prevent new relapses of the disease.
A specific nutritional regimen should be selected by the attending physician, taking into account the diagnostic results, the stage of the disease and the presence of concomitant disorders.
There are several nutritional principles that should be followed for inflammatory diseases of the gastrointestinal tract
:
- it is necessary to provide the patient with a complete, varied and balanced diet in accordance with the physiological needs of the body and the characteristics of the pathological process; you should not cut down the daily caloric intake too much;
- it is important to ensure mechanical sparing of the gastrointestinal mucosa;
- it is worth ensuring chemical sparing of the receptors and mucous membrane of the gastrointestinal tract
- In the acute stage, functional rest of the stomach, intestines, pancreas, liver and biliary system is necessary;
- thermal sparing of the mucous membrane and receptor apparatus of the gastrointestinal tract is necessary.
Now let’s take a closer look at each of the above principles and how to correctly implement it in practice.
The principle of a balanced diet
For diseases of the digestive system, just as for any other diseases, nutrition must be complete, balanced and provide the physiological needs of the body for basic nutrients. However, it must be emphasized that this is a method of nutritional treatment, so the diet is made up of specially selected and prepared products that affect individual pathogenetic links of the disease.
We recommend
“The benefits of grapes: vitamin content, calorie content and recommendations for consumption” Read more
First of all, when prescribing a particular diet, changes in the organs that are primarily affected by each specific disease are taken into account. For example, the gastroduodenal region for peptic ulcers, the pancreas for pancreatitis, etc. Next, the condition of the organs and systems most often involved in the pathological process is taken into account. For example, the intestines, biliary system for peptic ulcers: pancreas, liver, biliary system for intestinal diseases, etc. Be sure to pay attention to the degree of metabolic disorder and its possible correlation, as well as the state of the body as a whole.
Most diets used in gastroenterological practice contain the physiological norm of all nutrients per kilogram of human body weight
:
- 1.5-2.0 g proteins;
- 1.5-2.0 g fat;
- 5.0-6.0 g carbohydrates.
In some cases, in accordance with the characteristics of the course of the disease, corrections are made to these values. Thus, with increased catabolic processes, increased losses, especially proteins, due to a particular disease (for example, chronic intestinal diseases, diseases of the operated stomach, etc.), the body’s need for certain nutrients increases. In these cases, the daily intake of nutrients increases. More often this applies to proteins, vitamins and some minerals, such as potassium, calcium, iron, phosphorus.
Mechanical sparing principle
When prescribing a particular diet, it is necessary to take into account the local effect of food on the mucous membranes and the receptor apparatus of the gastrointestinal tract, in particular, its mechanical, chemical and thermal effects. The mechanical effect of food on the mucous membrane and receptor apparatus of the gastrointestinal tract is determined by the volume of food, its consistency, degree of grinding, the nature of heat treatment, and the amount of substances in the food that irritate the receptor apparatus and mucous membranes of the stomach and intestines. Mechanical irritants include fiber, cell membranes, and connective tissue. All diets used in gastroenterological practice have different requirements in terms of mechanical effects on the gastrointestinal tract.
In case of peptic ulcer of the stomach and duodenum in the stage of sharp exacerbation with symptoms of irritable stomach, chronic enterocolitis in the stage of sharp exacerbation with profuse diarrhea, exacerbation of chronic pancreatitis, diseases of the operated stomach and some other diseases of the digestive system, in which strict mechanical sparing is necessary, the daily volume of food is reduced before and is divided into 5-6, and sometimes even 8-10 doses (early periods after gastric surgery).
In some cases, the patient is given separate liquid and solid food with an interval of 1.5-2 hours (moderate or severe dumping syndrome). Dishes with a liquid and mushy consistency have less mechanical impact on the stomach and leave it faster than solid and compact dishes.
Another method of mechanical sparing is grinding food by passing it through a meat grinder.
And finally, another way to mechanically spare the receptors and mucous membrane of the gastrointestinal tract is to select products that contain less connective tissue. For example, rabbit meat, turkey meat, white chicken meat, veal, etc. Sources of connective tissue are fascia and tendons of meat, skin of fish and poultry.
In diets with pronounced mechanical sparing, meat must be thoroughly cleaned from fascia and tendons in its raw form before preparing minced meat; fish and poultry must be skinned. It is also necessary to limit all those products that contain fiber and cell membranes, which are strong mechanical irritants to the mucous membrane and receptor apparatus of the gastrointestinal tract.
For the same reason, the most gentle diets sharply limit vegetables, fruits and cereals, which contain a lot of fiber and cell membranes. There are especially many of them in the outer part of cereals (bran, millet, wholemeal flour, crushed wheat), and legumes. Carrots, beets, rutabaga, and green peas contain a lot of fiber and cell membranes. When included in the diet, they are served boiled and pureed.
The principle of chemical sparing
For any inflammatory diseases of the gastrointestinal tract, special importance is attached to chemical sparing of the secretory apparatus, receptors and mucous membrane of the gastrointestinal tract. The chemical effect of food is determined by a number of factors. First of all, the amount of nutrients that affect secretory processes in the gastrointestinal tract, the motor function of the stomach, intestines, and gall bladder. These are organic acids, extractives, essential oils, etc.
Organic acids enhance the secretion of gastric juice and intestinal motility, extractive substances accelerate the secretory process in the stomach, intestines, pancreas, liver, and biliary system as a whole. When frying, aldehydes and acroleins are formed, which are products of incomplete breakdown of fats. They, in turn, irritate the parenchyma of the liver and pancreas, so frying is extremely rarely used in diet therapy for diseases of the digestive system.
Another type of chemical sparing is a significant or complete limitation of table salt.
Thermal sparing principle
The temperature factor has an effect as soon as food comes into contact with the mucous membrane of the gastrointestinal tract, this is especially significant for its upper sections - the esophagus and stomach. Contrasting temperatures have a reflex effect on the underlying parts of the gastrointestinal tract, as well as on the functional state of the liver and pancreas.
The most preferred dishes are those whose temperature is close to that in the stomach - 36-37°C. Dishes with a temperature above 60-62°C have an irritating effect on the mucous membrane of the esophagus, stomach, and partly the duodenum. In addition, such dishes delay gastric emptying for a long time, thereby having a negative effect on motor function, reflexively increasing intestinal motility, and causing spasm of the sphincter of Oddi.
Fully or partially limited products
The diet of treatment tables for diseases of the gastrointestinal tract includes the following exceptions:
- Fatty meats/fish/poultry, smoked meats, canned meat/fish, meat products with the exception of cooked sausages.
- Products that stimulate the secretion of the gastrointestinal tract - extractive substances (concentrated and fatty meat/fish broths).
- Products containing essential oils (garlic, radish, celery, onion, spinach, radish).
- Products/dishes that enhance the processes of fermentation and rotting - rye bread, legumes, vegetables with coarse fiber, beer, fresh wheat bread.
- Spicy, salty, blue cheeses.
- Barley, millet, corn and pearl barley.
- Cooking/animal fat, margarine, mayonnaise.
- Ice cream, chocolate, cakes, grape juice.
Table of prohibited products
| Proteins, g | Fats, g | Carbohydrates, g | Calories, kcal | |
Vegetables and greens | ||||
| vegetables legumes | 9,1 | 1,6 | 27,0 | 168 |
| swede | 1,2 | 0,1 | 7,7 | 37 |
| cucumbers | 0,8 | 0,1 | 2,8 | 15 |
| parsnip | 1,4 | 0,5 | 9,2 | 47 |
| parsley (root) | 1,5 | 0,6 | 10,1 | 49 |
| radish | 1,2 | 0,1 | 3,4 | 19 |
| white radish | 1,4 | 0,0 | 4,1 | 21 |
| turnip | 1,5 | 0,1 | 6,2 | 30 |
| celery | 0,9 | 0,1 | 2,1 | 12 |
| horseradish | 3,2 | 0,4 | 10,5 | 56 |
| garlic | 6,5 | 0,5 | 29,9 | 143 |
| spinach | 2,9 | 0,3 | 2,0 | 22 |
| sorrel | 1,5 | 0,3 | 2,9 | 19 |
Fruits | ||||
| bananas | 1,5 | 0,2 | 21,8 | 95 |
| melon | 0,6 | 0,3 | 7,4 | 33 |
Berries | ||||
| grape | 0,6 | 0,2 | 16,8 | 65 |
Nuts and dried fruits | ||||
| dried fruits | 2,3 | 0,6 | 68,2 | 286 |
Cereals and porridges | ||||
| pearl barley | 9,3 | 1,1 | 73,7 | 320 |
| Wheat groats | 11,5 | 1,3 | 62,0 | 316 |
| millet cereal | 11,5 | 3,3 | 69,3 | 348 |
| barley grits | 10,4 | 1,3 | 66,3 | 324 |
Flour and pasta | ||||
| pasta | 10,4 | 1,1 | 69,7 | 337 |
Bakery products | ||||
| vysivkovy bread | 9,0 | 2,2 | 36,0 | 217 |
| Rye bread | 6,6 | 1,2 | 34,2 | 165 |
Confectionery | ||||
| candies | 4,3 | 19,8 | 67,5 | 453 |
| cookie | 7,5 | 11,8 | 74,9 | 417 |
| butter cookies | 10,4 | 5,2 | 76,8 | 458 |
Ice cream | ||||
| ice cream | 3,7 | 6,9 | 22,1 | 189 |
Cakes | ||||
| cake | 4,4 | 23,4 | 45,2 | 407 |
Raw materials and seasonings | ||||
| seasonings | 7,0 | 1,9 | 26,0 | 149 |
| mustard | 5,7 | 6,4 | 22,0 | 162 |
Meat products | ||||
| pork | 16,0 | 21,6 | 0,0 | 259 |
Sausages | ||||
| dry-cured sausage | 24,1 | 38,3 | 1,0 | 455 |
Bird | ||||
| duck | 16,5 | 61,2 | 0,0 | 346 |
| goose | 16,1 | 33,3 | 0,0 | 364 |
Fish and seafood | ||||
| dried fish | 17,5 | 4,6 | 0,0 | 139 |
| smoked fish | 26,8 | 9,9 | 0,0 | 196 |
| canned fish | 17,5 | 2,0 | 0,0 | 88 |
Oils and fats | ||||
| vegetable oil | 0,0 | 99,0 | 0,0 | 899 |
| animal fat | 0,0 | 99,7 | 0,0 | 897 |
| cooking fat | 0,0 | 99,7 | 0,0 | 897 |
Non-alcoholic drinks | ||||
| bread kvass | 0,2 | 0,0 | 5,2 | 27 |
Juices and compotes | ||||
| apricot juice | 0,9 | 0,1 | 9,0 | 38 |
| grape juice | 0,3 | 0,0 | 14,0 | 54 |
| plum juice | 0,8 | 0,0 | 9,6 | 39 |
| * data is per 100 g of product | ||||
Diet for intestinal diseases
Any diet for gastrointestinal diseases is designed to prevent any irritation of the intestinal mucosa. Although they are not able to influence the disease as such, with the right choice of food and its processing, the patient’s already significant discomfort is not aggravated. A proper diet with specially selected foods can speed up the healing process of the intestinal mucosa and alleviate the symptoms of the disease.
We recommend
“Flax for the intestines: benefits and recommendations” Read more
Most often, doctors of classical medicine for acute intestinal diseases and digestive disorders prescribe therapeutic diet No. 4, developed by gastroenterologist professor Manuil Pevzner. This nutrition system has several variations, depending on the patient's condition.
Diet No. 4 is a therapeutic diet, the main purpose of which is to reduce the load on the gastrointestinal tract and is prescribed for acute and chronic intestinal diseases, which are accompanied by diarrhea, bloating and other digestive disorders. The diet is prescribed for a fairly short period of time (from 3 to 7 days); in extreme cases, the duration of the diet can be increased to 14 days.
Study
: Prevention of cholic non-ulcerative colitis and irritable bowel syndrome
In addition, the diet is used for colitis and exacerbations of chronic gastrointestinal diseases (ulcers, gastritis, dysphagia). In such conditions, the patient develops dyspepsia, which is characterized by stool upset, abdominal pain, nausea, and cramps. Therefore, therapeutic nutrition should fully provide the patient during this period not only with nutrients, but also help reduce inflammatory reactions from the gastrointestinal mucosa.
The diet is also aimed at restoring microflora, relaxing muscles, and improving intestinal motility. The goal of a therapeutic diet is to ensure maximum relief of the digestive process, and as a result, restoration of the entire gastrointestinal tract. Table No. 4 provides for a special menu with strict control of the food consumed. But the main attention in this diet is given to sparing and restoring the mucous membrane of the gastrointestinal tract.
The basic principles of the 4 table diet are as follows
:
- Compliance with the calorie content of the diet (about 2050 kcal per day); in case of exhaustion or diarrhea, the daily calorie content can be increased to 2500-3000 kilocalories.
- Consuming 100 g of protein per day, including 70% animal origin, 250 g of carbohydrates, 70 g of fat.
- Limiting salt and sugar.
- Drink 1.5 liters of water daily.
- Cooking only by stewing and boiling.
- Eating food in liquid and pureed form.
- Fractional meals (4-5 times a day).
Features of cooking
In order to improve the general condition, improve the functioning of the intestines and reduce inflammation in it, you should adhere to certain rules of cooking
:
- In the process of preparing soups, you can use vegetable and weak meat broths.
- Porridge can only be cooked with water and broth. They prefer slimy and ground porridges.
- Meat dishes can consist of whole pieces of meat, fish or minced meat (meatballs, meatballs), prepared by stewing and steaming.
- Vegetables are consumed after heat treatment in soups or as purees in limited quantities. For constipation, the amount of vegetables consumed can be increased to 300 grams per day.
- It is recommended to consume 1 egg per day, mainly as part of meals.
- Fried and baked foods are prohibited.
- It is necessary to observe the principle of thermal sparing, which provides for food temperatures ranging from 15 to 45 degrees.
What can you eat if you have acute diseases of the gastrointestinal tract?
List of allowed products for gastrointestinal diseases:
- Bread : protein-wheat
, wheat loaf, dried (yesterday's) - biscuit dry cookies or buns (not buttery), pies with potatoes, apples, or cheesecakes.
- Milk: see if your stomach tolerates it well. The same applies to fermented milk drinks and curd dishes: souffles, puddings or “balls”.
- Eggs: up to 1 pc. in a day.
- Fats: If your doctor approves the introduction of butter into your diet, great! As part of this diet, you can put 10 g of butter in your favorite dish or just eat a sandwich in the morning. Frying food in butter is strictly prohibited.
- “First” courses: puree soup, which can be prepared with water or a very weak and always low-fat broth. Chop the permitted vegetables into smaller pieces, add a little rice, buckwheat, oatmeal or small pasta like “stars” to the saucepan - tasty and nutritious.
- Meat and poultry: lean varieties and cooked in minced form. Cutlets or meatballs, soufflés or quenelles, rolls made from lean parts of beef, veal, rabbit or chicken - all this can become the highlight of even a festive dinner.
- Fish: cook chopped, make juicy meatballs, cutlets or meatballs. But it is not forbidden to cook it in pieces, but you need to choose a low-fat type: hake, pollock, pike, cod, haddock or ice fish.
- vegetable diet with potatoes, pumpkin, zucchini and carrots, pre-boiled and thoroughly pureed.
- Cereals, pasta. Avoid barley and millet, which still remain an unbearable burden for an irritated stomach. Any porridge should be boiled in water, or better yet, boiled to a viscous, tender mass, but not hard.
- Fruits and berries: choose only very sweet and certainly soft ones, without hard skin, make sure that they are ripe without any “buts”. Plums, melons and apricots should be avoided. Tasty tip: baked apple mousse is a great snack during this diet.
- Drinks: prepare fruit jelly or make compote from pureed sweet fruits and berries, you can steam rose hips or drink natural tea, for example, black tea with milk (unless your doctor has forbidden you milk).
- Sauces, spices: aromatic dill and parsley (greens need to be chopped), laurel. You can also prepare the most delicate sauces: sour cream or milk, they will add a new note to even a boring dish.
Lists of permitted and prohibited products
The diet helps reduce inflammation in the gastrointestinal tract, normalize bowel movements, whether diarrhea or constipation, by eliminating certain foods that cause excess bile and digestive enzymes. When compiling a treatment menu, it is recommended to exclude from the diet
:
- rich broths, first courses with pasta and whole grain cereals;
- flour products (only white bread crackers are allowed);
- fatty meat, fish;
- dairy products;
- all legumes;
- vegetables (can only be used for decoctions)
- fresh and dried berries and fruits;
- sparkling water, coffee, strong tea;
- sauces and spices, marinades and canned food, sausages.
We recommend
“Orange: benefits and harm” Read more
Can be included in the menu
:
- soups from lean fish, meat and vegetables;
- wheat crackers (100-200 g per day);
- white meat turkey, rabbit, chicken, lean veal and beef;
- oatmeal, rice and buckwheat (we are talking about pureed cereals);
- cocoa without milk, herbal infusions;
- butter (5 g per meal);
- soups with a slimy consistency, cooked in low-fat meat, fish broth or vegetable broth, with well-cooked cereals, noodles or noodles, the addition of meatballs is allowed.
Breakfast options you can cook
:
- oatmeal (ground) in water with butter, soft-boiled egg;
- oatmeal and boiled chicken in the form of pate with a little butter;
- casserole of buckwheat and fresh (homemade) cottage cheese in breadcrumbs with egg;
- casserole (soufflé) of rice without milk with eggs and butter, crackers;
- steamed chicken cutlets with butter and egg, rice on water.
Lunches
:
- low-fat chicken broth with semolina, grated buckwheat in water, steamed chicken cutlets;
- soup with meatballs and rice, buckwheat with steamed cutlets;
- light broth with rice and chicken soufflé with eggs and butter in the oven, toasted bread;
- steamed fish cutlets, buckwheat porridge, light vegetable broth with semolina;
- steamed turkey cutlets, water rice, turkey fillet broth with breadcrumbs;
- light broth soup with pureed beef and buckwheat, rice with steamed cutlet.
Dinners
:
- steamed omelette;
- buckwheat casserole with egg;
- soufflé made from rice, eggs and chicken;
- baked fish fillet and rice porridge;
- steamed turkey (or fish) cutlets, buckwheat porridge;
- buckwheat porridge and two soft-boiled eggs.
Green tea, coffee, decoctions of rosehip, currant, quince and bird cherry diversify the drinking regime and the vitamin composition of the diet.
What is not allowed for acute diseases of the gastrointestinal tract?
List of prohibited foods for gastrointestinal diseases:
- Spicy and salty;
- canned food;
- discard spices;
- radish, rutabaga, all types of cabbage, onions and beets, garlic, sorrel, turnips, radishes and some others. (Raw vegetables are not recommended. Vegetables containing coarse fiber are prohibited even when boiled. Therefore, they are excluded);
- whole grain and rye bread;
- mushrooms and any legumes;
- fatty meat, fish and poultry Pork lard and lamb fat;
- fried foods;
- all melons, plums, peaches and apricots, kiwis and pears. Fruits and berries with hard and dense skin.
- carbonated drinks;
Types of diets for various gastrointestinal diseases
Another interesting and working type of diet: the FODMAP diet, which is used for complaints of severe flatulence, abdominal pain, alternating diarrhea and loose stools - all manifestations of IBS (irritable bowel syndrome), as well as inflammatory bowel diseases.
The essence of the diet is to exclude carbohydrate groups that contain large amounts of fructose, lactose, fructans, galactans and sugar alcohol polyols. These carbohydrates are poorly absorbed in the intestines and promote the growth of bacterial and fungal flora, which leads to symptoms such as bloating, gas formation, pain and discomfort in the gastrointestinal tract.
We recommend
“Foods good for the kidneys: TOP-25 for good health” Read more
FODMAPs are found in a wide range of foods, and most people eat high FODMAP foods every day without problems. When FODMAPs are eaten, they move slowly through the small intestine, attracting water. When they reach the colon, gut bacteria use FODMAPs as a fuel source for survival. Bacteria quickly ferment FODMAPs, resulting in gas production.
Below are food groups that contain FODMAP substances. Oligosaccharides (fructans and galactooligosaccharides) are found in foods such as wheat, rye, onions, garlic and legumes. Disaccharides (lactose) - found in dairy products such as milk, soft cheeses, yoghurts. Monosaccharides (fructose) - found in honey, apples, corn syrups, etc. Polyols (sorbitol and mannitol) are found in some fruits and vegetables and are used as artificial sweeteners.
The FODMAP diet allows
:
- Reduce pain and discomfort.
- Reduce bloating and distension.
- Improve bowel function (reduce diarrhea or constipation).
- Improve quality of life.
The diet shows its effectiveness in eliminating the symptoms of diarrhea, bloating, and abdominal pain. Of course, strict adherence to all restrictions is required, but if they are followed correctly, many people feel improvement within the first week of the diet.
Study
: A diet low in FODMAPs reduces symptoms of irritable bowel syndrome
In addition to diet, it is also important to reduce the overall level of stress, increase the digestive capabilities of the gastrointestinal tract, and use nutritional supplements and medications if necessary.
Study
FODMAPs and Irritable Bowel Syndrome
List of permitted/prohibited products
| Allowed | Prohibited | |
| Fruits | Berries except blackberries and currants. Maximum 1 fruit (serving) per day: banana (mini or unripe), melon, clementine, grapes, ripe guava, kiwi (golden, green), lemon, lime, orange, passion fruit, pineapple, raspberry, rhubarb. | Apples, mangoes, dates, figs, pears, dried fruits, guava, papaya, watermelons, cherries, ripe bananas, persimmons, plums, prunes, peaches, nectarines, lychees, blackberries, currants, avocados (2-3 slices per day are allowed). |
| Vegetables | Arugula, bok choy, bean sprouts, cross salad, pickled or pickled beets, bell peppers, celery, cucumbers, eggplant, green beans, ginger root, cabbage (no more than half a cup per day), Chinese cabbage, lettuce, parsnips, spinach , chard, zucchini, seaweed, tomatoes, zucchini, turnips, radishes, olives, oyster mushrooms, dill, parsley. Limited starchy vegetables (no more than half a serving, for example, half a small potato per day): potatoes, pumpkin, squash, carrots. | Beets, broccoli, fennel, garlic, onions, shallots, Jerusalem artichokes, asparagus, artichoke, sweet green peas, sun-dried tomatoes, cauliflower, cabbage, mushrooms, corn. |
| Animal proteins | Organic (bio) meat chicken, turkey, lamb, duck, beef, pork. | Meat from farmed animals, sausages, sausages, canned meat. |
| Fish | Wild salmon, cod, trout, anchovies, herring, sardines, mackerel, low mercury wild fish. | Factory fish, fish with high mercury content, including tuna, shark, swordfish. |
| Cereals | Gluten-free grains including quinoa, rice, buckwheat, millet, amaranth, brown rice pasta, buckwheat noodles, and gluten-free oats. | Gluten-containing grains including wheat, barley, rye, spelled, bran, flour, couscous, oats not labeled as gluten-free. |
| Beans and legumes | All legumes (peas, beans, lentils, chickpeas). | |
| Nuts and seeds | All nuts and seeds except those prohibited. | Peanuts (classified as legumes), pistachios, cashews. |
| Dairy | Hemp, almond, rice or coconut milk. Cheeses with low lactose content: brie, camembert, cheddar, mozzarella, parmesan, pecorino, Swiss (hard cheeses). Butter. Lactose-free dairy products. | Cow, goat, sheep, soy milk, soft cheeses (ricotta, cream, Adyghe, etc.), cream, cottage cheese, yogurt, fermented baked milk, yogurt, powdered milk. |
| Sweeteners | Small amounts of stevia, 100% maple syrup, 100% date sugar, molasses (blackstrap molasses), sugar (refined sugar, brown sugar, cane sugar), vanilla extract. | Sweeteners (sorbitol, mannitol, isomaltose, maltitop, xylitol), concentrated fruit juices, high fructose corn syrup. |
| Beverages | Green and herbal teas, mineral water, filtered water, limited coffee. | Commercial fruit juices, energy drinks, alcohol, sodas. Chicory and dandelion tea. |
| Oils | Unrefined cold-pressed oils: olive, coconut, flaxseed. Butter, ghee. | Refined oils, margarine, salad dressings. |
The transition to a low FODMAP diet usually occurs in several stages
.
Stage 1
. Exclusion of prohibited products. The exclusion period for prohibited foods is usually 3-6 weeks.
Stage 2
. Elimination. The duration of the low FODMAP diet is usually 2 to 6 weeks or until symptoms improve. If you have SIBO (bacterial overgrowth syndrome), diet alone is not enough to reduce pathogenic or opportunistic flora.
Stage 3
. Diet expansion. In order to establish a response to a specific FODMAP carbohydrate, it is advisable to first expand the diet to foods containing only one of the listed carbohydrates. For example, start with dairy products to eliminate lactose intolerance. Then - with honey (a source of fructose). Mannitol is found in mushrooms, and sorbitol is found in fresh avocado and peach. Fructans, other than some fruits (melon, etc.), are the only FODMAP carbohydrate in fresh onions, red onions and garlic. Galactans are present in significant quantities in almonds. It takes 3 days to introduce one product.
We recommend
“Proper diet: menu planning and ready-made recipes” Read more
On the first day, a small portion of the product is consumed. It is usually recommended to start with half a serving (for example, 100 ml of yogurt). If symptoms appear after consuming even a small amount of this product, this may indicate lactose intolerance. You should try another product with the same carbohydrate after 3 days. If there are no symptoms when consuming a small portion, you should continue to assess the tolerability of a regular portion of the product on the 2nd day.
The next day you can use a standard portion of the product. If unpleasant symptoms and sensations appear, the test is not carried out on the third day, but a break is taken for another three days. If all is well, on the third day you can consume a larger portion of the product. The presence of symptoms will indicate that such large quantities should not be consumed. If there are no symptoms after three days, the tolerability of other products from the same group should be assessed. Each new product is evaluated according to the above scheme (day 1-2-3). There should be 3 days between tests with two different products in order to completely eliminate the influence of the previous test on the subsequent one.
After analyzing the tolerance of various products within one group (for example, the group of milk and fermented milk products), you can move on to assessing other carbohydrates. Try a fructose tolerance test with honey and mango. The next food group to evaluate is, for example, lentils, hazelnuts and almonds (containing only galactans). Pomegranate, grapefruit, melon and some other fruits, garlic and onions will help assess your fructan tolerance. Sorbitol is found in peach, apricot, avocado, and blackberry. Mannitol is found in large quantities in mushrooms (champignons, porcini mushrooms), as well as in cauliflower.
Diet for intestinal diseases in children
The child may also have intestinal diseases. Dyspeptic syndrome is quite common: diarrhea, bloating. In such cases, pediatricians, gastroenterologists and nutritionists even recommend that children adhere to the same therapeutic diet No. 4, since it is not dangerous for the child’s body, and the choice of products is really wide, so people with allergies have the opportunity to replace allergenic foods. And, of course, the diet is really effective for digestive disorders.
If doctors have prescribed a fourth diet, which is therapeutic, you should not neglect this; it is advisable to think over a high-quality diet that the child will like. For moral support, you can diet with him. Parental support is always extremely important for a child, especially since treatment table No. 4 is, in principle, a fairly suitable and gentle option for a child’s incompletely formed gastrointestinal tract.
Diet for gastritis in the acute stage
The diet for gastritis in the acute stage deserves special attention. The requirements for products are the same as for all types of this pathology, but more stringent.
In acute forms of the disease, it is recommended:
- low-fat cottage cheese;
- yesterday's white bread and no pastries or baked goods;
- only lean meat, boiled and pureed or finely chopped;
- soups made exclusively with vegetable broths;
- non-acidic compotes and jelly;
- soft-boiled eggs or in the form of a steam omelet;
- vegetable purees from the baby food range; it’s also a good idea to borrow fish and meat purees from a jar from your kids;
- teas or infusions without sugar.
During the period of immediate exacerbation, the following are completely excluded from the menu:
- products with preservatives, flavor enhancers, artificial colors;
- raw vegetables and fruits;
- milk and any dairy dishes;
- all types of baked goods, except day-old bread;
- margarine, cooking oil and butter;
- pearl barley;
- all types of beans and beans.
All general restrictions on the products themselves and methods of their preparation also remain in force. Usually, the crisis passes in 3-4 days, then the diet becomes more varied, in accordance with the general recommendations for patients with gastritis.
Consequences of not following the diet
With spontaneous refusal of therapeutic nutrition, especially at the acute stage of the disease,
:
- pain symptoms, spasms;
- nausea, vomiting;
- diarrhea, to dehydration;
- bile flow disorders, hepatic colic;
- intoxication of the body due to intestinal infections, hepatitis C.
Errors in diet cause relapse of chronic gastrointestinal pathology.
Types of diets:
There are different types of diets for gastritis
The diet depends on the type of disease (high/low acidity) and the course of gastritis (acute form or chronic form.
For gastritis with low acidity, it is recommended to stick to table No. 2, which includes juice products.
For gastritis with high acidity, diet No. 1 and its variations are recommended. In case of exacerbation, table 1A is prescribed for 7-10 days with a gradual transition to table 1 B.
Dietary recipes
Chia pudding
To prepare you will need
:
- 4 tbsp. chia seeds
- 150 ml coconut milk
- fresh or frozen berries to taste
We recommend
“Metabolism: foods to speed up metabolism and lose weight” Read more
In the evening, pour the chia seeds with coconut milk in a separate container and mix well. Cover with a lid and place in the refrigerator overnight. In the morning, take out the pudding and stir, remove and wash the berries, grind in a blender. Place the pudding in a bowl/glass/deep container in layers: 1 layer berry puree, 2 layer chia. And so on until the ingredients run out. You can decorate the top with a mint leaf.
Buckwheat with coconut milk with berries and vanilla
To prepare you will need
:
- 30 grams of buckwheat
- 200 ml coconut milk
- 1 handful of berries (fresh or frozen)
- vanilla to taste
Rinse the buckwheat, add 150 ml of water and cook for 10 minutes. After the time has passed, add coconut milk, spices and berries and cook for another 5 minutes.
Rice porridge with pumpkin
To prepare you will need
:
- 70 g pumpkin
- 100 ml water
- 50 ml coconut milk
- 2 tbsp. rice
- 5 g butter
- 1 tsp poppy
- 20 g walnuts
- salt
Rinse the rice and soak in water for 15 minutes. Mix water, milk and put on low heat, add salt. Add rice, poppy seeds and stirring, cook over low heat for 7-10 minutes. Peel the pumpkin, cut and grate. Add to the porridge, cook the rice and pumpkin for another 5 minutes, stirring. Turn off the porridge, add butter. Add walnuts to the porridge. Cover with a lid and let stand for another 5 minutes.
Creamy risotto with chicken fillet and vegetables
To prepare you will need
:
- 150 g Risotto rice
- 200 g chicken fillet
- 1 tbsp. ghee
- 1 piece bell pepper
- green onions
- 1 piece carrot
- 100 ml coconut cream
- salt/pepper to taste
We recommend
“Vitamins for veins and blood vessels: nutritional rules for maintaining health” Read more
Wash, clean and cut the chicken fillet into cubes. Fry in ghee for 5-7 minutes. Wash, peel, chop the vegetables, add to the chicken and fry for another 7 minutes. Wash the rice, add to the vegetables and chicken, add salt/pepper and fill with water 2 fingers above the rice. Leave to cook over medium heat until done. Turn off the heat, add coconut cream, stir.
Cod soup
To prepare you will need
:
- 500 g cod fillet
- half a small zucchini
- 5 small potatoes
- 1 medium sized carrot
- salt to taste
All of the vegetables listed must be peeled and washed thoroughly. Cut the zucchini into thin strips and the potatoes into small cubes. Grate the carrots on a coarse grater. Next, you need to boil 1.5 liters of water and add chopped potatoes to it. After the water boils again, you need to reduce the heat, add the fish fillet, previously washed and cut into cubes. As the soup boils, you need to carefully remove the resulting foam. When the broth boils, add chopped zucchini and grated carrots, 1 tablespoon of sunflower oil and salt to taste. After this, reduce the heat and cook the soup for 20 minutes. Cover the finished dish with a lid and leave for half an hour.
Pumpkin Coconut Curry
To prepare you will need
:
- 1 tbsp. coconut oil
- 1 tbsp. grated fresh ginger
- 1 red bell pepper
- 200 g pumpkin
- 3 tbsp. tomato paste
- 1 tsp curry powder
- ½ tsp. turmeric
- 250 ml coconut milk
- 1 tbsp. lemon juice
- salt/pepper to taste
Wash, peel and chop the vegetables. Heat coconut oil in a frying pan, add vegetables and simmer for 15 minutes. Add milk, tomato paste, spices and simmer until the pumpkin is ready (soft). You can serve with greens and pumpkin seeds.
Cabbage pie with chicken fillet
To prepare you will need
:
- 300 g fresh cabbage
- 200 g chicken fillet
- 1 carrot
- 2 eggs
- 30 g walnuts
- herbs: dill, basil, thyme
- spices, salt, pepper
- 1 tbsp. ghee
Wash the fillet and cut into cubes. Fry in a preheated frying pan for 5-7 minutes. Wash, peel and cut vegetables as desired. Fry with the chicken for another 7 minutes. At this time, beat the eggs with a fork or whisk in a separate bowl. Add spices, salt, pepper to taste, herbs. Stir. Take a baking dish and place the chicken fillet and vegetables in it and fill it with the egg mixture. Sprinkle chopped walnuts on top. Place in a preheated oven at 180 degrees for 25-30 minutes.
Menu options
Option #1
Breakfast: steam omelette, herbal tea
Snack: baked apple
Lunch: cauliflower soup with croutons, fish cakes and mashed potatoes.
Afternoon snack: cottage cheese cake
Dinner: vegetable puree and boiled chicken breast, boiled beet salad with prunes
Option No. 2
Article on the topic
What types of therapeutic diets are there Breakfast: lazy dumplings with low-fat sour cream and strawberry syrup, weak tea
Snack: a bunch of white grapes
Lunch: white bean, carrot and spinach soup, baked beef with pumpkin slices, jelly
Afternoon snack: semolina casserole with pear
Dinner: rice zrazy with chopped lean beef, stewed zucchini
Option #3
Breakfast: semolina porridge with milk with berry jam, weak tea
Snack: banana and peach
Lunch: milk soup with baked pumpkin, buckwheat porridge with stewed carrots and steamed meatballs
Afternoon snack: baked apple
Dinner: vermicelli casserole with cottage cheese