GALVUS MET film-coated tablets 50mg+850mg No. 30
In patients receiving insulin, Galvus Met cannot replace insulin. Vildagliptin Liver dysfunction Since, when using vildagliptin, an increase in aminotransferase activity (usually without clinical manifestations) was noted somewhat more often than in the control group, before prescribing Galvus Met, as well as regularly during treatment with the drug, it is recommended to determine biochemical indicators of liver function. If a patient has elevated aminotransferase activity, this result should be confirmed by repeat testing, and then biochemical parameters of liver function should be regularly determined until they return to normal. If the excess of AST or ALT activity is 3 or more times higher than the ULN is confirmed by repeated testing, it is recommended to discontinue the drug. Metformin Lactic Acidosis Lactic acidosis is a very rare but severe metabolic complication that occurs when metformin accumulates in the body. Lactic acidosis during the use of metformin was observed mainly in patients with diabetes mellitus with high-grade renal failure. The risk of developing lactic acidosis increases in patients with diabetes mellitus that is difficult to treat, with ketoacidosis, prolonged fasting, prolonged alcohol abuse, liver failure and diseases that cause hypoxia. As lactic acidosis develops, shortness of breath, abdominal pain, and hypothermia occur, followed by coma. The following laboratory parameters have diagnostic value: decreased blood pH, serum lactate concentration above 5 nmol/l, as well as an increased anion gap and an increased lactate/pyruvate ratio. If metabolic acidosis is suspected, the drug should be discontinued and the patient should be hospitalized immediately. Monitoring renal function Since metformin is largely eliminated by the kidneys, the risk of its accumulation and development of lactic acidosis is higher, the more impaired renal function is. When using Galvus Met, renal function should be regularly assessed, especially in the following conditions that contribute to its impairment: the initial phase of treatment with antihypertensive drugs, hypoglycemic agents or NSAIDs. As a rule, renal function should be assessed before starting treatment with Galvus Megam, and then at least once a year for patients with normal renal function and at least 2-4 times a year for patients with serum creatinine above the ULN. In patients at high risk of renal impairment, renal function should be monitored more than 2-4 times a year. If signs of deterioration in kidney function appear, Galvus Met should be discontinued. Use of iodinated radiocontrast agents for intravascular administration When conducting x-ray examinations that require intravascular administration of iodinated radiocontrast agents, Galvus Met should be temporarily discontinued (during the examination, or immediately before it, as well as within 48 hours after the examination), since the intravascular administration of iodinated radiocontrast agents medications can lead to a sharp deterioration in kidney function and increase the risk of developing lactic acidosis. You can resume taking Galvus Met only after re-evaluating your kidney function. Hypoxia In acute cardiovascular failure (shock), acute heart failure, acute myocardial infarction and other conditions characterized by hypoxia, lactic acidosis and prerenal acute renal failure may develop. If the above conditions occur, the drug should be discontinued immediately. Surgical interventions During surgical interventions (with the exception of minor operations not related to restriction of food and liquid intake), Galvus Met should be discontinued. You can resume taking the drug after the patient begins to eat on his own and it is shown that his kidney function is not impaired. Alcohol consumption Alcohol has been found to enhance the effect of metformin on lactate metabolism. Patients should be warned against alcohol abuse while using Galvus Met. Vitamin B12 content It has been established that metformin causes an asymptomatic decrease in the serum concentration of vitamin B12 in approximately 7% of cases. Such a decrease in very rare cases leads to the development of anemia. Serum concentrations of vitamin B12 appear to quickly normalize after discontinuation of metformin and/or vitamin B12 replacement therapy. Patients receiving Galvus Met are recommended to undergo a general blood test at least once a year and, if any abnormalities are detected, determine their cause and take appropriate measures. It appears that some patients (eg, those with inadequate intake or malabsorption of vitamin B12 or calcium) are predisposed to decreased serum concentrations of vitamin B12. In such cases, it can be recommended to determine the serum concentration of vitamin B12 at least once every 2-3 years. Worsening of the condition of patients with type 2 diabetes mellitus who have previously responded to therapy If a patient with type 2 diabetes mellitus who has previously responded to therapy shows signs of deterioration (changes in laboratory parameters or clinical manifestations), and the symptoms are not clearly defined, tests should be performed immediately for detection of ketoacidosis and/or lactic acidosis. If acidosis in one form or another is confirmed, Galvus Met should be discontinued immediately and appropriate measures taken. Hypoglycemia Typically, in patients receiving only Galvus Met, hypoglycemia is not observed, but it can occur against the background of a low-calorie diet (when intense physical activity is not compensated for by the caloric content of food), or against the background of alcohol consumption. Hypoglycemia is most likely in elderly, weakened or malnourished patients, as well as against the background of hypopituitarism, adrenal insufficiency or alcohol intoxication. In elderly patients and in those receiving beta-blockers, the diagnosis of hypoglycemia may be difficult. Reduced effectiveness of hypoglycemic drugs When stress (fever, injury, infection, surgery, etc.) occurs in a patient receiving hypoglycemic drugs according to a stable regimen, a sharp decrease in the effectiveness of the latter for some time is possible. In this case, it may be necessary to discontinue Galvus Met and prescribe insulin. You can resume treatment with Galvus Met after the end of the acute period.
Galvus Met®
In patients receiving insulin treatment, Galvus Met® cannot replace insulin therapy. Galvus Met® should not be used to treat type 1 diabetes or diabetic ketoacidosis.
Vildagliptin
Liver dysfunction
The use of the combination drug vildagliptin + metformin is not recommended for patients with clinical or laboratory signs of liver dysfunction, including patients with an increase in ALT or AST >3 x ULN before treatment.
Rare cases of liver dysfunction (including hepatitis) have been reported with the use of vildagliptin. These cases were usually asymptomatic, without clinical consequences, and after discontinuation of therapy, liver function tests returned to normal. Liver function should be examined before starting therapy with the combination drug vildagliptin + metformin, then monitored once every 3 months during the first year of use of the drug, and then periodically. If an increase in aminotransferase activity is detected, a re-examination should be carried out to confirm the result, and then biochemical indicators of liver function should be regularly determined until they normalize. If an excess of AST or ALT activity of 3 or more times the ULN is confirmed upon re-examination, the use of the drug should be discontinued. If jaundice or other signs of liver dysfunction develop while using the vildagliptin + metformin combination, therapy should be discontinued immediately. After normalization of liver function indicators, treatment with the drug cannot be resumed.
Metformin
Lactic acidosis
Lactic acidosis is a very rare but severe metabolic complication, most often occurring with a sharp deterioration in renal function, as well as with cardiorespiratory syndromes and sepsis. With a sharp deterioration in kidney function, metformin accumulates in the body, which increases the risk of developing lactic acidosis.
If dehydration occurs (eg, associated with severe diarrhea or vomiting, fever, or decreased fluid intake), a patient taking metformin-containing medications (eg, Galvus Met®) should immediately stop taking the above medications and seek medical attention.
In patients taking drugs containing metformin (for example, Galvus Met®), caution should be exercised when initiating therapy with drugs that can acutely worsen renal function (for example, antihypertensive drugs, diuretics, NSAIDs). Other risk factors include: alcohol abuse, liver dysfunction, inadequately controlled diabetes mellitus, ketoacidosis, prolonged fasting, conditions associated with hypoxia, and concomitant use of drugs that can cause lactic acidosis.
Diagnosis of lactic acidosis
The patient and/or caregivers should be informed of the risk of developing lactic acidosis. Lactic acidosis is characterized by acidotic dyspnea, abdominal pain, muscle cramps, asthenia and hypothermia followed by coma. If symptoms develop that suggest the development of lactic acidosis, the patient should stop taking metformin-containing drugs (for example, Galvus Met®) and immediately seek medical help. Laboratory and instrumental examination data: decreased blood pH (<7.35), increased lactate concentration in the blood serum >5 mmol/l, as well as an increased anion gap and an increase in the lactate/pyruvate ratio. If lactic acidosis is suspected, therapy with metformin-containing drugs should be stopped and the patient should be hospitalized immediately.
Monitoring kidney function
Before starting therapy, GFR should be determined, and this indicator should be monitored periodically during drug therapy. The use of metformin-containing drugs (such as Galvus Met®) is contraindicated in patients with GFR <30 ml/min; in the presence of conditions that can impair renal function, the use of the above drugs should be temporarily suspended.
Since metformin is largely eliminated by the kidneys, the risk of accumulation and development of lactic acidosis increases with the severity of renal impairment. Because older age may be associated with deterioration of renal function, in patients in this category the dose of metformin-containing drugs (such as Galvus Met®) should be carefully adjusted to select the minimum dose that provides adequate glycemic effect, with regular monitoring of renal function.
Interactions
Concomitant use of medications that affect renal function or the distribution of metformin
Caution should be exercised when used concomitantly with drugs that can affect renal function, have significant hemodynamic effects or affect the distribution of metformin in the body, such as organic cations excreted by the kidneys by tubular secretion.
The use of iodine-containing radiocontrast agents for intravascular administration
Intravenous administration of radiopaque iodine-containing agents can provoke the development of contrast-induced nephropathy, leading to the accumulation of metformin in the body and increasing the risk of developing lactic acidosis. Metformin-containing medications (such as Galvus Met®) should be temporarily discontinued before or during the procedure; Dosage should be resumed no earlier than 48 hours after the procedure, after receiving laboratory confirmation of stabilization of renal function.
Alcohol consumption
It has been established that ethanol enhances the effect of metformin on lactate metabolism. The patient should be warned not to abuse alcohol while using metformin-containing drugs (such as Galvus Met®).
Alcohol intoxication is associated with an increased risk of lactic acidosis, especially with prolonged fasting, malnutrition and impaired liver function.
Vitamin B12 content
It has been established that metformin causes an asymptomatic decrease in the concentration of vitamin B12 in the blood serum in approximately 7% of cases. Such a decrease in very rare cases leads to the development of anemia. After discontinuation of metformin and/or vitamin B12 replacement therapy, serum concentrations of vitamin B12 quickly normalize. In patients receiving metformin-containing drugs (such as Galvus Met®), general clinical blood test parameters should be monitored at least once a year. If deviations of hematological parameters from the norm are detected, the etiology of such disorders should be clarified and appropriate treatment should be carried out. Some patients (eg, patients with insufficient intake or malabsorption of vitamin B12 or calcium) are predisposed to decreased serum concentrations of vitamin B12. In such patients, determining the concentration of vitamin B12 in the blood serum at least once every 2-3 years can have diagnostic value.
Hypoxia
Cardiovascular collapse (shock), acute heart failure, acute myocardial infarction, and other conditions characterized by hypoxemia are associated with lactic acidosis and may also contribute to prerenal azotemia. If the above conditions occur, the use of metformin-containing drugs (such as Galvus Met®) should be stopped immediately.
Surgical interventions
During surgical procedures under general, spinal or epidural anesthesia (except for minor operations not associated with restriction of food and fluid intake), the use of metformin-containing drugs (such as Galvus Met®) should be discontinued.
Resumption of the drug is possible no earlier than 48 hours after the intervention or after the restoration of oral food intake after receiving laboratory confirmation of stabilization of renal function.
Patients with liver dysfunction
Since lactic acidosis, which is one of the HPs of metformin, has been reported in some cases in patients with impaired liver function, the combination drug vildagliptin + metformin should not be used in patients with liver disease or impaired biochemical parameters of liver function.
Deterioration of the condition of patients with type 2 diabetes who previously responded to therapy
If a deviation in laboratory parameters from the norm is detected or clinical symptoms of a deterioration in the general condition appear (especially when symptoms are not clearly expressed and blurred) in patients with a previous adequate response to therapy, laboratory diagnostics should be immediately carried out to identify ketoacidosis and/or lactic acidosis. If acidosis is detected, you should immediately stop using the drug and take the necessary measures to correct the patient’s condition.
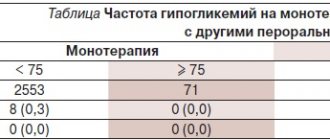
Hypoglycemia
As a rule, hypoglycemia is not observed in patients receiving therapy only with the combination drug vildagliptin + metformin, but it can occur against the background of a low-calorie diet (when intense physical activity is not compensated for by the caloric content of food), or against the background of alcohol consumption. The development of hypoglycemia is most likely in elderly, weakened or malnourished patients, as well as against the background of hypopituitarism, adrenal insufficiency or alcohol intoxication. In elderly patients and in those receiving beta-blockers, the diagnosis of hypoglycemia may be difficult.
Reduced effectiveness of hypoglycemic drugs
In case of stress (fever, injury, infection, surgery, etc.) that develops in patients receiving hypoglycemic drugs according to the standard regimen, a sharp decrease in the effectiveness of the latter for some time is possible. In this case, it may be necessary to temporarily discontinue therapy with the vildagliptin + metformin combination and transfer to insulin therapy. Resumption of treatment with Galvus Met® is possible after the end of the acute period.
Fertility
There have been no studies of the effect of the combination drug vildagliptin + metformin on fertility in humans. In animal studies, vildagliptin at doses 200 times higher than recommended did not cause fertility problems.
There were no adverse effects on fertility in males or females when metformin was administered at doses of 600 mg/kg per day, which is approximately 3 times the recommended human dose (based on body surface area).
Instructions for use GALVUSMET®
Suction
Galvusmet
In a bioequivalence study, Galvusmet tablets of different concentrations (50 mg/500 mg, 50 mg/850 mg and 50 mg/1000 mg) were compared with a combination of the individual drugs vildagliptin and metformin hydrochloride at corresponding doses. These studies demonstrated the bioequivalence of Galvusmet in combinations of individual drugs in terms of AUC and Cmax of both components of Galvusmet - vildagliptin and metformin hydrochloride.
Food intake does not affect the volume and extent of absorption of vildagliptin in Galvusmet. Cmax and AUC of metformin hydrochloride when taken with food decreased by 26% and 7%, respectively. The absorption of metformin hydrochloride was also delayed when taking the drug with food, which was reflected in Tmax (from 2.0 to 4.0 hours).
These changes in Cmax and AUC were consistent but less than those observed when metformin hydrochloride was taken alone with food. The effect of food intake on the pharmacokinetics of both components of the drug - vildagliptin and metformin hydrochloride - is similar to the effect on the pharmacokinetics of vildagliptin and metformin hydrochloride when used individually with food.
Vildagliptin
After oral administration on an empty stomach, vildagliptin is rapidly absorbed, Cmax in blood plasma is reached after 1.75 hours. Administration with food slightly reduces the degree of absorption of vildagliptin, which is characterized by a decrease in Cmax by 19%, and also delays the time to reach Cmax in blood plasma to 2.5 hours. Volume of absorption did not change, food did not affect exposure at all (AUC).
Metformin hydrochloride
The absolute bioavailability of metformin hydrochloride 500 mg tablets taken on an empty stomach is approximately 50% to 60%. Studies of single oral administration of metformin hydrochloride, tablets 500 mg to 1500 mg, and 850 mg to 2550 mg, indicate no dose-response relationship, which is due to decreased absorption rather than changes in elimination. Eating reduces the volume and slightly slows down the absorption of metformin hydrochloride, as evidenced by an approximately 40% lower mean Cmax, a 25% lower AUC, and a 35-minute increase in the time to reach Cmax after a single dose of 850 mg metformin hydrochloride with food. compared with the results after taking 850 mg of metformin hydrochloride on an empty stomach. The clinical significance of this decrease is unknown.
Linearity
Vildagliptin is rapidly absorbed, with absolute bioavailability after oral administration of 85%. Vildagliptin peak plasma concentrations and AUC increase over the therapeutic dose range in an approximately dose-dependent manner.
Distribution
Vildagliptin
The binding of vildagliptin to plasma proteins is low (9.3%); Vildagliptin is distributed equally between plasma and red blood cells. The average Vd of vildagliptin in the stationary phase after intravenous administration is 71 L, indicating extravascular distribution.
Metformin hydrochloride
The apparent Vd of metformin hydrochloride after a single oral dose of 850 mg averaged 654±358 L. Metformin hydrochloride is very little bound to plasma proteins, in contrast to sulfourea, which is more than 90% bound to plasma proteins. Metformin hydrochloride is distributed among red blood cells, most likely as a function of time. When using usual clinical doses and dosing regimens, steady-state plasma concentrations of metformin hydrochloride are achieved within 24 to 48 hours and are <1 mcg/ml. During controlled clinical trials of metformin hydrochloride, maximum plasma concentrations did not exceed 5 mcg/ml, even at the highest doses.
Metabolism
Vildagliptin
Metabolism is the major route of elimination of vildagliptin in humans, accounting for 69% of the dose. The main metabolite LAY151 is pharmacologically inactive and is a product of hydrolysis of the cyanogen fragment, accounting for 57% of the dose; followed by the hydrolysis product of the amide fragment (4% of the dose). DPP-4 is partially involved in the hydrolysis of vildagliptin.
Vildagliptin is not metabolized by cytochrome P450 enzymes to detectable amounts. In vitro studies have shown that vildagliptin does not inhibit or induce cytochrome P450 enzymes.
Removal
Vildagliptin
Following oral administration of 14C-vildagliptin, approximately 85% of the dose is excreted in the urine and 15% of the dose is excreted in the feces. After oral administration, 23% of the dose is excreted in the urine as unchanged vildagliptin. After intravenous administration to healthy volunteers, the total plasma clearance and renal clearance of vildagliptin are 41 L/h and 13 L/h, respectively.
The average T1/2 after intravenous administration is approximately 2 hours. T1/2 after oral administration is approximately 3 hours and does not depend on the dose.
Metformin hydrochloride
Studies using a single IV dose in healthy volunteers have shown that metformin hydrochloride is excreted unchanged in the urine and is not metabolized by the liver (no metabolites have been identified in humans) or excreted in the bile. Renal clearance is approximately 3.5 times higher than CC, which indicates tubular secretion as the main route of elimination.
After oral administration, approximately 90% of the absorbed drug is excreted by the kidneys within the first 24 hours, with a T1/2 from blood plasma of approximately 6.2 hours. In the blood, T1/2 is approximately 17.6 hours; this indicates that red blood cells may be a distribution compartment.
Pharmacokinetics in special groups of patients
Floor
No differences were observed in the pharmacokinetic parameters of vildagliptin or metformin hydrochloride
in men and women with different age ranges and body mass index.
Obesity
Body mass index has no effect on the pharmacokinetic parameters of vildagliptin
.
Liver failure
Exposure to vildagliptin
(100 mg) after a single dose in patients with mild and moderate hepatic impairment was reduced (20% and 8%, respectively), whereas vildagliptin exposure in patients with severe impairment increased by 22%. The maximum change (increase or decrease) in vildagliptin exposure is approximately 30%, which is not considered to be of clinical significance. There is no correlation between the severity of hepatic impairment and changes in vildagliptin exposure.
No pharmacokinetic studies have been performed on metformin hydrochloride.
in patients with liver failure.
Kidney failure
In patients with mild, moderate and severe renal impairment, as well as in patients with chronic renal failure who are on hemodialysis, systemic exposure to vildagliptin
increased (Cmax - from 8% to 66%; AUC - from 32% to 134%) compared with healthy volunteers.
Exposure to the inactive metabolite (LAY151) increased with increasing severity of renal failure (AUC 1.6-fold to 6.7-fold). Changes in vildagliptin exposure did not correlate with the severity of renal impairment, whereas changes in exposure to the inactive metabolite did.
T1/2 of vildagliptin did not change in renal failure. Based on the evaluation of the safety, tolerability and efficacy of vildagliptin in patients who participated in clinical trials with glomerular filtration values <60 ml/min, there is no need for dosage adjustment in patients with mild or moderate renal impairment. The use of vildagliptin is not recommended in patients with severe renal impairment or in patients with chronic renal failure who are on hemodialysis.
In patients with reduced renal function (based on determined QC) T1/2 of metformin hydrochloride
in plasma and blood is prolonged, and renal clearance decreases in proportion to the decrease in CC.
Elderly patients
In healthy elderly volunteers (>70 years), total exposure to vildagliptin
(100 mg 1 time/day) decreased by 32% with an 18% increase in Cmax in blood plasma compared with young healthy volunteers (aged 18 to 40 years). These differences are not considered clinically significant. Age-specific studies have shown that age does not affect DPP-4 inhibition by vildagliptin.
Limited data from controlled pharmacokinetic studies of metformin hydrochloride
in healthy elderly volunteers, indicate that the overall clearance of metformin hydrochloride from blood plasma is reduced, T1/2 is prolonged, and Cmax is increased compared to young volunteers. These data indicate that changes in the pharmacokinetics of metformin hydrochloride with age are mainly explained by changes in renal function.
Treatment with Galvusmet should not be initiated in patients aged >80 years unless CC determinations demonstrate no decline in renal function.
Children
No pharmacokinetic data available.
Ethnic groups
There is no evidence of an effect of ethnicity on the pharmacokinetics of vildagliptin or metformin hydrochloride.