A child can get diabetes at any age. But most often the pathology develops at 5-8 years and at 10-12 years. It is during these periods that increased growth of the body is observed, which is accompanied by intense metabolism. But recently, the number of diabetics among children under 5 years of age, including newborns, has been increasing.
Types of diabetes
- Type 1 – insulin dependent.
- Type 2 – insulin-independent.
The first type is most common in children. The disease is characterized by very low levels of insulin; the child requires constant monitoring.
In type 1 diabetes, the body does not produce enough insulin; it is necessary to constantly monitor its level and administer additional insulin if necessary. The cause is unknown and the disease cannot be prevented. Symptoms include thirst, constant hunger, excessive urination, fatigue, decreased visual acuity, and weight loss. Symptoms may occur suddenly.
Type 2 diabetes was previously observed only in adults, but is now appearing in children as well. The pathology is a consequence of ineffective absorption of insulin by the body. Develops against a background of physical inactivity and excess weight. Symptoms are less pronounced than with type 1. Source: A.B. Resnenko Type 2 diabetes mellitus in children and adolescents: from pathogenesis to treatment // Pediatric pharmacology, 2011, vol. 8, no. 4, pp. 125-129
Comparison table of LED types
| Signs and symptoms | Type 1 diabetes | Type 2 diabetes |
| The essence of metabolic processes | Insulin deficiency | Decreased insulin production |
| Spreading | In 5-10% of cases | In 90-95% of cases |
| Patient age | Children and teenagers | People over 40 years old |
| Body Features | Normal | Obesity |
| Onset of the disease | Acute | Unnoticeable, gradual |
| The body produces insulin | β-cells are affected, production is stopped | Insulin is produced, but cells do not use it to carry sugar |
| Insulin use | Necessarily | Not necessary |
| Treatment options | Insulin administration, diet | Diet, increase physical activity, take pills to reduce sugar |
Results
Elevated blood sugar can be a symptom of serious problems with metabolism and hormone production. To determine the cause of hyperglycemia, it is necessary to conduct a laboratory blood test. The most common factor influencing abnormal increases in glucose values is juvenile type 1 diabetes mellitus.
The disease is an incurable pathology of the endocrine system and requires lifelong insulin injections and adherence to dietary rules. The progression of the disease and the development of associated complications can be slowed down if you strictly adhere to medical recommendations.
Where does the disease come from in children?
Each type of diabetes has its own causes. There are risk factors that provoke the disease:
- mother or both parents are diabetic;
- viruses;
- high birth weight (more than 4.5 kg);
- obesity;
- presence of diathesis;
- frequent colds;
- weakened immune system;
- metabolic disease.
Many people are concerned about whether the disease is transmittable. The main cause of type 1 diabetes in children is heredity. This is confirmed by the large number of family cases when the disease occurs in a child in the presence of pathology in parents, grandparents.
The autoimmune process is initiated by an external factor – viruses. Chronic insulitis and insulin deficiency are caused by exposure to the ECHO virus, Coxsackie B virus, herpes, rubella, and Epstein-Barr. The disease can be caused by enterovirus, rotavirus, measles and others. Source: P.F. Litvitsky, L.D. Maltseva Disorders of carbohydrate metabolism in children: diabetes mellitus // Issues of modern pediatrics, 2021, v. 16, no. 6, p. 468-480
In children with a genetic predisposition, the disease can be triggered by intoxication, artificial feeding, monotonous carbohydrate diet, as well as stress and previous operations.
Type 2 diabetes in children develops due to dysfunction of the pancreas - when b-cells do not produce or secrete insulin. As a result, the sensitivity of the receptors decreases.
Mechanism and causes of type 1 disease
In juvenile diabetes, the endocrine function of the pancreas to produce insulin, the hormone that transports glucose into the cells and tissues of the body, stops. Sugar does not arrive “to the address”, but is concentrated in the blood. This causes energy starvation of cells and hyperglycemia (pathological increase in glucose levels). Sugar deficiency affects the cells of the pancreas itself, which eventually leads to their destruction.
Due to impaired carbohydrate metabolism, ketone bodies (toxic breakdown products) are rapidly formed. Their excessive amount threatens the body with acetone (ketone) intoxication, otherwise, ketoacidosis. Diabetic ketoacidosis in young children quickly turns into a state of hyperglycemic coma with possible death.
There are two main causes of juvenile diabetes:
- Autoimmune. Caused by a cardinal malfunction of the immune system. Instead of fulfilling its duties to protect the body, the immune system begins to produce autoimmune antibodies that destroy the body. Pancreatic cells become involved in the pathological process and stop producing insulin.
- Hereditary. In this case, diabetes owes its manifestations to unfavorable genetics. The biological ability of any organism to transmit morphological characteristics (including diseases) to its descendants increases the chances of developing the disease several times.
Important! From parents or close relatives, the child receives a hereditary predisposition (a set of abnormal genes), but not diabetes itself. The disease may or may not progress. It is impossible to give a 100% guarantee.
To activate an autoimmune or hereditary factor, a certain trigger (“trigger”) is required, the role of which is played by the following causes of diabetes:
- Intensive production of antibodies by the immune system as a reaction to allergens (allergies). Frequent and numerous allergic reactions in a child weaken the immune status.
- Infectious diseases of viral etiology (origin). Untimely treatment of viral diseases leads to decreased immunity. The occurrence of diabetes can be influenced by: mumps, herpes virus type 4 (Epstein-Barr), cytomegalovirus, Coxsackie virus, rubella.
- A high-carbohydrate diet combined with a sedentary lifestyle. The abundance of sweets, baked goods, and fast food in the children's menu disrupts the functionality of the pancreas and inhibits metabolic processes. In the absence of regular physical activity, this leads to obesity and hyperglycemia.
- Hypovitaminosis of D-group vitamins. Chronic deficiency of cholecalciferol and ergocalciferol in a child leads to immunosuppression.
- Chronic diseases. Pathologies of the thyroid and pancreas of a chronic nature adversely affect metabolic processes.
- Medications. Incorrect therapy with hormone-containing medications reduces the performance of the immune system.
An additional factor in the development of chronic hyperglycemia is artificial feeding of infants with a hereditary tendency to diabetes with cereal mixtures or cow's milk.
The order of development of pathology
Insulin is a hormone produced by the pancreas, which is small in a child. By the age of 10, the iron weighs 50 grams and its length is 12 cm. The main function is the production of insulin. The gland should cope with the task by the age of 5.
The greatest risk of diabetes occurs between the ages of 5 and 11 years. At this time, metabolism is fast, sugar is well absorbed. Every child needs 10 grams of carbohydrates. The exchange is controlled by an incompletely formed nervous system, and failures may occur.
Those at risk include teenagers going through puberty, premature babies and children who experience heavy stress.
The course of the disease depends on the age at which the pathology appeared. In children, diabetes is severe and leads to complications. Parents must understand that diabetes in children requires care and lifelong treatment.
Briefly about blood sugar regulation
Glucose is the main monosaccharide that provides complete nutrition to the brain and compensation for energy costs to all organs and systems. The substance is released during digestion from saccharides, which are contained in carbohydrate products, and amino acids, formed from protein. After the formation of glucose, a smaller part of it is absorbed by the liver, where it is transformed into glycogen - a kind of carbohydrate reserve. A larger amount enters the systemic circulation and is distributed throughout the body under neuro-hormonal control.
Maintaining stable glycemia is ensured by:
- intrasecretory hormones of the pancreas: insulin, which is responsible for transporting glucose into the cells and tissues of the body, reducing its level in the blood; glucagon, which synthesizes glucose from stored glycogen, increasing glycemia;
- hormones of the adrenal cortex - catecholamines (norepinephrine and adrenaline) and cortisol, stimulating the processes of glucose formation;
- adrenocorticotropic hormone of the pituitary gland, activating the production of catecholamines and cortisol.
The thyroid hormone thyroxine has a minor effect on carbohydrate metabolism. An imbalance in the qualitative and quantitative production of hormones leads to disruption of the stability of blood sugar levels and the development of pathologies.
Symptoms and first signs
The disease can develop in a child at any age. There are two peak periods - 5-8 years and puberty, when growth and metabolism are enhanced.
The disease of the first type manifests itself acutely. Signs of type 1 diabetes in children are : severe weakness and dizziness when hungry and full . From the onset of the first symptoms to a diabetic coma can take from 1 to 3 months. Source: ISPAD Clinical Practice Consensus Guidelines 2009 Compendium. Pediatric Diabetes. 2009; 10 (Suppl. 12): 210
The first signs of the development of diabetes mellitus in children:
- increased urination (over 2 liters per day);
- thirst and dry mouth;
- increased appetite with a sharp decrease in body weight;
- severe course of infectious diseases;
- rapid fatigue without exercise;
- absent-minded attention;
- increased blood glucose (exceeds 120 mg) in the analysis;
- rapid decrease in visual acuity;
- nausea and vomiting.
Parents may notice that the urine has become sticky, and starched stains remain on their underwear. Dryness of the mucous membranes and epidermis may be observed - peeling of the skin on the soles and palms. Symptoms of diabetes mellitus in children include irritation in the corners of the mouth (“seizures”) and stomatitis. Pustules, boils, and diaper rash appear. In girls, the development of the disease is accompanied by vulvitis, in boys – by balanoposthitis. If the disease first appears during a girl’s puberty, it can cause menstrual irregularities.
It is difficult to identify symptoms in children, so they pay attention to accompanying manifestations. Young children are characterized by nocturnal enuresis, itching, restlessness, and digestive problems. When sick, an infant greedily drinks milk and water. The sweet, sticky urine makes the diapers hard. Such signs indicate a moderate to severe form of pathology. In mild forms, the disease is diagnosed by blood and urine tests.
Advanced Diagnostics
If the initial blood test reveals an increase in sugar levels, the child needs to undergo additional examination. Advanced diagnostics include GTT (glucose tolerance test). The glucose tolerance test is a double blood draw for glycemic testing: initially on an empty stomach, and again two hours after the “sugar load”.
An aqueous solution of glucose acts as a load. For adolescents aged 12+, dilute 70 ml of the substance in 200 ml of water. For children under 12 years of age, the glucose dose is halved while maintaining the water norm. Testing allows you to determine the degree of glucose absorption in the body.
Glucose tolerance test results
Determination of the level of HbA1C (glycated hemoglobin) is prescribed. Glycated (glycated) hemoglobin is formed by the interaction of hemoglobin and glucose and remains in the body for 120 days. The analysis makes it possible to track glycemia in retrospect for 3 months. The concentration of antibodies to glutamate decarboxylase (GAD antibodies) is also analyzed. In juvenile diabetes it always gives a positive result (antibodies are detected).
When the diagnosis is confirmed by the results of blood microscopy, the child is prescribed a urine test for the presence of glucose and acetone in it (glucosuria and acetonuria).
Rules for preparing a child for blood sampling
The collection procedure is carried out in laboratory conditions. Blood for analysis is taken from a vein or finger. In newborn babies, biofluid (blood) is most often taken from the heel. Sugar values of capillary and venous blood can differ in the range of up to 12%, which is not a pathology and is taken into account when comparing with standards.
The main condition is to take the test on an empty stomach. This is explained by the body's physiological ability to release glucose into the blood immediately after eating and maintain its elevated level for about three hours. If your child eats breakfast before the test, blood sugar is guaranteed to be elevated. Blood microscopy for sugar is performed exclusively on an empty stomach!
Preparatory measures include fasting for 8 hours before the procedure, no sweets in the evening menu on the eve of the test, refusal of morning oral hygiene, and a full night's sleep. Before visiting the laboratory, you are prohibited from chewing gum or drinking sweet soda or juice (plain water is allowed in any reasonable quantity). Incorrect preparation of the child for the analysis procedure leads to distortion of the data obtained.
Diagnosis of diabetes mellitus
The first person to identify symptoms of the disease is the pediatrician who observes the child. The doctor pays attention to the classic signs: increased urination, feelings of thirst, hunger and weight loss.
During the examination, the doctor may notice diabetic blush, decreased skin turgor and a crimson tongue. If symptoms of diabetes are detected, the pediatrician transfers the patient to an endocrinologist for treatment and observation.
To make an accurate diagnosis, the child is sent for laboratory testing. It is necessary to take a blood test to check your sugar level; daily monitoring is used. They also check insulin, proinsulin, glucose tolerance, level of glycosylated hemoglobin, blood CBS.
Blood test results table
| results | Capillary blood glucose (mmol/l) | |
| on an empty stomach | 2 hours after taking glucose | |
| Norm | <5,5 | <7,8 |
| Impaired glucose tolerance | <6,1 | 7,8-11,1 |
| Diabetes | >6,1 | >11,1 |
The urine is tested for glucose and ketone bodies. The criteria for identifying the disease are: glycosuria, hyperglycemia, acetonuria, ketonuria.
As part of the preclinical detection of type 1 pathology in genetically predisposed children, Abs to glutamate decaboxylase and β-cells are determined. The structure of the gland is assessed using ultrasound.
Based on the patient’s complaints, urine and blood test results, and research results, the doctor makes a diagnosis.
Normal blood sugar values in children
Laboratory sugar levels are calculated in millimoles per liter (mmol/l). In adults, the upper limit of normal is 5.5 mmol/l, the lower is 3.3 mmol/l. Indicators from 4.2 to 4.6 mmol/l are considered optimal. Due to the characteristics of metabolism in a child’s body, reference values are distributed by age group.
Sugar levels in children on an empty stomach (in mmol/l)
| Baby up to a month | Child under one year old | Preschooler up to 5 years old | Schoolchild under 14 years old |
| 2,8 – 4,3 | 2,8 – 4,4 | 3,3 – 5,0 | 3,3 – 5,3 (5,5) |
The equalization of children's and adult indicators occurs at puberty. Deviations from reference values in the direction of decrease are called hypoglycemia, and in the direction of increase - hyperglycemia. In addition to age, sugar levels are directly affected by nutrition, psycho-emotional state, weight, physical activity, the presence of chronic pathologies and infectious viral diseases. There is no significant difference between boys and girls in terms of gender.
Treatment of the disease
When a diagnosis is made, the doctor, in accordance with clinical recommendations, prescribes observation and examination of the child every month. Monitoring the condition allows you to make adjustments to therapy, prevent exacerbations and prevent the pathology from becoming severe.
Treatment of diabetes in children includes medications, special exercise and diet. Source: I.I. Dedov, V.A. Peterkova, T.L. Kuraeva Russian consensus on the treatment of diabetes mellitus in children and adolescents // Pediatrics, 2010, v. 89, no. 5, pp. 6-14
- Proper nutrition. The specialist develops a balanced diet in terms of calories and nutritional supplements. A complex of vitamins is required. The diet should limit the consumption of baked goods and potato dishes. Unsweetened fruits and vegetables can be eaten in any quantity. The child needs to be provided with 6 fractional meals a day.
- Exercise helps lower glucose levels and improve insulin sensitivity. The load must be accurately dosed and selected by the attending physician. During and after exercise, you need to take carbohydrates.
- Medicines. Children are prescribed medications with insulin. In most cases, a single dose every day is sufficient. The doctor selects the dose and administration schedule. In addition to the main treatment or for mild diabetes mellitus in children, tablets are indicated.
Parental responsibilities
Regardless of the reason for the increase in sugar, the child needs treatment. The responsibilities of parents include creating comfortable living conditions and constant monitoring of the therapy. Necessary:
- purchase a glucometer with test strips and kitchen scales;
- monitor glycemia several times a day;
- do not violate the insulin treatment regimen;
- organize proper nutrition and systematic sports activities;
- regularly take your child to an endocrinologist for control and preventive examinations;
- provide psychological support and assistance.
To facilitate adaptation to the disease, endocrinologists strongly recommend attending classes at the Diabetes School. Children with a hereditary predisposition to diabetes need to begin prevention from the moment they are born. A child prone to hyperglycemia or diagnosed with diabetes needs to be properly explained which foods are strictly contraindicated for him and for what reason.
Disease prevention
No specific prevention has been developed for children with diabetes. For people at risk, it is important to maintain a normal weight, ensure daily physical activity, improve immunity, and be examined by an endocrinologist twice a year.
Timely vaccination helps prevent the development of diseases that are caused by diabetes: measles, mumps.
It is necessary to ensure that the child drinks sufficient amounts of liquid - at least 2 liters, in addition to tea and juices.
It is necessary to protect the child from stress; if there is excessive anxiety, it is better to consult a specialist.
Ways to reduce indicators
Hyperglycemia in children is compensated, first of all, by adjusting the diet. The condition of impaired glucose tolerance (prediabetes) is reversible. To prevent the development of diabetes, it is enough to review your diet and diet. If sugar levels are high, it is recommended to switch the child to a diet designed for diabetics.
If the juvenile type of the disease is confirmed, the child will receive lifelong treatment with medical insulin and a diabetic diet. The dosage of medications and the treatment regimen are determined by an endocrinologist. Insulin injections are carried out according to an individual schedule determined by the doctor. Short- and long-acting medical insulins are used for treatment.
Nutrition
A small patient is prescribed the “Table No. 9” diet, which helps maintain a stable glycemic level and prevent the early development of diabetic complications. Products containing large amounts of fast carbohydrates should be excluded from the menu:
- ice cream, cakes and other confectionery products;
- sweet pastries, jam, sweets;
- fruits: papaya, guava, carom, bananas, pineapples, figs;
- drinks: packaged juices, sweet soda, bottled tea.
The menu is based on protein products (dietary poultry, fish, mushrooms, eggs) and complex carbohydrates, which are slowly processed in the body. Slow carbohydrates include legumes, grains, and vegetables. Potatoes are allowed on a limited basis.
All foods for the diet are selected taking into account their glycemic index (GI), which indicates the rate at which glucose formed during the digestion of food enters the blood. In case of hyperglycemia, foods indexed from 0 to 30 are allowed; foods with an index from 30 to 70 are limited. A glycemic index of more than 70 is not allowed on the menu.
Brief table of products with index
Physical activity
A prerequisite for the treatment of diabetes and pre-diabetic conditions is participation in feasible sports. The load must correspond to the child’s physical capabilities and have a regular basis.
Effective treatment at SM-Clinic
Our medical center employs the best endocrinologists in St. Petersburg. At an appointment with a specialist, you will receive qualified assistance - we will accurately diagnose and prescribe treatment. To schedule a consultation, call us at the numbers provided. The doctor will answer your questions about the diagnosis, treatment and prevention of diabetes.
Sources:
- A.B. Resnenko. Type 2 diabetes mellitus in children and adolescents: from pathogenesis to treatment // Pediatric pharmacology, 2011, vol. 8, no. 4, pp. 125-129.
- P.F. Litvitsky, L.D. Maltseva. Disorders of carbohydrate metabolism in children: diabetes mellitus // Issues of modern pediatrics, 2021, vol. 16, no. 6, pp. 468-480.
- ISPAD Clinical Practice Consensus Guidelines 2009 Compendium. Pediatric Diabetes. 2009; 10 (Suppl. 12): 210.
- I.I. Dedov, V.A. Peterkova, T.L. Kuraeva. Russian consensus on the treatment of diabetes mellitus in children and adolescents // Pediatrics, 2010, v. 89, no. 5, pp. 6-14.
Astratenkov Oleg Gennadievich Clinic Author of the article
Astratenkov Oleg Gennadievich
Doctor of the highest qualification category
Specialty: endocrinologist
Experience: 19 years
The information in this article is provided for reference purposes and does not replace advice from a qualified professional. Don't self-medicate! At the first signs of illness, you should consult a doctor.
Type 1 diabetes mellitus in children and adolescents: etiopathogenesis, clinical picture, treatment
Diabetes mellitus (DM) is an etiologically heterogeneous group of metabolic diseases that are characterized by chronic hyperglycemia caused by impaired secretion or action of insulin or a combination of these disorders.
DM was first described in ancient India more than 2 thousand years ago. Currently, there are more than 230 million patients with diabetes in the world, in Russia - 2,076,000. In reality, the prevalence of diabetes is higher, because its latent forms are not taken into account, i.e., there is a “non-infectious pandemic” of diabetes.
Classification of diabetes
According to the modern classification there are [1]:
- Type 1 diabetes mellitus (type 1 diabetes), which is more common in childhood and adolescence. There are two forms of this disease: a) autoimmune type 1 diabetes (characterized by immune destruction of β-cells - insulitis); b) idiopathic type 1 diabetes, also occurring with destruction of β-cells, but without signs of an autoimmune process.
- Diabetes mellitus type 2 (DM 2), characterized by relative insulin deficiency with impairment of both insulin secretion and action (insulin resistance).
- Specific types of diabetes.
- Gestational diabetes mellitus.
The most common types of diabetes are type 1 diabetes and type 2 diabetes. For a long time, it was believed that type 1 diabetes was common in childhood. However, research over the past decade has shaken this assertion. Type 2 diabetes has become increasingly diagnosed in children, which predominates in adults after 40 years of age. In some countries, type 2 diabetes is more common in children than type 1 diabetes, due to genetic characteristics of the population and the increasing prevalence of obesity.
Epidemiology of diabetes
The established national and regional registries of type 1 diabetes in children and adolescents have revealed wide variability in incidence and prevalence depending on the population and geographic latitude in different countries of the world (from 7 to 40 cases per 100 thousand children per year). Over the past two years For decades, the incidence of type 1 diabetes among children has been steadily increasing. A quarter of patients are under four years of age. At the beginning of 2010, 479.6 thousand children with type 1 diabetes were registered in the world. The number of newly identified patients is 75,800. The annual increase is 3%.
According to the State Register, as of January 1, 2011, 17,519 children with type 1 diabetes were registered in the Russian Federation, of which 2,911 were new cases. The average incidence rate of children in the Russian Federation is 11.2 per 100 thousand children's population [1]. The disease manifests itself at any age (congenital diabetes exists), but most often children fall ill during periods of intensive growth (4–6 years, 8–12 years, puberty). Infants are affected in 0.5% of cases of diabetes.
Unlike countries with a high incidence rate, in which the maximum increase occurs in younger ages, in the Moscow population the increase in incidence is observed due to adolescents.
Etiology and pathogenesis of type 1 diabetes
Type 1 diabetes is an autoimmune disease in genetically predisposed individuals, in which chronic lymphocytic insulitis leads to the destruction of β-cells, followed by the development of absolute insulin deficiency. Type 1 diabetes is characterized by a tendency to develop ketoacidosis.
Predisposition to autoimmune type 1 diabetes is determined by the interaction of many genes, and the mutual influence of not only different genetic systems is important, but also the interaction of predisposing and protective haplotypes.
The period from the onset of the autoimmune process to the development of type 1 diabetes can take from several months to 10 years.
Viral infections (coxsackie B, rubella, etc.) and chemicals (alloxan, nitrates, etc.) can take part in triggering the processes of destruction of islet cells.
Autoimmune destruction of β-cells is a complex, multi-stage process, during which both cellular and humoral immunity are activated. The main role in the development of insulitis is played by cytotoxic (CD8+) T-lymphocytes [2].
According to modern concepts, immune dysregulation plays a significant role in the occurrence of the disease from the onset to the clinical manifestation of diabetes.
Markers of autoimmune destruction of β-cells include:
1) islet cell cytoplasmic autoantibodies (ICA); 2) anti-insulin antibodies (IAA); 3) antibodies to islet cell protein with a molecular weight of 64 thousand kDa (they consist of three molecules):
- glutamate decarboxylase (GAD);
- tyrosine phosphatase (IA-2L);
- tyrosine phosphatase (IA-2B). Frequency of occurrence of various autoantibodies in the onset of type 1 diabetes: ICA - 70-90%, IAA - 43-69%, GAD - 52-77%, IA-L - 55-75%.
In the late preclinical period, the population of β-cells decreases by 50–70% compared to the norm, and the remaining ones still maintain the basal level of insulin, but their secretory activity is reduced.
Clinical signs of diabetes appear when the remaining number of β-cells is unable to compensate for increased insulin requirements.
Insulin is a hormone that regulates all types of metabolism. It provides energy and plastic processes in the body. The main target organs of insulin are the liver, muscle and adipose tissue. In them, insulin has anabolic and catabolic effects.
The effect of insulin on carbohydrate metabolism
- Insulin ensures the permeability of cell membranes to glucose by binding to specific receptors.
- Activates intracellular enzyme systems that provide glucose metabolism.
- Insulin stimulates the glycogen synthetase system, which ensures the synthesis of glycogen from glucose in the liver.
- Suppresses glycogenolysis (the breakdown of glycogen into glucose).
- Suppresses gluconeogenesis (synthesis of glucose from proteins and fats).
- Reduces blood glucose concentration.
The effect of insulin on fat metabolism
- Insulin stimulates lipogenesis.
- It has an anti-lipolytic effect (inside lipocytes it inhibits adenylate cyclase, reduces cAMP of lipocytes, necessary for lipolysis processes).
Lack of insulin causes increased lipolysis (the breakdown of triglycerides into free fatty acids (FFA) in adipocytes). An increase in the amount of FFA causes fatty infiltration of the liver and an increase in its size. The breakdown of FFAs increases with the formation of ketone bodies.
The effect of insulin on protein metabolism
Insulin promotes protein synthesis in muscle tissue. Insulin deficiency causes breakdown (catabolism) of muscle tissue, accumulation of nitrogen-containing products (amino acids) and stimulates gluconeogenesis in the liver [3].
Insulin deficiency increases the release of contrainsular hormones, activation of glycogenolysis, and gluconeogenesis. All this leads to hyperglycemia, increased blood osmolarity, tissue dehydration, and glycosuria.
The stage of immunological dysregulation can last for months and years, and antibodies can be detected that are markers of autoimmunity to β-cells (ICA, IAA, GAD, IA-L) and genetic markers of type 1 diabetes (predisposing and protective HLA haplotypes, which relative risk may differ among different ethnic groups).
Latent diabetes mellitus
At this stage of the disease there are no clinical symptoms. The fasting blood glucose level can periodically range from 5.6 to 6.9 mmol/l, and during the day remains within normal limits; there is no glucose in the urine. Then a diagnosis of “impaired fasting glucose (IFG)” is made.
If, when performing an oral glucose tolerance test (OGTT) (using glucose at a dose of 1.75 g/kg body weight up to a maximum dose of 75 g), the blood glucose level is > 7.8 but < 11.1 mmol/l, then the diagnosis is made "impaired glucose tolerance."
Some children experience spontaneous hypoglycemia after exercise or on an empty stomach before diabetes is diagnosed. In addition to the increased need for sweets, at the onset of the disease there may be general weakness, pallor, and sweating. They are likely due to β-cell dysfunction, which results in the release of inappropriate amounts of insulin, accompanied by symptoms of hypoglycemia.
Impaired glucose tolerance and impaired fasting glucose are intermediate stages between carbohydrate metabolism disorder and diabetes mellitus.
Overt diabetes mellitus
Phases of the course of type 1 diabetes:
1) decompensation without ketoacidosis; 2) decompensation with ketoacidosis; 3) diabetic ketoacidotic coma:
- I degree - doubtfulness;
- II degree - stupor;
- III degree - actual coma (loss of consciousness).
Decompensation phase without ketosis
In children, type 1 diabetes often develops acutely. But this is preceded by symptoms such as polydipsia (thirst), polyuria, pollakiuria, polyphagia, and weight loss. Polyuria is the first manifest symptom of glucosuria. Polyuria develops as a result of osmotic diuresis caused by a high concentration of glucose in the urine (above the renal threshold of 9 mmol/l). The amount of urine per day rarely exceeds 3 liters. Nocturnal enuresis and the presence of “sweet” spots on the floor in young children often attract parents.
Polydipsia is associated with plasma hyperosmolarity and polyuria. Constant thirst day and night is compensatory in nature.
Polyphagia (increased appetite) is caused by impaired utilization of glucose by cells - the latter starve.
Weight loss is a symptom characteristic of type 1 diabetes; it is called “skinny” diabetes. The patient’s sharp weight loss is associated with the failure of glucose to be absorbed by cells, increased lipolysis and proteolysis processes in conditions of insulin deficiency, as well as due to dehydration of the body.
Early signs of diabetes mellitus may be itching of the skin in the area of the external genitalia (vulvitis in girls, balanitis in boys).
At the height of the disease, the skin is dry, flaky, and turgor is reduced. The liver is often enlarged in size (fatty infiltration). The acid-base composition (ABC) or blood pH is 7.35–7.45 (normal), there are no ketone bodies in the urine.
Decompensation phase with ketoacidosis
Diabetic ketoacidosis develops as a result of late diagnosis or improper treatment of an already diagnosed disease. Clinical signs of this condition are diabetic flushing on the face, increasing thirst, polyuria, weight loss, decreased appetite, nausea, vomiting, the smell of acetone on the breath, abdominal pain, and headache. Important laboratory signs of this phase are acidosis and ketonuria.
Diabetic coma
The most severe manifestation of ketoacidosis is the development of diabetic ketoacidotic coma. For practical reasons, the latter is divided into coma I–III degrees (I–II degrees are a precomatous state, III degree is the actual coma).
First-degree coma is characterized by drowsiness, as well as muscle adynamia, severe thirst, nausea, occasional vomiting, moderately reduced reflexes, tachycardia, blood pH 7.25–7.15.
Stupor (hibernation) is typical for second-degree coma. The patient can be woken up, he answers simple questions and immediately falls asleep. Breathing is noisy, deep, ketoacidotic (Kussmaul), the smell of acetone in the exhaled air is felt at a distance. Adynamia is pronounced, reflexes are suppressed. Heart sounds are muffled, blood pressure is low, blood pH is 7.15–7.0.
In a third degree coma there is no consciousness. Severe dehydration, the mucous membranes of the mouth are brightly dry, the tongue is coated with a thick brown coating, vomit is the color of coffee grounds. The skin is dry with a grayish tint, peels, and gathers in folds. The pulse is thready, heart sounds are muffled. Due to severe dehydration, oligoanuria develops, blood pH less than 7.0. In the lactic acid variant of diabetic coma, sharp pain in the chest, heart, muscles, and abdomen may predominate. There is a rapid appearance and increase in shortness of breath, ketosis is absent or weakly expressed, hyperglycemia is moderate (up to 15–17 mmol/l).
When ketoacidotic coma is combined with hyperosmolarity, severe dehydration, agitation, hyperreflexia, hyperthermia, focal neurological symptoms, pathological reflexes, convulsions, hyperglycemia above 30 mmol/l are characteristic. Possible increases in sodium and urea in the blood, ketosis and acidosis [4].
Laboratory diagnostics
The main laboratory sign of diabetes is hyperglycemia. The normal glucose content in capillary blood on an empty stomach is:
- in newborns 1.6–4.0 mmol/l;
- in infants 2.8–4.4 mmol/l;
- in children of early and school age 3.3–5.0 mmol/l.
Criteria for the diagnosis of diabetes mellitus (ISPAD, 2009)
- Symptoms of diabetes in combination with the random detection of a glucose concentration > 11.1 mmol/l.
- Fasting plasma glucose level > 7.0 mmol/l.
- Glucose level 2 hours after exercise > 11.1 mmol/l [5].
In a healthy person, there is no glucose in the urine. Glucosuria occurs when glucose levels are above 8.88 mmol/l.
Ketone bodies (acetoacetate, β-hydroxybutyrate and acetone) are formed in the liver from free fatty acids. Their increase is observed with insulin deficiency. Test strips are available to measure urinary acetoacetate and blood β-hydroxybutyrate levels (>0.5 mmol/L). In the decompensation phase of type 1 diabetes without ketoacidosis, there are no acetone bodies and acidosis.
Glykylated hemoglobin. In the blood, glucose irreversibly binds to the hemoglobin molecule to form glycated hemoglobin (total HBA1 or its “C” fraction HBA1c), i.e., it reflects the state of carbohydrate metabolism over 3 months. The normal level of HBA1 is 5–7.8%, the level of the minor fraction (HBA1c) is 4–6%. With hyperglycemia, glycated hemoglobin levels are high.
Immunological markers of autoimmune insulitis: autoantibodies to β-cell antigens (ICA, IAA, GAD, IA-L) may be elevated. The content of C-peptide in the blood serum is low.
Differential diagnosis
To this day, the diagnosis of type 1 diabetes remains relevant. More than 80% of children with diabetes are diagnosed in a state of ketoacidosis. Depending on the prevalence of certain clinical symptoms, it is necessary to differentiate with:
1) surgical pathology (acute appendicitis, “acute abdomen”); 2) infectious diseases (flu, pneumonia, meningitis); 3) diseases of the gastrointestinal tract (food poisoning, gastroenteritis, etc.); 4) kidney diseases (pyelonephritis); 5) diseases of the nervous system (brain tumor, vegetative-vascular dystonia); 6) diabetes insipidus.
When the disease develops gradually and slowly, the differential diagnosis is between type 1 diabetes, type 2 diabetes and adult-onset diabetes of the young (MODY).
Treatment of type 1 diabetes mellitus
Type 1 diabetes develops as a result of absolute insulin deficiency. All patients with manifest form of type 1 diabetes undergo insulin replacement therapy.
In a healthy person, insulin secretion constantly occurs regardless of food intake (basal). But in response to food intake, its secretion increases (bolus) in response to post-alimentary hyperglycemia. Insulin is secreted by β cells into the portal system. 50% of it is consumed in the liver to convert glucose into glycogen, the remaining 50% is carried throughout the systemic circulation to the organs.
In patients with type 1 diabetes, exogenous insulin is administered subcutaneously, and it slowly enters the general bloodstream (not into the liver, as in healthy people), where its concentration remains high for a long time. As a result, their post-nutrition glycemia is higher, and in the late hours there is a tendency to hypoglycemia.
On the other hand, glycogen in patients with diabetes is primarily deposited in the muscles, and its reserves in the liver are reduced. Muscle glycogen is not involved in maintaining normoglycemia.
In children, human insulins obtained by a biosynthetic (genetically engineered) method using recombinant DNA technology are used.
The dose of insulin depends on age and duration of diabetes. In the first 2 years, the insulin requirement is 0.5–0.6 IU/kg body weight per day. Currently, the most widespread is the intensified (bolus-basal) insulin administration regimen [6].
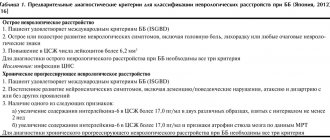
Insulin therapy begins with the administration of ultra-short or short-acting insulin (Table 1). The first dose in children of the first years of life is 0.5–1 IU, in schoolchildren 2–4 IU, in adolescents 4–6 IU. Further adjustment of the insulin dose is carried out depending on the level of glucose in the blood. When metabolic parameters are normalized, the patient is transferred to a bolus-basic regimen, combining short- and long-acting insulins.
Insulins are available in vials and cartridges. Insulin syringe pens are the most widely used.
To select the optimal dose of insulin, a continuous glucose monitoring system (CGMS) has been widely used. This mobile system, worn on the patient's belt, records blood glucose levels every 5 minutes for 3 days. These data are subjected to computer processing and presented in the form of tables and graphs, which indicate fluctuations in glycemia.
Insulin pumps. This is a mobile electronic device worn on the belt. The computer-controlled (chip) insulin pump contains short-acting insulin and is delivered in two modes, bolus and basal [7].
Diet
An important factor in compensating for diabetes is diet. The general principles of nutrition are the same as for a healthy child. The ratio of proteins, fats, carbohydrates, calories should correspond to the age of the child.
Some dietary features for children with diabetes:
- Reduce, and in young children completely eliminate, refined sugar.
- It is recommended to record meals.
- The diet should consist of breakfast, lunch, dinner and three snacks 1.5–2 hours after main meals.
The sugar-raising effect of food is mainly determined by the quantity and quality of carbohydrates.
According to the glycemic index, foods that increase blood sugar levels very quickly (sweet foods) are identified. They are used to relieve hypoglycemia.
- Products that quickly increase blood sugar (white bread, crackers, cereals, sugar, sweets).
- Foods that moderately increase blood sugar (potatoes, vegetables, meat, cheese, sausages).
- Foods that slowly increase blood sugar (rich in fiber and fat, such as brown bread, fish).
- Foods that do not increase blood sugar are vegetables [1].
Physical exercise
Physical activity is an important factor regulating carbohydrate metabolism. During physical activity in healthy people, there is a decrease in insulin secretion with a simultaneous increase in the production of contrainsular hormones. The liver increases the production of glucose from non-carbohydrate compounds (gluconeogenesis). This serves as an important source of glucose during physical activity and is equivalent to the degree of glucose utilization by muscles.
Glucose production increases as the intensity of exercise increases. Glucose levels remain stable.
In type 1 diabetes, the effect of exogenous insulin does not depend on physical activity, and the effect of counter-insular hormones is not enough to correct glucose levels. In this regard, hypoglycemia may occur during or immediately after physical activity. Almost all forms of physical activity lasting more than 30 minutes require adjustments in diet and/or insulin dosage.
Self-control
The goal of self-control is to teach the diabetic patient and his family members to help themselves independently. It includes [8]:
- general concepts about diabetes;
- ability to determine glucose using a glucometer;
- Correctly adjust the insulin dose;
- count grain units;
- ability to recover from a hypoglycemic state;
- keep a self-control diary.
Social adaptation
When a child is diagnosed with diabetes, parents are often at a loss, as the disease affects the family’s lifestyle. Problems arise with ongoing treatment, nutrition, hypoglycemia, and concomitant diseases. As the child grows, he develops his own attitude towards the disease. During puberty, numerous physiological and psychosocial factors make glucose control more difficult. All this requires comprehensive psychosocial assistance from family members, an endocrinologist and a psychologist.
Target levels of carbohydrate metabolism indicators in patients with type 1 diabetes (Table 2)
Fasting (preprandial) blood sugar is 5–8 mmol/l.
2 hours after a meal (postprandial) 5–10 mmol/l.
Glycated hemoglobin (HBA1c) < 7.5%.
The study of glucosuria has practically faded into the background due to the advent of glucometers.
An important indicator of diabetes compensation is the absence of frequent hypoglycemia.
Treatment of diabetic ketoacidotic coma
Treatment of a patient with a diabetic coma is carried out in the intensive care unit. The main therapeutic measures are infusion therapy and intravenous insulin.
During the treatment process it is necessary:
1) eliminate dehydration and hypovolemia; 2) balance blood pH; 3) normalize the electrolyte balance of the blood; 4) reduce hyperglycemia and maintain it at an optimal level; 5) prevent the development of complications; 6) treat concomitant diseases.
The main infusion solutions are crystalloids (saline, Ringer's solution) using glucose-containing solutions. To eliminate potassium deficiency, a solution of potassium chloride is used. The optimal blood glucose level in the first 1–2 days is 12–15 mmol/l. A glycemic level below 8 mmol/l against the background of severe ketoacidosis is dangerous due to the development of a hypoglycemic state.
Insulin therapy is an essential component of the treatment of diabetic coma. Only intravenous administration of short- and ultra-short-acting insulin is used. Insulin is administered as an intravenous bolus every 1–2 hours or added to the infusion medium. This ranges from 1-2 to 4-6 units per hour depending on the child’s age and blood sugar level.
In addition, the following are added to infusion solutions: heparin, cocarboxylase, ascorbic acid, panangin, calcium and magnesium preparations.
Infusion therapy is completed after stabilization of the patient’s condition, the ability to take fluids and food independently, stable normalization of blood pH, and the absence of complications requiring its continuation [5, 6].
Hypoglycemia
Hypoglycemia is the most common complication of type 1 diabetes. Occurs in more than 90% of patients. Hypoglycemia develops as a result of a discrepancy between the dose of insulin, food consumed and physical activity.
The hypoglycemic state that precedes hypoglycemic coma is clinically manifested by an acute feeling of hunger, tremor, pale skin, cold sweat, tachycardia, anxiety, fear, irritability, inappropriate behavior, nightmares, etc.
If the symptoms of a hypoglycemic state are not eliminated in a timely manner, it can quickly develop into a hypoglycemic coma. The patient develops trismus of the jaws, confusion, and then loss of consciousness and convulsions. Hypoglycemic coma against the background of ketoacidosis threatens the development of edema and swelling of the brain with a fatal outcome.
Treatment of hypoglycemic conditions consists of immediate ingestion of rapidly absorbed carbohydrates - glucose, sugar, sweets, juice, cookies, etc. When you feel better, take complex carbohydrates (fruits, bread, milk).
In case of hypoglycemic coma: the patient should be immediately given intramuscular glucagon 0.5–1.0 mg or intravenously a glucose solution 10–20% 20–40 ml, dexamethasone.
Specific complications of type 1 diabetes
These include microangiopathies. Vascular complications are associated with impaired microcirculation, blood coagulation and fibrinolytic systems, antioxidant defense system, and glycosylation of the vascular wall. Depending on the damage to the organ, they speak of diabetic nephropathy, diabetic retinopathy, diabetic neuropathy, etc.
Other complications with long-term uncompensated type 1 diabetes may include cataracts, limited joint mobility (diabetic hairopathy), necrobiosis lipoidica of the skin, Mauriac syndrome (retardation in physical and sexual development, enlarged liver).
In the last decade, type 2 diabetes mellitus has been increasing in childhood [9]. This is believed to be due to the increasing prevalence of obesity in youth, which is reaching epidemic proportions in the United States. The rapid development of molecular genetics has made it possible to identify monogenic forms of diabetes mellitus associated with mutations in genes that control β-cell function [10]. This is the so-called MODY diabetes.
Clinical observation for diabetes in children
It is carried out by a pediatrician and endocrinologist and includes home management, training of parents and children in methods of diabetes compensation. Periodic (every 6–12 months) examinations and adjustment of insulin doses. Criteria for the effectiveness of observation are normalization of carbohydrate metabolism, absence of acute conditions and vascular complications, normal liver size, correct sexual and physical development. Currently, curing a patient with type 1 diabetes is impossible, but with long-term stable compensation, the prognosis for life and work ability is favorable; it significantly worsens in the presence of vascular complications.
Prevention of diabetes in children
It consists of medical and genetic counseling in families of patients with diabetes. Determination of predisposing and protective genes and their combinations, immunological studies (ICA, IAA, GAD, IA-L), hormonal metabolic status (OGTT, C-peptide, immunoreactive insulin, glycated hemoglobin).
New technologies in the diagnosis and treatment of type 1 diabetes
- Glucose monitoring tools: Continuous Glucose Monitoring System, CGMS. It is attached to the belt and uses a subcutaneous sensor (changes every 3 days) to monitor blood glucose levels.
- Insulin pump: A small computer that delivers rapid-release insulin continuously through a small plastic catheter into the subcutaneous fat.
- "Artificial pancreas": a device that combines a continuous blood glucose monitoring system and an insulin pump. This treatment method will create conditions to fully reproduce the function of β-cells.
Literature
- Dedov I. I., Kuraev T. K., Peterkova V. A. Diabetes mellitus in children and adolescents. Hand-in. 2nd ed. GEOTAR-Media, 2013, 272 p.
- Balabolkin M.I., Klebanova E.M., Kreminskaya V.M. Differential diagnosis and treatment of endocrine diseases. Handbook M.: Medicine, 2002, 752 p.
- Endocrinology and metabolism. T. 2. Translation from English. edited by F. Fleming, J. D. Baxter, A. E. Broadus, L. A. Fromen. M.: Medicine, 1985. 416 p.
- Treatment of diabetic coma in children. Methodological recommendations No. 16 DZM, M., 2006. 14 p.
- ISPAD Clinical Practice Consensus Guidelines. 2009. Vol. 10, suppl. 12.210 p.
- Dedov I.I., Peterkova V.A., Kuraev T.L. Russian consensus on the treatment of diabetes mellitus in children and adolescents // Pediatrics. 2010, no. 5, p. 1–8.
- Peterkova V. A., Emelyanov A. O., Kuraeva T. L. The use of insulin pumps in children and adolescents with diabetes: a manual for doctors / Ed. I. I. Dedova, M.: Institute of Healthcare Management Problems, 2009. 32 p.
- Algorithms for specialized medical care for patients with diabetes mellitus / Ed. I. I. Dedova and M. V. Shestokova. 4th ed. Vol. 4. M., 2009: 101.
- Miller J., Silverstein JH, Rosenblook AL Type 2 diabetes in adolescents. Lifshits F., Marcel Dekker, 2007. P. 169–188.
- Kuraeva T. L., Zilberman L. I., Titovich E. V., Peterkova V. A. Genetics of monogenic forms of diabetes mellitus // Diabetes mellitus. 2011, No. 1, p. 20–27.
V. V. Smirnov1, Doctor of Medical Sciences, Professor A. A. Nakula
GBOU VPO RNIMU im. N. I. Pirogova Ministry of Health of the Russian Federation, Moscow
1 Contact information
Prices
| Name of service (price list incomplete) | Price |
| Appointment (examination, consultation) with a pediatric endocrinologist, primary, therapeutic and diagnostic, outpatient | 1750 rub. |
| Consultation (interpretation) with analyzes from third parties | 2250 rub. |
| Prescription of treatment regimen (for up to 1 month) | 1800 rub. |
| Prescription of treatment regimen (for a period of 1 month) | 2700 rub. |
| Consultation with a candidate of medical sciences | 2500 rub. |
What happens in the body
In children with diabetes, when there is a high level of glucose in the body, some dehydration of the internal organs occurs.
The body, trying to dilute the blood, takes fluid from the cells of all tissues, which makes the child constantly thirsty. Thus, increased blood sugar in children affects the urinary system, since fluid consumed in large quantities must be eliminated. Frequent urge to urinate should attract the attention of parents and teachers, because the child is forced to leave the toilet during lessons. Constant dehydration of the body negatively affects vision, since in this case the lenses of the eyes are primarily affected. This leads to blurred vision and a feeling of fog in the eyes.
Over time, the body loses the ability to use glucose as an energy source and begins to burn fat. In such cases, the child rapidly loses weight.
In addition, parents should pay attention to the constant weakness that appears due to lack of insulin. As a result, glucose is not able to be transformed into the necessary energy.
Increased blood sugar in children leads to the body being unable to saturate and absorb food normally. Therefore, patients suffering from diabetes are more likely to experience a constant feeling of hunger. But if appetite decreases, this may indicate diabetic ketoacidosis.