What it is
Arrhythmia is a violation of the regularity and sequence of heart contractions.
Everything that is not sinus rhythm is called this term and includes various pathologies of impulse formation and its conduction. But few ordinary people know this, and it is believed that if a patient told the doctor: “I have an arrhythmia!”, then he understood everything and would immediately solve the problem by prescribing one specific medicine. Alas, everything is not so simple.
There is more than one classification of arrhythmias, but since my task is to introduce readers to the diversity and help them understand it themselves, and not to give a lecture to cardiologists, I will divide them into 2 groups:
- violation of impulse formation - here we include extrasystoles and tachycardias;
- pathology of the same signal - blockade and bradyarrhythmia.
How does normal heart contraction occur? Normally, the sinus node dominates - a power plant that generates impulses and transmits them further through the internodal pathways to the atrioventricular node, from which the signal goes along the His bundle, to its right and left branches, to the Purkinje fibers and to the ventricular myocardium.
Causes of arrhythmias
There are three groups of reasons:
- cardiac - when there is cardiovascular pathology: coronary disease, hypertension, heart disease, myocarditis, pericarditis, cardiomyopathy, and so on;
- extracardiac – these include diseases of other organs and systems (chronic bronchitis, pathologies of the thyroid gland, gastrointestinal tract), taking medications (antiarrhythmics, sympathomimetics, antidepressants, diuretics, etc.) or toxic effects (smoking, alcohol, drugs), as well as electrolyte disturbances (hypo- or hyperkalemia, hypomagnesemia, etc.);
- idiopathic – when the cause of the arrhythmia could not be identified.
Diagnostics
Of course, the central role in the diagnosis of arrhythmias is played by electrocardiogram analysis, single ECG recording or 24-hour (Holter) monitoring.
An ECG with stress and functional studies are performed. Sometimes a revil-implantable device is installed that continuously records the ECG for several months. Additionally, an electroencephalogram, genetic testing, MRI or CT scan of the heart, and echocardiography are performed. Laboratory methods for diagnosing arrhythmias in order to identify electrolyte disturbances and signs of inflammation deserve special attention. Blood, urine, nail or hair tests are taken to determine the levels of magnesium, potassium, sodium, and chlorine. Blood tests are more revealing.
You can perform a complex laboratory test "Cardiorisk", including determination of troponin levels, NT-pro BNP; C-reactive protein, homocysteine, triglycerides, lipoprotein, creatine kinase, LDH, cholesterol, low and high density lipoproteins, D-dimer.
To monitor the effectiveness of treatment, a study of the level of drugs amiodarone, lidocaine, procainamide in the blood is prescribed using high-performance liquid chromatography.
The mechanism of heart rhythm disturbances
The heart has the following abilities:
- automaticity - cardiomyocytes can spontaneously generate an impulse (due to this they are called “pacemakers”);
- excitability - cells perceive the signal and respond to it;
- conduction - the impulse can spread through the conduction system of the heart;
- contractility - the ability to contract in response to a stimulus.
Thus, the myocardium independently generates electrical currents that are conducted along the intracardiac pathways, excite the muscle and cause its contraction.
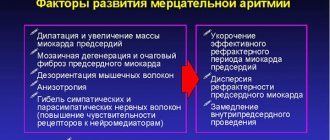
As noted earlier, arrhythmias arise due to a violation of impulse formation or conduction. The main mechanisms are presented in the figure below.
A change in automaticity in the sinus node is the cause of tachycardia, bradycardia (with weakness of the sinus node) and other arrhythmias. If the excitability of the underlying links of the conduction system, for example, the atrioventricular connection, increases, then it takes on the role of a pacemaker, and an ectopic accelerated rhythm occurs.
Trigger activity is the formation of impulses by cardiomyocytes, which normally do not have a pacemaker (signal-generating) function. This mechanism underlies extrasystoles and tachycardias as well as another, re-entry (in its case, the signal causes one contraction, but under certain conditions it can excite the myocardium repeatedly due to the circulation of current in a circle).
A blockade occurs when an impulse encounters tissue that is unable to respond to the signal, for example, a post-infarction scar that has taken the place of a damaged cardiac conduction system.
How does the human heart work?
Each person's heart has 4 chambers: 2 ventricles and 2 atria. A healthy heart contracts and relaxes rhythmically. Initially, blood flows through the veins into the atria, after which they contract and the blood is pushed through the valves into the relaxed ventricles. After this, it is the turn of the ventricles to contract. As a result, the blood from them enters the aorta and pulmonary artery, and the valves prevent it from returning back to the atria. There is a short pause, during which blood from the veins is again supplied to the atria and the cycle repeats. Thus, the contractions of the chambers take about 0.43 seconds, and the rest period is 0.4 seconds. Therefore, an adult’s heart manages to complete an average of 70 cycles per minute.
The conduction system is responsible for the timeliness of heart contractions. It is a complex of atypical muscle fibers located inside the heart: the sinus-atrial and atrioventricular nodes. It is they, under the influence of impulses generated in the muscle cells of the heart, that ensure the automaticity of the work of the main muscle of the human body.
The sinoatrial node is called the first order pacemaker or the main one. It is formed by a small cluster of cardiomyocytes (special muscle cells). They generate electrical impulses that are transmitted along nerve fibers to the left atrium, from where they pass through special anatomical structures into the ventricles. This guarantees the initial contraction of the atrium and then the ventricle, i.e. normal heart function.
Signs and symptoms: what complaints do patients have?
The palette of clinical manifestations is varied and colorful: from normal health to loss of consciousness and arrhythmogenic shock.
Depending on the type of arrhythmia, psycho-emotional status and concomitant diseases, patients present the following complaints:
- heart sinking;
- heart beats against the chest;
- cardiopalmus;
- dizziness, darkening of the eyes;
- shortness of breath, feeling of lack of air;
- weakness, fatigue;
- loss of consciousness and so on.
These symptoms are accompanied by a feeling of fear and are not always specific. A similar picture of the disease is also described by somatically (physically) healthy people suffering from panic attacks, neuroses or phobias. In these situations, we are talking about psychosomatics, and work with a psychotherapist is required, and not treatment by a cardiologist.
Case study: arrhythmia in a woman
There was an interesting case in my practice: a middle-aged woman came in complaining of episodes of loss of consciousness. They occurred during physical activity (climbing stairs, riding a bicycle), which was accompanied by severe shortness of breath, and before falling, she felt a palpitation. Before contacting a cardiologist, the patient was examined by a neurologist, but no abnormalities were identified.
When conducting echocardiography of the heart, the following was visualized: secondary hypertrophic cardiomyopathy, which developed as a result of subvalvular aortic stenosis. Thickened left ventricular myocardium is a risk factor for the development of life-threatening tachycardias and sudden cardiac death. During 24-hour ECG monitoring, runs of ventricular arrhythmia of varying duration were recorded.
The patient was sent for surgical treatment - correction of the heart defect and ablation (cauterization) of the arrhythmia area.
Features in men
A special feature of arrhythmia in men is “holiday heart syndrome.” This is a condition in which, after short-term consumption of large doses of alcohol (usually during feasts), arrhythmia occurs. More often, atrial fibrillation (atrial fibrillation) or ventricular arrhythmias occur.
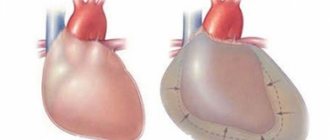
Clinically, this syndrome is manifested by a feeling of palpitations, a feeling of weakness, shortness of breath, and chest discomfort, which can lead to arrhythmogenic death. The mechanisms of alcohol’s effect on the heart include both direct toxic effects and increased activity of the sympathetic nervous system and electrolyte imbalance. In chronic alcoholism, cardiomyopathy develops, the main manifestations of which are heart failure and cardiac arrhythmias.
If you stop drinking alcohol in time, there is a chance to restore the pumping function of the heart, but scientists have not been able to find out where the limit is when it is not too late. The attitude towards drinking in our country is very frivolous; people believe that alcohol “cleanses blood vessels” and its consumption is associated with health benefits. Yes, systematically drinking people rarely have heart attacks - they die from sudden arrhythmias, before thrombosis occurs.
Classification of arrhythmias
Since the article is general education, I will not overload you with scientific terms, pathophysiology and other characteristics, but in general terms I will explain into which main groups arrhythmias are divided.
According to their source (topographically), they are supraventricular (everything that arises above the atrioventricular node) and ventricular. Based on the rhythm frequency, tachycardia (with a heart rate of more than 90-100 per minute) and bradycardia (slowing the rhythm to 50-60 beats or less) are distinguished. Tachycardias, in turn, are divided into supraventricular and ventricular, paroxysmal and non-paroxysmal.
Bradycardia is based on a violation of impulse conduction - blockade, which can be sinoatrial, atrioventricular, interatrial and intraventricular. These are the most common arrhythmias, and such a classification gives an idea of how they should be treated.
Table 1. Classification of arrhythmias.
By localization:
|
By heart rate:
|
Tachycardia:
|
Blockades:
|
I will separately highlight extrasystole - the “queen” among arrhythmias. The overwhelming number of patients come to me with exactly this problem. Extrasystoles are extraordinary contractions of the heart. They occur in everyone - both in healthy people and in people with various diseases - and often deprive patients of peace and sleep due to the painful sensations they experience during rhythm disturbances.
An interesting paradox is associated with this type of rhythm disturbance: in healthy individuals they do not pose a threat to life, despite the striking manifestations of symptoms. In people with serious organic diseases, extrasystoles can be asymptomatic and be an accidental finding on an electrocardiogram or daily ECG monitoring.
Manifestations on the cardiogram
Let's consider the signs of arrhythmia on the electrocardiogram using the example of extrasystole, tachycardia and blockade of impulse conduction.
If a patient has an extrasystole, for example an atrial one, his ECG will look like this: against the background of a regular sinus rhythm, where there are equal intervals between the ventricular complexes, an extraordinary contraction appears, followed by a pause of varying duration depending on the type of extrasystole.
We will analyze tachycardia using two examples: paroxysmal AV nodal and ventricular. With the first type of arrhythmia, an episode of rhythm with a high frequency is recorded on the ECG, while it remains constant throughout the entire paroxysm. The complexes on the cardiogram are narrow and the P waves, characteristic of sinus rhythm, will not be visible.
With ventricular tachycardia, dilated deformed complexes are recorded, reminiscent of bundle branch blocks; heart rate is more than 120 beats per minute.
In the case of blockade development, for example, 1st degree AV block, on the ECG we see an extension of the PQ interval by more than 0.2 seconds, which reflects a disturbance in the conduction of impulses from the atria to the ventricles. With 2nd degree AV block Mobitz 2 there is a sudden loss of the complex, while the PQ interval is either prolonged or normal.
Forecast
Cardiac arrhythmia itself is not classified as a fatal disease, therefore, with the appropriate level of drug treatment, compliance with medical recommendations and giving up bad habits, a patient with arrhythmia can lead a full life.
If the attack of arrhythmia is isolated and caused by emotional stress, it is enough to take a short course of rehabilitation and take a number of sedatives.
If cardiac arrhythmia is concomitant, then stopping the signs of the underlying disease will reduce the risk of arrhythmia progression to a minimum.
By taking medications for cardiac arrhythmia on an ongoing basis, the patient reduces the likelihood of a major attack to a minimum.