Bradycardia
Bradycardia is a type of cardiac arrhythmia characterized by a slowing of the heart rate to 55 beats per minute or lower. It is the norm for athletes who systematically experience significant physical activity. In this case, we talk about physiological (functional) bradycardia. However, more often it is pathological in nature and serves as a symptom of heart disease. This condition is based on the inability of the sinus node to produce electrical impulses more than 60 times per minute, or to distribute them correctly along the conduction pathways.
Causes of sinus bradycardia
Pathological causes of the development of the disease are of two types - organic and functional. The latter are provoked by the following factors:
- disruptions in the functioning of endocrine organs;
- high intracranial pressure;
- neurocirculatory dystonia;
- excessive use of drugs;
- increased potassium levels in the blood.
Organic causes of bradycardia are caused by the following diseases:
- heart defects;
- myocardial infarction;
- myocarditis;
- heart damage as a result of arthritis, vasculitis, collagenosis;
- post-infarction cardiosclerosis.
Types of bradycardia and causes of its occurrence
According to its localization, pathological bradycardia of the heart can be:
- sinus. Appears due to a malfunction of the sinus node;
- caused by heart block. In this case, the sinus-atrial or atrioventricular conduction of impulses is disrupted.
Sinus bradycardia, depending on the causes that provoked it, is divided into the following forms:
- Organic. Appears as a result of any cardiac pathology: dystrophy or myocardial infarction, cardiosclerosis, myocarditis.
- Neurogenic (not associated with heart disease). This form can be caused by many factors: increased intracranial pressure, brain tumors and brain hemorrhages, various neuroses, vegetative-vascular dystonia, head bruises, wearing an excessively tightly tied tie or tight collar. Bradycardia is typical for patients with reduced thyroid function. Its cause may be a stomach or duodenal ulcer.
- Medicinal. This form is caused by taking certain medications, in particular, cardiac glycosides, morphine, β-blockers, calcium channel blockers, etc.
- Toxic. Develops with severe intoxication due to sepsis, typhoid fever, uremia, hepatitis. Toxic bradycardia is caused by poisoning with phosphorus compounds.
Sometimes the cause of the slow heart rate cannot be determined. This form is called idiopathic.
Cardiac bradycardia in a child or adolescent is usually caused by the same causes as in an adult. Such children require systematic monitoring by a cardiologist.
Women sometimes develop sinus bradycardia during pregnancy. This is a temporary condition that is not considered a pathology and goes away on its own after childbirth.
Diagnosis of bradycardia
Only a doctor can differentiate physiological or pathological bradycardia. To do this, he uses several diagnostic methods.
Auscultation
A simple diagnostic method is to listen to the heart using a phonendoscope. Auscultation of the heart allows not only to determine a rare rhythm, but also to suspect certain diseases of the cardiovascular system.
Electrocardiography
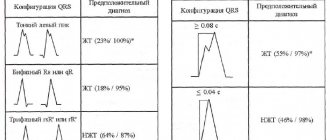
ECG is a method of instrumental diagnostics of the heart, which records not only heart rate, but also helps to diagnose cardiac causes of bradycardia (myocardial ischemia and infarction, sinus node pathology, AV block). This is important for effective therapy. In some cases, daily ECG monitoring is necessary - a Holter study.
Phonocardiography
Phonocardiography (PCG) is a method of hardware diagnostics of sound phenomena that are created during the work of the heart. The study is carried out in conjunction with an ECG. At the same time, the heart sounds that are created during the operation of the valves, as well as additional noise, are assessed.
To diagnose the causes of bradycardia, the doctor may also prescribe:
- EchoCG - ultrasound examination of the heart;
- blood test for markers of damage to the heart muscle (troponins, creatine kinase);
- study of inflammation indicators (C-reactive protein, rheumatic tests, markers of collagenosis);
- blood test for thyroid function indicators (TSH, T4, T3);
- study of blood electrolytes (potassium, magnesium, calcium, sodium);
- biochemical blood test (glucose, bilirubin, cholesterol, creatinine, etc.).
Clinical picture
Mild bradycardia (45–55 beats per minute), which does not cause significant disturbances in the body, is usually not accompanied by clinical manifestations. Symptoms such as dizziness, weakness and fainting occur when the heart rate drops to 40 beats per minute.
In addition, when the heart rate slows down, you may experience:
- chronic fatigue;
- dyspnea;
- cold sweat;
- chest pain;
- blood pressure surges;
- problems with attention, thinking and memory;
- flashing “flies” before the eyes.
In severe cases, fainting and episodes of loss of consciousness are possible. The severity of bradycardia symptoms depends on the degree of circulatory disorder developing against its background.
Prevention
Sinus bradycardia requires constant prevention. To do this, you need to visit a cardiologist once a year in order to promptly detect and treat cardiac bradycardia.
In order to reduce the risk of disease, you must follow simple rules:
- to give up smoking;
- normalization of blood pressure;
- control diabetes and maintain blood sugar levels close to normal;
- reduction of high cholesterol levels;
- maintaining normal weight;
- eating heart-healthy foods;
- maximum restriction of alcohol consumption;
- daily exercise;
- reducing the risk of stress factors.
If you are concerned about a low heart rate, you should not delay visiting your doctor. Any disturbances in the functioning of the heart can lead to serious consequences. That is why you should not postpone drug treatment for bradycardia. Make an appointment at our clinic. Highly professional doctors with extensive experience in the treatment of bradycardia will work with you. You can find out details about the location of our branches on the “Clinic Addresses” page, as well as by phone +7 (495) 223-38-83.
Diagnostics
The main symptom of the pathology in question is a rare pulse. With sinus bradycardia, heart contractions have a regular rhythm. The sonority of heart sounds remains unchanged. Some patients experience irregular breathing.
To clarify the diagnosis, the doctor prescribes additional tests:
- ECG;
- ultrasound sonography of the heart;
- bicycle ergometry with load;
- transesophageal electrophysiological study of cardiac conduction tracts.
The latter method allows you to differentiate the functional and organic forms of heart rhythm disturbances.
During pregnancy
Pathology during pregnancy can be a general condition, or manifests itself as a result of an enlarged uterus. In this case, the vagus nerve is compressed, its tone increases, which leads to a decrease in heart rate. But this is rather rare, since more often pregnant women experience rapid heartbeat.
The presence of pathology during pregnancy most often does not have a negative impact on the condition of the pregnant woman and the fetus. Special treatment and termination of pregnancy are not prescribed in this case. Dizziness with the possibility of loss of consciousness is rare. Then it is recommended to take tonics and stimulants under the supervision of a doctor.
If the pathology continues for a long time, Doppler examination is required. Negative effects may include a lack of oxygen for mother and baby. In such cases, in the early stages, drugs are prescribed that ensure the transport of oxygen; in the last months, a caesarean section is prescribed.
Treatment of bradycardia
Physiological and mild types of pathology that do not cause much discomfort to the patient do not require therapy. If the decrease in heart rate is caused by medications, then dose adjustments or drug replacement are carried out. All other forms are eliminated with medication. The basis of treatment should be to eliminate the problem that caused the slow heart rate.
Symptoms associated with cerebral hypoxia are relieved by products containing belladonna (Bellaspon, Bellataminal, Besalol, Zelenin Drops), Eleutherococcus extract, ginseng root, and caffeine.
Drugs that can increase heart rate include:
- "Atropine sulfate";
- "Izadrin";
- "Normosecretol";
- "Orciprenaline sulfate";
- "Ephedrine hydrochloride."
Injection solutions and tablets for bradycardia are selected by the doctor, taking into account the clinical picture, contraindications, the patient’s age and concomitant diseases.
In adults
Most often, adults with pathology do not notice any discomfort. The disease manifests itself during a medical (instrumental) examination. When exposed to the carotid sinus, the contraction interval reaches 5 seconds, while in a healthy person it lasts 3 seconds. The pathology most often occurs in people who play sports professionally. During long-term exercise in athletes, the vagus nerve is in increased tone. But this does not in any way affect a person’s well-being.
Complications
Moderate or mild cardiac bradycardia may not cause hemodynamic disturbances. However, a significant decrease in heart rate (up to 40 beats or less) leads to insufficient blood flow to vital organs and their oxygen starvation. As a result, serious damage to the brain, kidneys, liver, intestines, lungs and disruption of their normal functioning can occur.
The brain suffers the most from impaired contractile function of the heart muscle (myocardium) and insufficient blood supply. Its hypoxia causes convulsions or episodes of loss of consciousness lasting up to a minute. This is the most serious complication, since breathing may stop during an attack. In case of frequent loss of consciousness with a sharp drop in blood pressure, the issue of implanting a pacemaker is decided - a device that artificially generates electrical impulses with the required frequency.
In children
Heart rate in newborns up to 140 beats per minute is considered normal. By the age of one year, the frequency of contractions decreases to 100. If the baby has a lower frequency during this period, this may be a sign of sinus-type bradycardia. At an early age, pathology is of two types: relative and absolute.
Most often, the cause of the development of pathology is a hereditary factor. In addition, hypoxia during pregnancy or increased bilirubin can provoke the disease. At a high concentration of the latter, brain tissue is saturated with this substance, which negatively affects the functioning of the cardiovascular system. This condition manifests itself in babies with the development of jaundice.
In children over 1 year of age, symptoms are as follows:
- increased drowsiness;
- decreased activity;
- fatigue;
- lethargy;
- chest pain;
- deterioration of general condition.
A small child cannot describe these symptoms, so you need to pay attention to lack of appetite, decreased activity, decreased concentration, and impaired coordination of movements. If such manifestations occur, it is worth undergoing a comprehensive examination. If the pathology is not detected in time, the heart wall may become depleted, which can lead to its rupture.
Frequently asked questions about bradycardia
What medications can be taken for bradycardia?
If you begin to notice a slowing of your heartbeat, then rush to see a doctor to determine the cause. Medicines are prescribed depending on the origin and type of pathology. Do not try to stop a sudden attack of acute bradycardia on your own. Better call an ambulance.
What causes bradycardia?
There may be several reasons for a decrease in heart rate. The leading place among them is occupied by organic heart lesions. Disorders of the nervous system, diseases of the thyroid gland and stomach, and the use of certain drugs can also provoke a slowdown in heart rate. Sometimes bradycardia is accompanied by severe poisoning.
What to take if your heart rate is low?
For mild sinus bradycardia, it is enough to drink “Zelenin Drops” 2-3 times a day, 20-30 drops with water. If bradycardia is accompanied by painful symptoms and does not go away, then you cannot do without medical help.
Drugs used for bradycardia and heart block
Home Medical encyclopedia Medicines Cardiovascular medicines
ATROPINE SULPHATE (Atropinisulfas)
Synonyms: Atropine, Atropine sulfate.
An alkaloid contained in various plants of the nightshade family (Solanaceae): belladonna (Atropa Belladonna L.), henbane (Hyoscyamusniger L.), various types of datura (Daturastramonium L.), etc.
Pharmachologic effect. Atropine is a non-selective M-cholinergic receptor blocker. The effects of atropine are opposite to those observed when the parasympathetic nerves (including the vagus) are excited.
Indications for use. For bradycardia (slow pulse) that develops as a result of increased tone of the vagus nerve and an overdose of beta-blockers and calcium antagonists.
Method of administration and dose. For blockade of vagal origin (caused by increased activity of the vagus nerve), 1 ml of a 0.1% solution is administered intravenously. Atropine in a similar dose is also used for blockade caused by propranolol or verapamil.
Side effect. When using atropine, care should be taken in dosage and the possibility of increased individual sensitivity of patients should be taken into account. A slight overdose can cause dry mouth, dilated pupils, impaired accommodation (impaired visual perception), tachycardia (rapid heartbeat), difficulty urinating, atony (loss of tone) of the intestines, dizziness.
Contraindications. Atropine is contraindicated in glaucoma (increased intraocular pressure).
Release form. 0.1% solution in ampoules of 1 ml.
Storage conditions. List A. In a place protected from light.
ISADRIN (Isadrinum)
Synonyms: Isoprenaline hydrochloride, Isoproterenol, Isuprel, Novodrin, Euspiran, Aleudrin, Aludrin, Antasmin, Bronchodilatin, Izodrenal, Isonorin, Isopropylarterenol, Isorenin, Neodrenal, Neoepinephrine, Norizodrine.
Pharmachologic effect. The pharmacological and therapeutic effect of isadrin is explained by its stimulating effect on beta-adrenergic receptors. The action of isadrin extends simultaneously to 6era- and beta2-adrenergic receptors, so the effect on the bronchi, cardiovascular system and other organs equipped with beta-adrenergic receptors is not selective.
During heart blocks, the effect of isadrin is associated with an improvement in conductivity due to its effect on the sympathetic innervation of the heart, with an increase in the excitability and contractile function of the myocardium (heart muscle). A similar effect is exerted by various sympathomimetic substances, including norepinephrine, adrenaline, ephedrine; however, these drugs cause increased blood pressure, angina pain (pain in the heart), increased excitability of ectopic foci (displaced rhythm sources) and other side effects, which limits the possibility of their widespread use in atrioventricular block (impaired conduction of excitation through the conduction system of the heart). Izadrin
more convenient for this purpose, since it does not increase blood pressure and is less capable of causing ventricular fibrillation (chaotic contractions of the heart muscle).
Indications for use. Isadrin is used in the treatment of patients with atrioventricular conduction disorders, to relieve atrioventricular block and prevent attacks in Adams-Stokes-Morgagni syndrome (loss of consciousness with a sharp drop in pressure due to certain heart rhythm disturbances).
Isadrin is also used in some forms of cardiogenic shock (normovolemic /without changes in circulating blood volume/, with reduced output and high peripheral resistance).
Method of administration and dose. Administered intravenously in a 5% glucose solution at a dose of 0.5-5 mcg (0.0005-0.005 mg) per minute.
Side effect. When using isadrin (especially in cardiological practice), it should be taken into account that it causes tachycardia (rapid heartbeat), can activate ectopic foci, cause extrasystoles (heart rhythm disturbances) with the risk of ventricular fibrillation. You should also consider the possibility of nausea and tremor (shaking) of the hands. dry mouth. Caution should be exercised when prescribing to patients with angina pectoris and thyrotoxicosis (thyroid disease).
Contraindications.
Release form. 0.5% and 1% solutions in bottles of 25 and 100 ml; tablets containing 0.005 g of the drug.
Storage conditions. List B. In a dry, cool place, protected from light.
Ipratropium bromide
Synonyms: Atrovent, Atrovent nasal. Arutropid, Vagos, Itrop, Normosecretol.
Pharmachologic effect. M-anticholinergic agent. Causes a pronounced and prolonged increase in heart rate. Dilates the bronchi, reduces the secretion of glands. Unlike atropine, it does not affect the central nervous system. The maximum concentration of the drug is determined in the patient’s blood plasma 2-5 hours after administration.
Indications for use. Sinus bradycardia (rare pulse), mainly caused by the influence of the vagus nerve, bradyarrhythmias (rare irregular contractions of the heart) with sino-auricular block (impaired conduction of excitation through the conduction system of the heart), atrioventricular block of the second degree according to Wenckebach (impaired conduction of excitation through the conduction system of the heart ) and bradysystolic form of atrial fibrillation (a type of heart rhythm disorder).
Method of administration and dose. The dose of the drug is selected individually. Treatment begins with a single administration of the contents of 1 ampoule of ipratropium bromide intravenously or with taking '/2-1'/2 tablets of the drug. When taken orally (by mouth), the drug is usually prescribed 1-1'/2 tablets 2-3 times a day.
Side effect. Dry mouth, loss of appetite, constipation, impaired accommodation (impaired visual perception), increased intraocular pressure, impaired urination, decreased secretion of sweat glands, extrasystole (heart rhythm disturbances).
Contraindications. Glaucoma (increased intraocular pressure), hypertrophy (increase in volume) of the prostate gland, mechanical stenosis (narrowing) in the gastrointestinal tract, tachycardia (rapid heartbeat), megacolon (enlargement of the upper part of the large intestine), first trimester of pregnancy.
Release form. Tablets of 0.01 g in a package of 50 pieces; injection solution 1 ml in ampoules in a package of 5 pieces.
ORCIPRENALINE SULPHATE (Orciprcnalinisulfas)
Synonyms: Alupent, Astmopent, Alotek, Astor, Dosalupent, Metaproterenol sulfate, Novasmazol.
Pharmachologic effect. Its chemical structure and pharmacological properties are similar to isadrin. The drug is a mixed type beta-adrenergic receptor stimulant, acting on beta- and beta-adrenergic receptors. Facilitates atrioventricular conduction (conduction of excitation through the conduction system of the heart).
Indications for use. Atrioventricular conduction disorders.
Method of administration and dose. In case of atrioventricular block (impaired conduction of excitation through the conduction system of the heart), the drug is used with caution, injecting 0.5-1 ml of a 0.05% solution slowly intravenously, or intramuscularly, or 1-2 ml subcutaneously. If necessary, administer the drug by slow intravenous infusion. For infusion, the contents of 1-2 ampoules of 10 ml of 0.05% solution (total 5-10 mg) are diluted in 250 ml of 5% glucose solution or isotonic sodium chloride solution and administered at a rate of 10-20 drops per minute.
To prevent attacks with Adams-Stokes-Morgagni syndrome (loss of consciousness with a sharp drop in pressure due to certain heart rhythm disturbances), with absolute bradyarrhythmia (very rare and irregular heartbeats) and with intoxication (poisoning) with digitalis drugs, digitalis is prescribed orally at a dose of '/2- 1 tablet (adults) 6-10 times a day, changing the dose and frequency of doses depending on the heart rhythm.
Side effect. Orciprenaline is usually better tolerated than isadrin, but its use may cause side effects similar to those with
Neniya Izadrina. When administered intravenously, a decrease in blood pressure is possible.
Contraindications. Severe atherosclerosis.
Release form. 0.05% solution in ampoules of 1 and 10 ml (0.5 and 5 mg); tablets 0.02 g.
Storage conditions. List B. In a dry place.
EPHEDRINE HYDROCHLORIDE (Ephedrinihydrochloridum)
Synonyms: Ephedrine hydrochloride, Efalon, Ephedrozan, NeoPhedrin, Sanedrin, Efetonin, etc.
An alkaloid found in various types of ephedra (EphedraL.), fam. ephedraaceae (Ephedraceae), including Ephedraequisetina (equisetum ephedra), growing in the mountainous regions of Central Asia and Western Siberia, EphedramonospermaS.AM, growing in Transbaikalia, etc.
Pharmachologic effect. Ephedrine stimulates alpha and beta adrenergic receptors.
In terms of its peripheral sympathomimetic effect, ephedrine is close to adrenaline. Causes vasoconstriction, increased blood pressure, dilation of the bronchi, inhibition of intestinal peristalsis (wave-like movements), dilation of the pupils, increased blood glucose levels. Facilitates atrioventricular conduction (conduction of excitation through the conduction system of the heart).
Indications for use. Atrioventricular conduction disorders.
Method of administration and dose. Used in cases where the use of atropine, isadrine and orciprenaline sulfate is contraindicated, at a dose of 30-50 mg every 4-6 hours, but the effect is rarely achieved. To avoid disruption of nighttime sleep, ephedrine should not be prescribed at the end of the day or before bedtime.
Side effect. The drug is usually well tolerated. Sometimes, 15-30 minutes after ingestion, slight trembling is observed, which quickly passes.
Contraindications. The drug is contraindicated in atherosclerosis, organic heart disease, hyperthyroidism (thyroid disease).
Release form. Powder; tablets 0.025 mg; tablets 0.002; 0.003 and 0.001 g; 5% solution for injection in ampoules of 1 ml; 2% and 3% solutions in 10 ml bottles.'
Storage conditions. List B. Powder - in a well-closed container, protected from light; tablets, ampoules and solutions - in a place protected from light.
| print version | This information is not a guide to self-treatment. A doctor's consultation is required. |
Emergency care for bradycardia
You need to act quickly, especially if several symptoms are present at once, and be sure to call an ambulance.
While you are waiting for an ambulance you need to:
- lay on your back, placing a cushion under your legs so that they are slightly higher than your heart.
- If symptoms include pain in the heart area, nitroglycerin can be given. This drug acts quickly, relief will come within 5 minutes.
- You can take some medications (belladonna extract). This drug is suitable for those who are experiencing symptoms of bradycardia attacks for the first time. Two tablets of the drug need to be crushed and poured under the tongue. But the effect will not appear as quickly as from nitroglycerin, and will appear only after 30 minutes.
- those who have frequent attacks and have cardiovascular diseases,
You can take isadrin - the drug acts for 10 minutes, but to take it you need to consult a doctor.