Pulmonary hamartoma (from ancient Greek “error” and “tumor”) is a benign congenital tumor that, together with the lung tissue, contains fibrous, cartilaginous or vascular structures. The term was proposed in 1094 by E. Albrecht when describing liver dysembryoplasias.
- Epidemiology
- Etiology
- Pathological anatomy
- Classification
- Symptoms
- Instrumental diagnostics
- Treatment
- Forecast
Epidemiology
Among benign lung tumors, hamartoma is most often detected. According to medical statistics, it accounts for about 60-64% of cases of all peripheral benign pulmonary neoplasms. Rarely (in 1-12 cases out of 100) endobronchial hamartomas are recorded. The disease most often develops in people aged 25 years (30-50 years). The disease is 2-4 times more common in men compared to women.
Peripheral hamartoma is 3 times more likely to be found in the anterior segments of the lungs compared to the posterior segments. Damage to the right lung is 2 times more common than to the left. In rare cases, multiple hamartomas of one or both lungs are noted. Multiple pulmonary hamartoma in female patients is sometimes a sign of the Carney triad and Cowden syndrome (according to the article “Pulmonary hamartoma: subject of research and observation experience” by the authors Vasiliev, Samtsov, Baidala, published in 2008). Very slow growth is typical.
Forecast
The prognosis is considered favorable if the tumor is detected early and adequate therapy is received. In this case, the tumor does not increase in size, and the unpleasant symptoms are controlled with medication.
Hamartoma is a benign tumor that rarely undergoes changes at the cellular level and forms metastases. In world practice, there are about 20 cases of degeneration of a hamartoma into a malignant tumor - hamartoblastoma .
Etiology
Hamartoma is the result of a violation of fetal development in the embryonic period. It includes various elements of embryonic tissues. The hamartoma contains the same components as the organ in which it is located. These components are located incorrectly, and the degree of differentiation is also incorrect. This is the difference between a hamartoma and a teratoma. It is worth noting that the latter also consists of tissue primordia that are foreign to the organ in which it is localized (according to Vasilyev, Samtsov, Baidaly).
Content
- 1. History
- 2 Epidemiology
- 3 Etiology and pathogenesis
- 4 Pathological anatomy
- 5 Classification 5.1 Based on tissue predominance
- 5.2 By number of tumors
- 5.3 By localization
- 7.1 X-ray of the lungs
Pathological anatomy
Macroscopically, the hamartoma is most often round in shape, its surface is finely lumpy or smooth, and the consistency is dense-elastic or dense. There is no capsule. Clear demarcation from adjacent lung tissue. On the section, the tumor has a grayish or gray-yellow tint, and has a lobular appearance. The tumor includes foci of cartilage and is separated by fibrous layers; lime inclusions are often found (according to the book “Thoracic Surgery: A Guide for Doctors,” edited by L.N. Bisenkov).
In some cases, a hamartoma removed from its bed breaks up into separate lobules. The compressed alveoli form the tumor bed. There is no anatomical connection between them and the tumor, which explains the possibility of enucleating the hamartoma during surgery.
Microscopically, hyaline, and in rare cases, elastic cartilage, which has an atypical structure, is determined; there are layers of connective and adipose tissue around it. Areas of calcification or ossification are also detected. Sometimes there are lymphoid accumulations, smooth muscle fibers, and cyst-like cavities lined with epithelium.
Causes of hypothalamic hamartoma
This type of tumor is considered quite rare and difficult to diagnose and treat. Hypothalamic hamartoma manifests itself in the form of seizures, cognitive impairment and endocrinological disorders. Premature puberty is a characteristic symptom of the pathology.
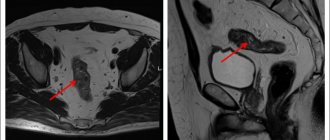
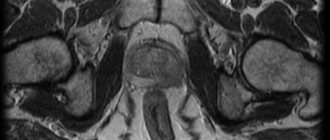
The diagnosis is made based on the results of MRI, EEG (electroencephalography), neuropsychological testing, taking into account the general symptoms and complaints of the patient.
The main causes of hypothalamic hamartoma are genetic disorders and exposure to negative factors during fetal development (infections, stress and inflammatory diseases of the mother). The diagnosis is made to one in 200 thousand children.
On our website you can make a personal appointment with a doctor and get an answer to the question “hamartoma - what is it?”
Symptoms
Lung hamartoma develops in the human body without causing specific symptoms. If a subpleural hamartoma progresses and grows, a person may complain of unusual sensations or pain in a certain area of the chest (depending on the location of the formation). If a hamartoma originates from the wall of the bronchus, its growth may impair the patency of the bronchi. In such cases, a person develops a cough with the release of mucous or mucopurulent sputum in a small amount; in rare cases, hemoptysis is also noted.
Prevention
Due to the fact that the tumor-like node begins to form during embryonic development and is partly due to genetic factors, there is no specific prevention.
It is almost impossible to predict in advance at what stage of development a failure will occur. However, parents can make their contribution to the birth of a healthy baby. To do this, it is necessary to minimize all risks associated with the negative impact of the environment on the health of the expectant mother.
Parents are advised to adhere to a healthy lifestyle, give up bad habits, and unquestioningly follow the instructions of the attending physician. Particular care should be taken when taking medications, especially during pregnancy.
Only with the right organizational approach to bearing and giving birth to a baby can the risk of developing pathology be significantly reduced, even with a genetic predisposition to neoplasms.
Instrumental diagnostics
An x-ray is required. A hamartoma is visible as a single (or multiple) spherical shadow (of solitary pulmonary nodes), having clear, slightly wavy contours. With a lobular structure, the tumor has a tuberous outline. Typical are calcareous inclusions, which are localized as individual grains or a central conglomerate.
The shadow in the center of the tumor is often more intense than the shadow of the edges, which suggests that it is a hamartoma and not another tumor. The pulmonary pattern around the formation is often unchanged. Sometimes a rim may be detected along the periphery (tumor bed). There are no changes in the root of the lung, and there are also no pleural reactions. Whatever part of the lung tissue the hamartoma is localized in, its long axis in all cases is directed towards the root of the lung. If we carry out long-term dynamic observation, it can be noted that the size of the hamartoma changes very slowly, but the intensity of calcareous deposits often progresses.
Endobronchial hamartomas manifest themselves with direct and indirect signs. Straight is a spherical tumor-like formation in the lumen of the bronchus with smooth and clear contours, detected on X-ray tomography. Indirect manifestations are hypoventilation, atelectasis and other signs that indicate impaired bronchial obstruction.
Fiberoptic bronchoscopy
Endobronchial hamartoma can be localized in the area of the bronchial “spur” or on the walls of the bronchi. The shape is cone-shaped and gar-shaped, the color is whitish, the base is wide. The mucous membrane covering the hamartoma is unchanged. Instrumental palpation reveals a rocky density, which makes it difficult to take biopsy material from the tumor.
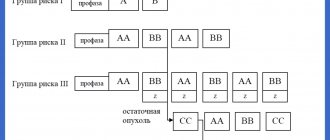
Classification
The generally accepted classification is based on the predominance of certain tissues in the neoplasm.
Types of hamartomas indicating the predominant tissue:
- lipomatous (fatty);
- chondromatous (cartilaginous);
- fibromatous (connective);
- leulomyomatous (smooth muscle);
- organoid (several types);
- angiomatous (vessels).
Depending on the number of pathological formations, single and multiple foci are distinguished.
Lung hamartoma
Congenital, benign neoplasm. The tumor can contain both lung tissue and adipose, cartilage tissue, as well as blood vessels and fibrous formations. It is considered the most common species among hamartomas.
The pathological process is formed against the background of mutation at the level of growth and differentiation of tissues during gestation in the fetus. After birth, the pathological node continues to grow and develop. The first symptoms may only appear decades later. It is easiest to diagnose a node that contains cartilage tissue. The neoplasm can also include alveolar, epithelial, connective and other types of tissue. The parenchyma is affected subpleurally (on the surface) or intrapulmonary (in the deep layers). Most often, the node is located in the lower lobe of the right lung.
The formation is considered absolutely benign; metastases are not diagnosed. Lung tissue can be damaged only when the tumor a large size. Typically, nodes do not exceed 40 mm in diameter, but in medical practice large neoplasms up to 100 mm are also encountered.
Hypothalamic hamartoma
The hypothalamus is located between the floor of the third ventricle and the diencephalon. This area of the brain is responsible for the functioning of the internal glands and other vital systems. Any structural changes in the hypothalamus lead to serious disruptions in the functioning of the entire organism.
A hypothalamic hamartoma is a benign compaction that consists entirely of organ pathogens and does not contain foreign inclusions. As the hamartoma increases in size, adjacent tissues are compressed, which can negatively affect the patient’s health.
A neoplasm in the hypothalamus also originates at the embryonic stage. The first signs of pathology may appear already in the first year of a child’s life. The cause of the development of hypothalamic hamartoma is considered to be the negative impact of external factors on the body of a pregnant woman, which leads to cell mutation in the fetus.
Hamartoma of the breast
The formation of the neoplasm also begins during the development of the embryo. Breast hamartoma is considered a benign tumor, but it can bring some discomfort to a woman’s life. A cystic neoplasm consists entirely of tissue from the own mammary gland. The first symptoms appear after 30 years. The pathological node is easily palpable, has clear boundaries and moves freely (if its size is more than 30 mm). May cause pain when palpated. Ultrasound examination reveals it as a dense, lumpy formation.
Liver hamartoma
The formation of a benign tumor occurs during the formation of the embryo. At the initial stage, the disease is completely asymptomatic. In 7% of patients, malignancy occurs and the tumor turns cancerous. The disease is detected in childhood. The tumor looks like a dense, lumpy formation. Depending on the structural composition, two varieties are distinguished:
- mesenchymal;
- hepatocellular.
Classification of liver hamartoma by location in the organ:
- near-surface;
- deep;
- subcapsular.
It is also customary to distinguish cystic and fibrous hamartomas, true and biliary tumors.
The danger of the disease lies in the risk of rupture of the neoplasm and the very rapid proliferation of pathological cells. Compression of neighboring organs and tissues is possible. It is important to pay attention to signs such as:
- attacks of nausea;
- excessive thinness;
- fast fatiguability;
- stool instability (alternation of constipation , diarrhea and vice versa);
- muscle weakness.
Hamartoma of other organs
The neoplasm can be located in other human organs and tissues:
- spleen;
- retina and iris (astrocytic form);
- nose (nasal form);
- esophagus, stomach, large intestine (presacral form);
- sebaceous glands;
- The lymph nodes;
- skin of the thighs, buttocks, arms, legs, face (cutaneous hamartoma);
- renal system ( angiomyolipoma ).
Treatment
Since the diagnosis can finally be made only after a histological examination of the removed hamartoma, the main method of therapy is surgical, that is, surgery. Subpleurally located hamartomas are removed by simple enucleation with a previous incision of the pleura above them and the cortical layer of the lung. In recent years, this operation has been performed using video-thoracoscopic techniques, avoiding traumatic incisions.
When the hamartoma is located endobrochially, in some cases they resort to excision of the tumor during fiberoptic bronchoscopy. If there are significant contraindications to the operation, the doctor can only prescribe long-term follow-up.
Story
German physician Hermann Lebert (1813-1878), who first described a cartilaginous tumor of the lung in 1845.
A cartilaginous tumor of the lung was first described in medical literature in 1845 by the German physician Hermann Lebert (1813-1878). The histological structure and macroscopic picture were later studied by Rudolf Ludwig Karl Virchow, 1863, Hans Chiari, 1883, Felix Victor Birch-Hirschfeld, 1887, Maurice Letulle, 1897. , A.I. Abrikosov (1903), Hart (1906), however, reports of intravital detection of cartilaginous lung tumors appeared only in the 20th century, which is associated with the advent and development of radiology. Already by 1926, according to Hickey and Simpson, there were 40 cases of detection of cartilaginous lung tumors in the world literature. Subsequently, due to the successful development of thoracic surgery, reports of the detection of pulmonary hamartomas increased significantly.
German pathologist Eugen Albrecht (1872-1908), who first proposed the term “hamartoma” in 1904
For a long time, there was no consensus in scientific medical circles about the causes of cartilaginous lung tumors. Hans Chiari, who discovered this formation against the background of bronchiectasis, believed that cartilaginous tumors arise against the background of chronic inflammation. Similar views were held by Rudolf Virchow, Johannes Orth and some other pathologists. Will suggested that pulmonary chondromas arise from the so-called “bronchiogenic tissue” - embryonic gill arches. All of the above scientists agreed that hamartomas are true tumors. However, back in the late 19th and early 20th centuries, Felix Victor Birch-Hirschfeld, Maurice Letul and A.I. Abrikosov believed that cartilaginous tumors arise in the embryonic period from elements of the bronchial tree (according to A.I. Abrikosov, this point of view was confirmed presence of adenomatous structures in these formations).
The term “hamartoma” was first proposed by the German pathologist Eugen Albrecht (1872-1908) in 1904 when describing liver dysembryoplasia. In 1922, Feller first used this term to refer to lung tumors, since he believed that all benign lung tumors described by that time could be classified as hamartomas. In 1930, Bayer used this term to refer to cartilaginous lung tumors containing other tissue elements. Goldsworthy in 1934 used the term "hamartoma" to refer to benign lung tumors consisting primarily of a combination of fat and cartilage tissue.
Despite the fact that hamartoma is not an organ-specific pathological condition, currently in the world medical literature the term “hamartoma” is usually used in relation to lung formations.
Pathology prognosis
The tumor rarely recurs; only 7% of cases of recurrent development of compaction after surgery have been recorded. Immediately after removal of the seal, regular examination by a pulmonologist is recommended for 2-5 years. Hamartoma is sometimes hidden, when even after diagnostic studies it is not immediately visible.
Painful symptoms disappear immediately after recovery in the postoperative period. The role played by doctors preserving most of the respiratory organs. When only the tumor is removed from the lung tissue, the patient recovers quickly. But if a lobe resection was performed, the standard of living deteriorates.
It is important to find out in time what pulmonary hamartoma is and undergo examinations and listen to the body. This way you can avoid complications.
Author: Evgeniya Leshenkova Therapist, pulmonologist
Likely consequences
Despite its benign nature, the lack of timely removal is dangerous due to malignant transformation, the development of obstructive pneumonia, segmental or lobar atelectasis. In rare cases, the hamartoma rapidly increases in size, causing metastases to occur in the liver, spine and diaphragm.
If the pathology is started, the hamartochondroma degenerates into chondrosarcoma, liposarcoma, adenocarcinoma or fibrosarcoma. These malignant tumors are deadly for the patient.