Forms of sore throat and symptoms of the disease in adults
Each form of sore throat manifests itself differently. It is important to find out which pathogenic microorganism caused the disease. But it is impossible to determine this at home. Only a qualified doctor can accurately identify the nature of the pathogen and prescribe adequate treatment for sore throat, promoting a speedy and complete recovery.
Catarrhal sore throat
Acquired through contact with an infected person, it begins acutely, with a slight increase in body temperature and a feeling of weakness. The tonsils and submandibular lymph nodes are slightly enlarged. Dryness in the mouth and throat is accompanied by a sore sensation; swallowing is painful and difficult. If not stopped in time, the disease can develop into a severe form with subsequent complications.
Lacunar tonsillitis
The purulent form of tonsillitis is characterized by a very rapid onset of symptoms. The lymph nodes become enlarged and swollen, the tonsils are markedly swollen and covered with a white-yellow purulent coating. The throat with lacunar sore throat hurts especially badly.
An increase in temperature to 40 degrees is accompanied by headache, muscle and joint pain, sometimes radiating to the heart. Fever may cause seizures, vomiting, and confusion.
In the absence of proper treatment, lacunar tonsillitis can develop into fibrinous tonsillitis, when severe purulent intoxication of the body begins, in some cases causing brain damage.
Follicular tonsillitis
The purulent form has symptoms similar to lacunar angina. The tonsils are covered with many purulent follicles. Sometimes the patient complains of pain in the lower back, joints ache, like with the flu. Unbearable pain in the throat radiates to the ear.
This form of purulent tonsillitis is dangerous due to a wide range of complications, as well as rupture of the follicles inward, followed by a purulent abscess.
Herpangina
A dangerous viral form acquired by using a shared toilet, shaking hands and any type of tactile contact with a carrier of the disease - a person or animal. Small serous blisters appear on the tonsils, throat and palate. The throat hurts unbearably, the cervical lymph nodes are swollen and painful to the touch.
At the same time, all the symptoms characteristic of influenza appear: fever, chills, headache, nausea, diarrhea.
Confirming the diagnosis of “herpetic sore throat” is only possible by consulting a doctor. A qualified specialist will first of all direct the patient to undergo tests for serological testing and virology, after which he will prescribe a course of necessary antibiotics.
Otherwise, improper treatment can have serious consequences: encephalitis, meningitis, and myocarditis.
Phlegmonous sore throat in adults
This is a purulent form of the disease, typical for the age group of 20-40 years. The causative agent is streptococci, and the cause is not long-standing catarrhal or follicular tonsillitis. With this form of sore throat, redness is observed not only of the palate and tonsils, but also of the peri-almond space.
The throat hurts on one side, the focus of suppuration does not have clear boundaries and requires surgical intervention.
The patient has chills and fever, the voice is hoarse or disappears completely. As a result of purulent melting of the tonsil, a characteristic, unpleasant odor comes from the mouth.
Treatment of phlegmonous sore throat cannot be delayed. In the absence of timely assistance from specialists, in most cases, cervical or brain abscesses, purulent meningitis, and general blood poisoning occur.
Treatment of angina should occur under the strict supervision of a doctor, who will be able to notice in time and prevent the development of complications that are of the most unexpected nature.
Etiology and pathogenesis
Among the various possible microbial pathogens of sore throat (cocci, bacilli, viruses, spirochetes, fungi, etc.), in most cases the main etiological role belongs to group A b-hemolytic streptococcus (GABHS). This pathogen, according to a number of authors, is detected in sore throat in more than 80%, according to other sources - in 50–70% of cases. Much less frequently, acute tonsillitis is caused by group C and G streptococci, Arcanobacterium haemolyticum, Neisseria gonorrhoeae, Corynebacterium diphtheria (diphtheria), anaerobes and spirochetes (Simanovsky-Plaut-Vincent angina), and extremely rarely by mycoplasma and chlamydia. The cause of acute viral tonsillitis can be adenovirus, rhinovirus, coronavirus, influenza and parainfluenza viruses, Epstein-Barr virus, Coxsackie A virus and others. Penetration of an exogenous pathogen into the mucous membrane of the tonsils can occur through airborne droplets and alimentary routes, as well as through direct contact. In the occurrence of an endogenous pathogen, great importance is attached to chronic tonsillitis. As noted by B.S. Preob¬ra¬zhensky (1954), the frequency of sore throats in chronic tonsillitis is explained by the fact that in this disease there are usually up to 75% of cases of carriage of GABHS, vegetating in the crypts of the palatine tonsils.
In the pathogenesis of tonsillitis, a certain role can be played by a decrease in the body’s overall reactivity to cold, sharp seasonal fluctuations in environmental conditions (temperature, humidity, nutrition, intake of vitamins, etc.), trauma to the tonsils, constitutional predisposition to tonsillitis (for example, in children with lymphatic – hyperplastic constitution), the state of the central and autonomic nervous system. Factors predisposing to angina are chronic inflammatory processes in the mouth, nose and paranasal sinuses. The development of sore throat occurs according to the type of allergic-hyperergic reaction, which is a prerequisite for complications such as rheumatism, acute diffuse nephritis and other diseases of an infectious-allergic nature and associated with the GABHS antigen.
Complications after a sore throat: where to expect a blow?
First of all, the ENT organs closest to the source of inflammation come under attack, especially vulnerable after suffering from a sore throat. Therefore, the recovery period, which takes place under the supervision of a specialist, will eliminate the development of a number of dangerous diseases:
- lymphadenitis (inflammation of the lymph nodes) can accompany any form of sore throat. In case of suppuration of the lymph nodes, immediate surgical intervention is required;
- Laryngeal edema is a consequence of excessive swelling of the tonsils and can spread further to the vocal cords. Rapidly developing suffocation poses a serious threat to the patient's life;
- Mediastinitis can occur as a result of suppuration of the posterior pharyngeal wall. The inflammatory process affects the deep cervical regions, right up to the mediastinum.
Chronic tonsillitis occurs after severe or frequent recurrences of tonsillitis. Overgrowth of tonsil tissue is treated with medication, although in some cases surgery is required;
Therefore, it is so important to entrust the treatment of sore throat to a qualified doctor who will determine the form of the disease and prescribe antibiotics that are mandatory in the treatment of sore throat.
The course of therapy should be carried out under the supervision of a specialist who can quickly and correctly respond to any changes in the body and prevent the development of irreversible consequences.
During pregnancy, sore throat is especially dangerous. Intoxication of the mother’s body can harm the baby, and in the early stages (up to 12 weeks) there is often a threat of miscarriage.
Treatment of sore throats
Treatment of vulgar tonsillitis.
The rational treatment of sore throats is based on adherence to a certain gentle regimen, local and general therapy. Bed rest is mandatory in the first days of the disease, and then at home without physical activity. Prescribe a non-irritating, soft, nutritious diet, mainly vegetable and dairy, vitamins, and drinking plenty of fluids is beneficial.
Patients with angina, regardless of the severity of the condition and the period of the disease (even after the fever subsides), require antibacterial treatment to prevent the subsequent development of the described metatonsillar diseases.
GABHS are highly sensitive to penicillins and cephalosporins. β-lactams remain the only class of antibiotics to which GABHS has not developed resistance. The main problem is resistance to macrolides, which in Russia is 13–17%. At the same time, the M-resistance phenotype, characterized by resistance to macrolides and sensitivity to lincosamides (lincomycin and clindamycin), has become widespread. Resistance to tetracyclines and sulfonamides of GABHS in Russia exceeds 60%. In addition, tetracyclines, sulfonamides, co-trimoxazole do not provide eradication of the pathogen, and therefore they should not be used for the treatment of acute streptococcal tonsillitis caused even by strains sensitive to them in vitro.
Given the high sensitivity of GABHS to b-lactams, the first-line (drug of choice) for the treatment of acute streptococcal tonsillitis is penicillin (phenoxymethylpenicillin). More reliable, due to the possible resistance of the pathogen, is the use of amoxicillin clavulanate and sulbactam. Oral cephalosporins are rarely used. In patients allergic to b-lactams, macrolides or lincosamides should be used. Recommended medications, doses and dosage regimens are presented below.
Antibacterial therapy for acute streptococcal tonsillitis
Penicillins
- amoxicillin 750 mg in 3 doses 10
- amoxicillin/clavulanate 625 mg in 3 divided doses 10
- amoxicillin/sulbactam
Cephalosporins
- Cefadroxil 30 mg/kg in 1 dose 10
Macrolides (prescribed
for β-lactam intolerance)
- azithromycin 12 mg/kg in 1 dose 5
- Clarithromycin 15 mg/kg in 2 divided doses 10
- midecamycin 50 mg/kg in 2 divided doses 10
- roxithromycin 5 mg/kg in 2 divided doses 10
- spiramycin 3 million units in 2 doses 10
Lincosamides (prescribed
with intolerance to β-lactams and macrolides)
- lincomycin 30 mg/kg in 3 doses 10
- clindamycin 20 mg/kg in 3 divided doses 10
In severe cases of the disease, the patient is treated in an infectious diseases hospital. Here it is rational to use parenteral administration of an antibiotic. To prevent candidiasis on an individual basis, it is necessary to prescribe antifungal drugs. It is also advisable to prescribe a hyposensitizing drug (diphenhydramine, chloropyramine, mebhydrolin, loratadine, etc.).
In addition to general therapy, rinsing (slightly warm) with a solution of furacillin, miramistin, calendula tincture, and chamomile decoction is prescribed locally; apply a warm compress to the submandibular area. During febrile periods, drinking plenty of fluids is recommended.
Antipyretics (paracetamol-containing: paracetamol, ketaprofen, ibuprofen, etc.) are indicated at a body temperature of 38°C and above.
In the acute period of the disease and in the first days of normal body temperature, bed rest is necessary, then semi-bed rest and home rest (until the 7th day of normal body temperature). At this time, taking multivitamins is indicated.
Health indicators after a sore throat are normal body temperature for 5 days, absence of sore throat and pain on palpation of the maxillary lymph nodes, normal blood tests, urine tests and electrocardiogram.
- Atypical tonsillitis should first of all include Simanovsky-Versan tonsillitis (ulcerative-necrotic), as well as tonsillitis that occurs with systemic blood diseases and leukemia, herpetic and fungal tonsillitis.
- Treatment of ulcerative-necrotic sore throat of Simanovsky-Vincent (symbiosis of the spindle-shaped rod (B. fusiformis) and spirochete (Spirochaeta buccalis) of the oral cavity) is carried out by an otolaryngologist and consists of lubricating the ulcerated mucous membrane of the pharynx with a 10% solution of novarsenol in glycerin , 2% solution of methylene blue, 1% solution of boric acid, 10% solution of copper sulfate. Gargling with a 0.1% solution of ethacridine lactate, 0.1% solution of potassium permanganate. In severe cases of the disease, amoxicillin clavulanate (625 mg x 3 times) and intravenous infusion of novarsenol (0.3–0.4 g at intervals of 1–2 days) are recommended.
- Treatment of patients suffering from secondary acute tonsillitis due to infectious diseases is carried out in an infectious diseases hospital. Etiotropic and pathogenetic therapy is used. Disinfecting rinses are used locally.
- Treatment of patients with secondary acute tonsillitis due to diseases of the blood system is carried out in a therapeutic or specialized hematology department according to the rules for the treatment of the underlying disease.
- Fungal tonsillitis (pharyngomycosis) occurs mainly in young children and is caused by yeast-like fungi of the genus Candida albicans in 95% and Leptotryx buccalis in 5%.
Treatment of mycotic tonsillitis should be comprehensive. It includes oral use of antifungal antibiotics for 10–14 days (levorin, nystatin, decalinium chloride, mycoheptin, amphoglucamine B, ketoconazole, fluconazole), ascorbic acid, antihistamines and B vitamins. Rinses and inhalations are prescribed locally. For inhalation use amphotericin B, sodium salt of levorin, fluconazole, for rinsing - an aqueous solution of 3% boric acid, gramicidin 1:10000, potassium permanganate 1:10000, 1% quinosol.
Diagnostics
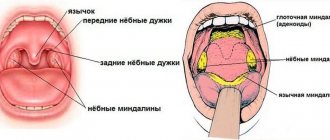
To make a diagnosis, an examination by a doctor - a therapist, pediatrician or otorhinolaryngologist - is sufficient. Pharyngoscopy (examination of the oropharynx with a spatula) reveals a significant enlargement of the palatine tonsils, the presence of exudate - white, gray or yellow purulent discharge, swelling of the palatine arches and uvula, and sometimes a bruise-like rash on the soft palate. In order to understand how to treat follicular tonsillitis , and to understand the follow-up plan after the illness, additional examinations may be required:
- general blood test with calculation of leukemia and determination of erythrocyte sedimentation rate (ESR),
- rapid test to detect group A streptococcus,
- examination of a smear from the back wall of the pharynx to determine the pathogen with a negative strep test.
As a rule, it is possible to differentiate viral and bacterial origin already at the examination stage:
- With a viral etiology, tonsillitis is accompanied by a runny nose, hoarseness or conjunctivitis.
- GABHS infection is characterized by petechiae of the soft palate, enlargement and tenderness of the lymph nodes in the neck.
- Epstein-Barr viral infection is characterized by generalized lymphadenopathy (affecting all groups of lymph nodes), an increase in the size of the liver and spleen.
- Enteroviral stomatitis has a summer seasonality and is accompanied by a rash on the palms and soles, which is why it is called “hand-foot-mouth disease.”
- Diphtheria is characterized by abundant dense deposits that are difficult to separate from the bleeding surface.
Recurrent episodes of tonsillitis must be differentiated from Marshall syndrome - recurrent attacks of febrile fever, aphthous stomatitis, pharyngitis and cervical lymphadenitis. Exacerbations occur every 2-8 weeks. The deterioration in health lasts 1-2 days and is relieved by the administration of glucocorticosteroids at the beginning of the episode. More common in children. It stops completely within a few years.
Avoid complications
There are often cases when a patient is careless about his health and decides that “it will go away on its own” or, conversely, tries to try all the advice of traditional medicine on himself. This is the other extreme of negligent attitude towards one’s health. Catarrhal tonsillitis, although it is one of the mildest forms of acute tonsillitis, but in the absence of proper treatment, severe complications can develop, which will be quite difficult to treat.
If tonsillitis is not treated, you may encounter diseases such as chronic tonsillitis (a chronic form of inflammation), rheumatoid arthritis, peritonsillar abscess, myocarditis, kidney disease (glomerulonephritis), laryngeal edema, and even sepsis.
Pregnant women need to pay special attention to their health: the inflammatory process that spreads beyond the palatine tonsils can lead to tonsil intoxication and the threat of miscarriage! Therefore, treatment of catarrhal tonsillitis in adults should be carried out on time and always under the supervision of an ENT doctor.
General information about the disease
With this type of sore throat, inflammation of the follicles of the palatine tonsils occurs. A follicle is a collection of lymphatic cells that look like small tubercles. It is in them that the protective cells of the immune system - leukocytes - are produced.
The main function of the palatine tonsils is to protect the body of any person, both adults and children, from infection entering the lower respiratory tract. The tonsils are an organ of the immune system. As soon as contact occurs between pathogenic microorganisms and the surface of the tonsil, the follicles begin to intensively produce leukocytes, which are sent to fight the enemy agent. As soon as the enemy is defeated, the dead bacteria, along with the dead leukocytes, are eliminated from the body. But if, for a number of reasons, the immune system is weakened, the tonsils cease to fully perform their functions. The inflammatory process spreads to the palatine tonsils.
If inflammation affects the lacunae of the tonsils, we talk about lacunar angina, if the follicles of the tonsils - about follicular angina, respectively.
Diagnosis of lacunar tonsillitis in children
Diagnosis of lacunar tonsillitis in children is carried out by an ENT doctor.
In 99% of cases, the otolaryngologist identifies the disease at the initial appointment. The specialist collects an anamnesis of the disease, assesses the general condition of the patient, and analyzes the complaints of the child and parents. A slight drop in body temperature after taking antipyretics for 3-4 hours is typical. After this, the fever returns to its previous levels. However, the key element in diagnosing lacunar tonsillitis is pharyngoscopy. An ENT doctor, using a special mirror and a light source, visually assesses the condition of the palatine tonsils and the entire oropharyngeal cavity. If characteristic white deposits are detected, the diagnosis of lacunar tonsillitis is beyond doubt.
For a comprehensive assessment of the condition of a sick child, the following diagnostic procedures are prescribed:
- General and biochemical blood test. These tests are used to assess the severity of infectious inflammation.
- Sowing a swab or smear from the tonsils onto a nutrient medium. The procedure allows you to accurately determine the type of causative agent of the disease and select adequate treatment.
- Polymerase chain reaction (PCR) is an optional method that allows you to accurately identify the DNA or RNA of a particular pathogen, even with its minimal amount in the body.
If the child’s condition is serious and there is a suspicion of concomitant pathology, the patient is examined by related specialists (pediatrician, cardiologist, ophthalmologist).
Prevention of sore throat
In addition to general restorative therapy and measures aimed at preventing infection, preparations of bacterial origin, in particular complexes of antigens - lysates, the most common causative agents of inflammatory diseases of the upper respiratory tract, oral cavity and pharynx, have proven to be an effective means of preventing exacerbations in various forms of pharyngitis and recurrent tonsillitis. It is possible to use similar drugs with systemic action, but this group of drugs has a greater number of contraindications.
It should be noted that all patients suffering from chronic tonsillitis who have had more than 2 sore throats over the past 3 years are subject to mandatory follow-up in group D3, that is, 2 times a year.