SPECIALISTS Gynecologist Gynecologist-endocrinologist Pediatric gynecologist Mammologist-oncologist Dermatologist Hirudotherapist Intimate plastic surgery Doctor Contour plastic doctor Ultrasound doctor SERVICES AND PRICES Gynecology Mammology Ultrasound diagnostics Paid tests Intimate surgery Contour plastic Treatment for women PROMOTIONS AND DISCOUNTS Students Teams Friends and subscribers am For residents of the region For pensioners Promotions in clinic
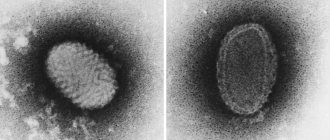
HPV is a viral infection that is transmitted between people through skin-to-skin or mucous-to-mucous contact. There are more than 100 varieties of this virus, 40 of which are sexually transmitted and can affect the genitals, anus, mouth or throat in women.
Some types of HPV, so-called. “high risk” are responsible for cancer of the cervix, anal canal, vagina and vulva. Other types of papillomavirus cause genital warts. About half of the new infections are people aged 16 to 25 years. In most people infected with HPV, the body clears it of it on its own. But for others who are not cleared of the virus, it can cause cancer of the cervix, vagina and external genitalia in women, and cancer of the anus and rectum in men and women.
And at present, medicine and, in particular, gynecology, has no way to predict who will or will not be cleared of papilloma viruses. After all, HPV usually has no visible signs or symptoms, so HPV carriers can transmit it to other people without knowing it.
What is HPV
Human papillomaviruses, entering the body through microtraumas of the skin, penetrate into the cells of the basal layer of the epithelium. HPV can exist in any layers of the epidermis. However, its reproduction occurs exclusively in the basal layer.
The development of the virus occurs in 2 stages:
- Reproductive – the virus enters a cell without affecting its chromosomes and multiplies.
- Integrative – HPV is introduced into the genome of the infected cell.
It is during the second stage that the virus transforms cells. They begin to actively divide, and tumor-like formations appear - papillomas. These are papillary growths protruding above the surface of the skin (that’s why they are called: papilloma - from the Latin papilla - nipple and Greek oma - tumor). The second stage does not always occur. The virus, being in the first stage of development, is able to regress (leave the body). However, even if the patient does not experience pathological changes, he is a carrier of HPV and is capable of infecting other people.
The incubation period can last from 3 weeks to a year. On average it is 3 months. In some cases, non-genital forms of papillomas appear first, and then neoplasms appear on the genitals.
In most cases, the body copes with the virus within 2 years. However, re-infection may occur - with the same or a different strain. Also, papillomas or other skin manifestations can regress after 6-8 months (gradually decrease and subsequently disappear). This happens when the immune system suppresses the virus and “survives” it from the cells.
Most often, the HPV virus affects the skin and mucous membranes:
- Anogenital area.
- Upper respiratory tract.
- Oral cavity.
- Bronkhov.
- Conjunctivae.
- Rectum.
- Esophagus.
Classification of viral strains
All HPV strains are divided into cutaneous and mucosotropic. Skin viruses lead to the formation of benign tumors on the skin. Mucosotropic provoke the appearance of neoplasms on the mucous membranes.
Skin strains provoke the development of different types of papillomas:
- Flat. Round nodules with a diameter of up to 10 mm. They do not turn into cancer.
- Pointed. Shaped like a cockscomb. These are pink formations covered with horny cells.
- Thread-like. Round papillomas on a thin stalk. Diameter up to 7 mm.
Mucosotropic strains cause the following diseases:
- Bowenoid papulosis. The appearance of spots and plaques on the genitals.
- Dysplasia. Pathological degeneration of cervical tissue.
- Inguinal condylomas. Ball-shaped tumors on a stalk.
If benign tumors appear, you should consult a doctor. A dermatovenerologist will determine the type of papillomavirus and the degree of its danger, and prescribe a treatment regimen for the infection.
HPV types
The first human papilloma virus (HPV) was isolated in 1971. And scientist Harald zur Hausen managed to identify and prove the connection between HPV and cervical cancer. He subsequently received the Nobel Prize for his discoveries.
Today, about 600 different strains of HPV are known. Some provoke the appearance of warts, others – condylomas, and others – papillomas. There are also types of HPV that affect the development of cancer. They are called oncogenic. Fortunately, there are not many of them. They may have low, medium or high oncogenic potential:
- Strains 6, 11, 40, 42, 43, 44, 54, 61, 70, 72, 81 are characterized by low oncogenicity.
- Average oncogenicity in types 26, 31, 33, 35, 51, 52, 53, 58, 66.
- High oncogenic potential in strains 16, 18, 39, 45, 56, 59, 68, 73, 82.
Cervical cancer is most often caused by types 16 and 18.
Reference! The presence of an oncogenic type of HPV in the body does not mean that a person is “sentenced” to cancer. The presence of the virus increases the risk of developing cancer, but is not the only cause of their occurrence. If a patient has been diagnosed with an oncogenic strain of HPV, he simply needs to more closely monitor his health and regularly undergo preventive tests. If necessary, the doctor will prescribe appropriate therapy.
About 40 types of papillomaviruses can infect the reproductive system of women and men. The result of their activity is not only cancer, but also genital warts or condylomas.
Reference! Cancer tumors develop slowly: within 5-30 years after infection with papillomavirus. They are preceded by precancerous conditions (benign neoplasms that can degenerate into malignant ones). This is why it is so important to undergo regular preventive examinations. Both precancerous conditions and even cancer in the initial stages are perfectly treatable, and dangerous consequences can be avoided.
Removal of papillomas and warts
Benign formations caused by HPV must be removed, which can be done using the following methods:
- cryodestruction - exposure to cold on a tumor;
- electrocoagulation - treatment with high frequency current;
- laser removal - layer-by-layer exposure to laser irradiation until a scab appears;
- chemical destruction - treatment with special chemical solutions that are applied to condylomas and destroy them;
- surgical removal - given the high risk of relapse after this type of destruction, it is prescribed selectively - if it is impossible to use other methods.
To prevent relapses and complications after all types of destruction, complex treatment is prescribed. Treatment with antiseptics is necessary to prevent infection of the healing surgical site. Glycyrrhizic acid (Epigen Intim Spray) is prescribed to suppress the activity of the virus, improve immune defense and stimulate regenerative processes. If the patient has a weakened immune system, he is referred to a consultation with an immunologist.
Among the new developments in the treatment of HPV is the CRISPR/Cas9 system, which almost completely cuts DNA and inserts its own sections, thereby inactivating the further spread of the virus.
Routes of transmission of HPV
The main “condition” for infection is the presence of microdamages (wounds, cracks, scratches) of the skin or mucous membranes. They serve as the “gateway” for HPV.
Most often, transmission of the virus occurs when the skin or mucous membranes of two people come into contact. Therefore, the main route of papillomaviruses is sexual contact. Moreover, the use of condoms does not exclude the possibility of infection. The virus can be transmitted through oral sex, during which contraception is not always used. In addition, the condom does not cover the entire surface of the penis, and is often put on already in the middle of sexual intercourse. HPV can also be transmitted through kissing.
HPV can also be transmitted:
- From mother to child as the baby passes through the birth canal.
- In everyday life: when using other people's hygiene products (towels, toothbrushes, shaving accessories).
- In public places: baths, gyms, swimming pools.
Reference! The survival period of papillomaviruses in the external environment is short. Therefore, although the risk of domestic infection exists, it is much lower than through sexual contact.
Self-infection is also possible: transfer of the virus from one part of the body to another during depilation, scratching the skin, biting nails.
Infection through contact with the virus does not occur in all cases. The following factors increase the risk:
- Decreased immunity.
- Bad habits: smoking, alcohol abuse.
- Stress.
- Presence of sexually transmitted infections.
- Diseases of the urinary system.
- Injuries to the skin and mucous membranes.
- Immunodeficiency states.
- Long-term use of hormonal contraceptives.
Reference! For women, oncogenic strains of HPV are more dangerous than for men, since they become infected with them more often.
Signs
If HPV does not manifest itself in formations (warts, papillomas and condylomas), then without special tests the patient usually does not know that he is infected. In this case, the symptoms of the human papillomavirus are precisely the neoplasms - they can be accompanied by itching and discomfort.
If formations appear in the genital area, they can also manifest as painful and unpleasant sensations during or after sexual intercourse.
Are you experiencing symptoms of human papillomavirus?
Only a doctor can accurately diagnose the disease. Don't delay your consultation - call
What diseases can HPV cause?
Papillomaviruses primarily provoke the growth of papillomas, warts and condylomas in patients of both sexes. All of the above neoplasms can occur on any part of the body. However, most often they affect the genitals and anal area. In women, they occur in the vulva, cervix, and vagina. In men - the scrotum, head of the penis, foreskin. In patients of both sexes, neoplasms often appear in the anus.
Warts also often appear on the soles, larynx, and vocal cords. Papillomas (papillary, flesh-colored formations) do not have a “favorite place” - they can appear on the torso, neck, face, arms and legs. In children and adolescents, flat warts (also called juvenile warts) are most common. These are small (3-5 mm) dark neoplasms that protrude slightly above the surface of the skin. Most often they occur on the back of the hands, face, and legs.
As for oncological diseases, most patients are associated with HPV, first of all, cervical cancer. Indeed, this pathology is very common in our time. However, in women, HPV also often provokes the development of cancer of the vagina and vulva (65-70% of cases), and in men – cancer of the penis (50% of cases). Also, in both women and men, papillomaviruses can contribute to the occurrence of malignant tumors:
- rectum;
- oral cavity;
- larynx.
In children, HPV usually manifests itself as the growth of papillomas against the background of decreased immunity due to previous diseases, usually viral or bacterial infections. Papillomaviruses also affect young patients suffering from allergic reactions or frequent colds.
HPV and pregnancy
Papillomaviruses negatively affect female fertility. If they are present, the likelihood of pregnancy is halved, since HPV can prevent the implantation of a fertilized egg. If the partner is also infected with the virus (which happens in 65-70% of cases), then the possibility of conception decreases even more. HPV has a negative effect on sperm motility.
When pregnancy occurs, papillomavirus increases the risk of developing:
- Little or polyhydramnios.
- Chronic placental insufficiency.
- HPV can also cause miscarriage.
Therefore, pregnant women are prescribed gentle drug therapy, which can significantly reduce all of the above risks.
When a baby passes through the birth canal, there is a risk of infection. Therefore, it is preferable for women with HPV to give birth by caesarean section - the risk of transmitting the virus is reduced by 5 times.
Changes in hormonal levels provoke the rapid growth of genital warts on the genitals. They can grow together, which can cause difficulties in urination and defecation, cause discomfort when walking, and bleeding. During childbirth, neoplasms are easily injured. They can also make it difficult for the baby to pass through the birth canal. To avoid all this, genital warts are treated in early pregnancy. Methods such as cryodestruction, laser surgery, etc. are used.
Human papillomavirus in women: causes
Having become infected with the virus, the body of a healthy woman either quickly gets rid of the pathogen, or the woman becomes an asymptomatic carrier. Among the factors that lead to the virus remaining in the body and causing HPV-associated diseases, the following should be highlighted:
- concomitant pathology of the reproductive system;
- endocrine disorders;
- immunodeficiencies and vitamin deficiencies;
- frequent acute infectious diseases - ARVI, other viral and bacterial infections;
- early sexual intercourse;
- abortions;
- smoking and drinking alcohol;
- chronic psycho-emotional stress, weakening the immune system;
- excessive physical and emotional stress, irregular daily routine;
- postpartum period - due to stress and hormonal changes;
- long-term use of immunosuppressive drugs and oral contraceptives.
Frequently changing sexual partners also increases the risk of both infection with new strains of the virus and intensification of an existing infection. If immunity decreases, the virus is integrated into the cellular genome, which entails a high probability of cancer - how to cure HPV in women at this stage has yet to be discovered by medical science. Therefore, it is so important to keep the activity of the virus under control and properly stimulate the immune defense.
Diagnostics
To diagnose HPV, first contact a physician. Depending on the manifestations of the virus, he will refer the patient for diagnostic tests and to a specialist (gynecologist, urologist, dermatologist, oncologist, proctologist, etc.).
Both women and men may be prescribed tests such as:
- Enzyme immunoassay blood test - its results cannot determine the concentration and oncogenicity of the virus, but antibodies to it can be detected; the method is ideal for early diagnosis, when symptoms have not yet appeared.
- PCR diagnostics – allows you to detect HPV DNA, that is, it allows you to accurately find out whether there is a virus in the body or not; Blood, saliva, genital secretions, etc. are taken for analysis.
- Digene test – allows you to assess the degree of oncogenicity of the strain and determine the amount of virus in the body; The biomaterial is a piece of tissue scraped from the cervical canal, vagina or urethra.
Women are prescribed the following types of examination:
- Cytological examination (PAP test) - examination of a vaginal smear under a microscope to identify cells altered by the virus.
- Colposcopy is an examination of the cervix using a colposcope; this procedure is prescribed to the patient if, according to the results of a cytological examination, altered cells were detected.
Is there a cure for human papillomavirus?
In order to understand how HPV is currently treated in women, you should understand what approaches exist in the treatment of human papillomavirus infection. At the moment, therapy for HPV infection comes down to the following measures:
- prevention of progression of HPV infection;
- elimination of clinical manifestations;
- stimulation of systemic and local antiviral immunity.
There are no drugs that lead to the complete disappearance of the virus from the body. However, research in this area is ongoing - the focus of doctors is on the need for combined treatment of various manifestations of HPV. Research in the field of genetic engineering is promising. Scientists are considering the possibility of “rewriting” the virus code to self-destruct instead of spreading. Reducing viral copies restores local immunity and eliminates chronic inflammation.
Information for doctors on the topic “How to treat HPV in women” is currently described in detail in current clinical guidelines.
Treatment
There is no specific treatment for HPV (that is, aimed at its destruction). However, measures can be taken to suppress the activity of the virus and increase the likelihood of self-healing. The patient is prescribed:
- Vitamins.
- Immunomodulators.
- Antiviral drugs.
Symptomatic treatment is also carried out - removal of tumors. Under no circumstances should you try to treat condylomas, papillomas and warts with folk remedies. There is a risk of provoking the development of a secondary infection or the degeneration of a benign tumor into a malignant one.
The following methods are used to eliminate tumors:
- Removal using a scalpel.
- Cryodestruction (freezing with liquid nitrogen).
- Removal with a radio knife.
- Laser removal.
- Electrocoagulation.
The method is chosen by the doctor depending on the nature and location of the tumor, as well as the condition of the patient’s body.
Advantages of the Private Practice Clinic
- Certification in all areas of work.
- The consultation is conducted by experienced dermatovenerologists and gynecologists.
- The latest methods of treating diseases.
- Possibility of removing papillomas and condylomas using all currently known modern methods without pain and serious scars.
- Results of express tests on the day of treatment.
- Individual approach to each patient.
- Polite and friendly staff.
- You can undergo diagnosis and treatment anonymously.
- Convenient location of the clinic in the center of Moscow and Southern Administrative District.
- Parking for visitors to the medical center.
Prevention
Preventive methods include maintaining a healthy lifestyle and regularly strengthening the immune system through a nutritious and varied diet, moderate physical activity, and quality rest. It is important to observe the rules of personal hygiene and not use other people’s equipment. To avoid the risk of infection, you should avoid casual sex and use barrier contraception.
Also nowadays it is possible to vaccinate against some highly oncogenic strains of HPV. Vaccinations are recommended between the ages of 9 and 26 years (the optimal age is 11-12 years). Women can get vaccinated after 26 years of age, but only if the gynecologist believes there is an indication. It should be borne in mind that vaccination does not cure the virus already present in the body, but prevents infection with some particularly dangerous types.
Important numbers: the statistics are scary
- In the last 10 years, the number of people infected with hpv
has increased 12-fold. - HPV ranks second after genital herpes among all female infections and is found in 70% of adult women.
- Papillomavirus is the cause of all cases of cervical cancer.
- HPV is associated with 50% of anogenital cancers.
- The greatest risk of infection is between the ages of 18 and 25. The peak age for development of cervical dysplasia is 30 years, and cervical cancer is 45 years.