August 31, 2020
Chlamydia is an infection transmitted primarily through sexual contact; the causative agent is chlamydia (Chlamydia trachomatis).
From the article you will learn what kind of disease this is, why it is dangerous and how it is transmitted. Chlamydia is an infection transmitted primarily through sexual contact; the causative agent is chlamydia (Chlamydia trachomatis). According to WHO, urogenital chlamydia is one of the most common diseases among STDs. Absolutely all sexually active people can get chlamydia; the greater the number of sexual partners, the higher the risk of infection. About 75% of new cases of the disease are registered among women under 25 years of age, and by the age of 30, approximately 50% of sexually active women have the disease. For sexually active men, the risk of infection is highest between the ages of 20 and 24 years.
Chlamydia trachomatis is able to actively multiply in healthy human cells and absorb from them all the enzymes necessary for its life. The incubation period for the development of chlamydia ranges from 5-7 days to 3-6 weeks (on average 20-30 days). According to doctors, the main way of contracting chlamydia is through sexual contact. However, chlamydia can enter the human body through everyday life or from mother to child, during its passage through the birth canal, inseminated by pathogenic bacteria.
The following methods of transmission of infection are officially registered:
- Sexual contact, including vaginal, anal and oral sex. The probability of transmission from a single sexual act is 68% from an infected woman to a man and 25% from an infected man to a woman.
- “Vertical” during childbirth - infection of newborns (conjunctivitis or pneumonia) during childbirth from a sick mother while passing through the birth canal.
- The contact and household route of infection with chlamydia is rarely recorded: through bedding and toiletries, underwear, etc. Cases of infection of the mucous membrane of the conjunctiva of the eye (discharge from the genital organs) have been described.
What is chlamydia
Chlamydia is a bacterial disease that is transmitted primarily through sexual contact. In this case, the organs of the genitourinary system come under attack. Most often, chlamydia affects the urethra and cervix. With the development of an ascending infection, the seminal vesicles, prostate gland, testicles and uterine appendages can be affected. Despite the fact that the disease manifests itself predominantly as multifocal lesions of the genitourinary system, other organs can also suffer when infected with chlamydia:
- conjunctiva,
- rectum,
- Airways,
- The lymph nodes,
- liver,
- nervous system,
- the cardiovascular system.
There are also cases of joint damage, which are often confused with ordinary arthritis. The course of a chlamydial infection largely depends on the specific pathogen and how it enters the body. Read more about the different types of chlamydia in our main article on this disease.
Pathogen
The disease is caused by bacteria of the genera Chlamydia and Chlamydophila. They parasitize and multiply in the cells of their host, which can be not only humans, but also animals and birds.
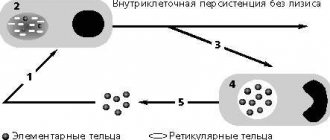
The most important human enemy among chlamydia is the causative agent of genitourinary chlamydia, Chlamydia trachomatis. Its “favorite” places of penetration include the epithelial tissue of the fallopian tubes, urethra and rectum. Penetrating into the host epithelial cell, chlamydia begins to feed on its energy resources. Then they enter the intercellular space in order to infect new cells - this process develops quite rapidly, determining the duration of the incubation period and the clinical picture of the disease. Chlamydia destroys a healthy epithelial cell within 2-3 days, after which a new reproduction cycle begins, which usually does not exceed 48 hours.
Boosting immunity after chlamydia
During the disease, the immune system deteriorates significantly, so to improve immunity, drugs that enhance immunity are prescribed - immunomodulators.
The complex course of treatment includes one of the immunomodulators:
Polyoxidonium. Promotes increased immune defense and more active production of antibodies. The drug stimulates the activity of blood phagocytes, reduces the toxic effects of other drugs on liver cells. Administration is carried out according to the following scheme: 1 time every two days, intramuscularly at a dosage of 6 mg. Polyoxidonium is contraindicated during pregnancy and breastfeeding; Timalin. The drug enhances cellular immunity and enhances phagocytosis. The course is 10 days. Dosage – intramuscularly 5 – 20 mg, daily. Contraindication is individual intolerance to the components. During therapy, it is possible that signs of allergy may develop.
Vitamin complex for chlamydia
To improve immunity, it is not enough to take only immunomodulators; it is necessary to provide the body with the necessary vitamins and microelements. The doctor himself prescribes a vitamin complex, often “Aevit” and “Vitrum”.
Aevit - vitamins A and E. Help improve immunity and strengthen the cardiovascular system. You need to take the vitamin 2 times a day, one tablet. Contraindications to the use of “Aevita” are intolerance to one of the components of the drug, circulatory disorders and thromboembolism diagnosed. Problems with the digestive tract may occur.
Vitrum is a vitamin complex that provides the body with all the necessary vitamins and strengthens the immune system. The duration of the course of taking the drug is individual, the dosage is two tablets once a day. As with taking Aevit, this drug has similar contraindications: intolerance to components, heart failure, as well as tuberculosis, sarcoma, thrombophlebitis. In case of overdose, adverse reactions are possible in the form of skin rashes and itching.
Routes of infection
Due to their two-phase life cycle, chlamydia adapts well to unfavorable environmental conditions, so you can acquire these “little rascals” even when using someone else’s soap.
According to statistics, every year an average of 100,000,000 (!) cases of infection are recorded worldwide.
Sexual tract
The greatest chance of contracting chlamydia occurs during sex with an infected partner. The urethra and pelvic organs are most often affected; the disease is caused by the bacteria Chlamydia trachomatis.
From mother to child
A child can get chlamydia from the mother while in the womb, during childbirth, or through breast milk. In this case, the respiratory system, conjunctiva, joints, and genitals may be affected.
Household way
Contact and household transmission is less common. Typically, people who have frequent contact with birds are susceptible to infection, since many birds, such as ducks and chickens, are also susceptible to chlamydia (its other name is psittacosis). Ornithosis is caused by the bacteria Chlamydophila psittaci. Typically, infection occurs in poultry farms, where people constantly inhale dust that contains microscopic particles of bird droppings. Children in families that keep feathered pets also often suffer from psittacosis. In addition to the respiratory system, the disease in this case often affects the eyes.
Contact path
This includes all methods of transmission when the cause of infection is direct or indirect contact with the biological fluids of a sick person. This is primarily a contact and household route of transmission, when common personal hygiene items become the source of infection. The term “chlamydia family” appeared because children often become carriers of the infection, having become infected at home from their parents.
Airborne path
The airborne route of transmission of chlamydia is characteristic of the bacteria Chlamydophila pneumoniae, which is one of the causes of bacterial pneumonia.
Classification of chlamydia
Many people think that chlamydia affects only the genitourinary organs, but in fact this is not the case. All chlamydia are included in the order Chlamydiales. One of the families Chlamydiaceae, genus Chlamydia and Chlamydophilia, includes several species of microorganisms, including:
- Chlamydia psittaci
- Chlamydia pneumonia
- Chlamydia pecorum
- Chlamydia trachomatis
C.psittaci can lead to the development of atypical pneumonia, pyelonephritis, encephalomyocarditis and arthritis, C.pneumonia causes the development of acute respiratory diseases and one form of pneumonia, and C.pecorum is currently poorly understood and is associated with diseases in cattle. The role of this microorganism in the pathogenesis of human inflammation is unknown.
The extensive subgroup C. trachomatis includes more than 15 species of the pathogen, which is the most significant pathogen for humans and is capable of infecting internal and external organs, causing a number of dangerous diseases, including UGC.iii
Symptoms of chlamydia
The incubation period of the disease is on average 1-2 weeks, but sometimes it can last up to a month. After this, the disease progresses, often without causing any clinical manifestations.
Asymptomatic progression is an extremely unpleasant feature of chlamydia. According to data from various sources, this is from up to 80% of all cases of infection. It would seem that what's wrong with this? If there are no symptoms, why get treatment? But it's not that simple. Firstly, in such situations, the risk of infection of the patient’s immediate environment increases - after all, he does not yet know about his illness. Secondly, chlamydia does not go away on its own, and its late diagnosis is always fraught with an additional risk of severe complications.
Important! Since chlamydia is often asymptomatic, it is advisable for women at the stage of planning pregnancy to undergo screening for the presence of sexually transmitted diseases. Even if there are no signs of chlamydia, it is better to play it safe to prevent infection of the fetus, because the disease is not only transmitted through sexual contact.
It should also be borne in mind that the symptoms of chlamydia can often be nonspecific, that is, they resemble the symptoms of other diseases. Therefore, if after accidental sexual contact a sore throat appears or the mucous membrane of the eyes becomes inflamed for no apparent reason, you should immediately consult a doctor (his specialization will depend on the nature of the symptoms). This must be done even if a condom was used during sex - it significantly reduces the risk of infection, but does not provide a 100% guarantee of safety.
In men
Typically, the clinical manifestations of chlamydia in men resemble chronic inflammation of the urethra - urethritis. The following symptoms are noted:
- scanty translucent discharge from the urethra,
- moderate pain, aggravated by urination (pain can radiate to the rectum),
- the urine is cloudy, may contain minor impurities of pus or blood,
- intoxication is manifested by general weakness and an increase in temperature to an average of 37.5 oC,
- in rare cases, swelling of the scrotum and pain in the testicles, radiating to the lower back, may be observed,
- after unprotected anal intercourse, symptoms reminiscent of proctitis are observed - pain and itching in the rectum, as well as purulent and/or bloody discharge.
Upon examination, the mucous membrane of the patient’s external urethral opening is red and swollen.
If these symptoms quickly go away without treatment, this does not mean that the body has coped with the infection on its own and the problem can be forgotten. Most often, the sudden “self-removal” of clinical signs of chlamydia means that the disease has become latent.
Among women
A characteristic feature of the clinical manifestations of chlamydia in women is nagging pain in the lower abdomen, reminiscent of sensations on the eve of menstruation. Other symptoms:
- itching and pain in the vagina,
- thick mucus discharge from the urethra (their quantity increases over time, the color changes to yellowish-green, a sharp unpleasant odor appears),
- frequent and painful urination,
- weakness and slight increase in temperature,
- intermenstrual bleeding from the genital tract.
Upon visual examination, the mucous membrane of the external opening of the urethra is swollen, hyperemia (redness) is noted. On endoscopic examination: ulcerations on the mucous membrane of the cervix, swelling and redness, mucous discharge mixed with pus.
If infection occurs during oral or anal intercourse, pain in the throat and rectum may appear, respectively.
Abnormal discharge due to chlamydia
The incubation period for the disease is quite long: from two to four weeks, so abnormal discharge does not appear immediately. The discharge is initially colorless and transparent, over time it may change to dark brown (purulent impurities), it may have an unpleasant odor, which may indicate gonorrhea. The discharge may become sticky, which indicates that secondary infections have occurred.
Important! Changes in vaginal mucus can be noticed only a week or two after infection. But, as previously noted, the disease in most cases is asymptomatic.
Diagnostics
Discharge from the urethra, the first portion of urine, prostate secretion (in men) and discharge from the cervical canal (in women) are used as research material. There are several methods that are currently considered the most effective in diagnosing chlamydia.
- Urogenital smear. This universal diagnostic method is PCR (polymerase chain reaction), with the help of which chlamydia DNA is determined in biomaterial. The undeniable advantage of the method is that the DNA of each microorganism is unique, which means that the analysis will be specific. Simply put, in this case chlamydia cannot be confused with other bacteria.
- Enzyme-linked immunosorbent test (ELISA). The method is based on the determination of immunoglobulins IgM and IgG. These are antibodies that are produced by the body's immune system in response to the activity of pathogenic microorganisms. The main disadvantage of the method is the possibility of obtaining false positive results.
- Cultural method (bacteria culture). The essence of the method: a scraping of epithelial cells from the urethra is taken from the patient (the procedure is unpleasant, but short). The resulting biomaterial is inoculated on a nutrient medium, which is then placed in an incubator. If after a few days chlamydia colonies begin to multiply on the surface of the nutrient medium, the laboratory technician has every reason to tell the patient the unpleasant news. Due to its high reliability, the culture method is considered the gold standard for diagnosing chlamydia.
- Microscopy. This method is considered outdated, since chlamydia, among other pathogenic microorganisms, is not distinguished by its size, and therefore it can be determined under a microscope in approximately 30% of observations. The only advantage of the method is that the cost of the study is low, so in most government institutions microscopy is performed free of charge.
- RIF (immunofluorescence reaction). A smear is taken from the patient's urethra, after which antibodies that recognize chlamydia protein are added to the resulting biomaterial. For convenience, they are marked with a fluorescent marker, so if the biomaterial actually contains chlamydia, luminous antibodies recognize them and form an “antigen-antibody” complex. In this case, a sample of biomaterial will sparkle under the microscope lenses, like a Christmas tree. The disadvantage of the method is low reliability (40-50%).
- Express tests. In recent years, tests have appeared on the market that help identify chlamydia even at home. The result can be obtained within 15 minutes, and the manufacturer claims high reliability and specificity of rapid tests (90-95%, respectively).
Important! The patient's sexual partner must also be diagnosed.
Advantages of prevention and treatment of chlamydia at the Medical Center
Needless to say, chlamydia should be treated by a qualified doctor, since any diseases of the genital organs are fraught with serious consequences, including infertility. Our Medical Center has collected and developed unique methods for the treatment of chlamydia, which combine all the latest progressive developments in the fight against this disease. They contain medical procedures, drug therapy, physiotherapeutic procedures, recommendations on diet and daily routine.
In our Medical Center you will find the following:
highly qualified specialists with many years of successful experience; high-tech modern equipment that allows accurate diagnostics; optimal prices and high quality of treatment; individual approach to each case of disease; treatment is carried out comprehensively, it includes both traditional and modern medical methods, as well as alternative and preventive ones; accompanying the patient during relapses, including hospitalization in the best clinics in the city; attentive, friendly staff, always strictly observing medical confidentiality.
Don't delay visiting the doctor! Only timely and adequate treatment contributes to recovery and complete cure of the disease. Since the main treatment for chlamydia is antibacterial agents, self-medication is inappropriate in this case. Many chlamydia are resistant to certain groups of antibiotics, so drugs are prescribed purely individually. Your health is in your hands. Treat chlamydia responsibly. After all, its complications will darken your life for many years. And we will help you overcome this illness. Our goal is to give people back the joy of a full life and regain self-confidence.
Treatment
The main goal in the treatment of chlamydia is the eradication of Chlamydia psittaci and Chlamydia trachomatis, that is, the complete destruction of these bacteria. Antibiotics are used for this purpose.
Antimicrobial therapy
The specific drug and antibiotic regimen are selected by the doctor individually for each patient. Chlamydia has the worst relationship with tetracyclines and macrolides, which is why they are first-line drugs. As an alternative, fluoroquinolone antibiotics are used.
Chlamydia is a sexually transmitted disease, which means all sexual partners should be treated for it.
Treatment of chlamydia, like many other sexually transmitted infections, involves:
- Refusal of sexual intercourse for the entire period of therapy.
- Treatment of all sexual partners of the patient (if he had sexual contact with the patient within 60 days before diagnosis).
- A control smear for PCR analysis after completion of treatment (3-4 weeks after the end of therapy for pregnant women, and 3-4 months later for all others).
Additional methods and means of treatment
In addition to systemic treatment with antibiotics, local therapy is also used for chlamydia. The most common methods:
- washing the urethra with disinfectant solutions in men and women (for example, furatsilin or chamomile decoction),
- vaginal tampons with tetracycline,
- indomethacin suppositories to reduce itching and swelling.
After completing the course of treatment, men are recommended to massage the prostate gland.
Restoration of microflora after taking antibiotics
To restore the intestinal microflora during and after taking antibiotics, probiotic preparations containing live lacto- and bifidobacteria can be prescribed. For women, it is also possible to use vaginal suppositories and capsules.
Diet for chlamydia
Chlamydia should be treated in conjunction with a transition to a balanced diet. First of all, oddly enough, it is necessary to exclude any dairy products. The fact is that lactic acid bacteria help chlamydia develop resistance to antibiotics. Quite expected restrictions apply to alcohol, fried, fatty and smoked foods - you will have to forget about them during treatment.
Recommended products (Fig. 1):
- fruits and vegetables,
- any cereals (buckwheat, oatmeal, pearl barley are best),
- lean meat (turkey, chicken, beef),
- seafood.
Figure 1. Recommended foods for people with chlamydia: vegetables, grains, lean meats. Photo: Marta Cuesta/Pixabay
Treatment at home
It is not recommended to treat chlamydia on your own. Home remedies are not proven to be effective. Treatment with folk remedies can only aggravate the problem and lead to complications. During therapy, you can take vitamins in consultation with your doctor, drink chamomile tea or take chamomile baths.
Immunomodulatory drugs
Chlamydia is NOT treated with immunomodulatory drugs. This is ineffective and does not give a positive result. The basis of treatment is antibiotic therapy.
Immunomodulators in the treatment of chlamydial infection
They are used both to correct immune disorders caused by the infectious process and to increase the effectiveness of anti-chlamydial antibiotic therapy.
The fact is that when a patient starts taking antibiotics, chlamydia stops transforming into its active form, which is precisely sensitive to them. He waits out the course of treatment for chlamydia, and then the pathological process is activated again and resumes.
Immunomodulators are designed to artificially increase the activity of infectious inflammation to improve the availability of chlamydia trachomatis to antibiotics.
The most commonly used immune drugs are:
- Polyoxidonium 6 mg intravenously.
- Cycloferon 12.5% -2 ml intramuscularly or intravenously.
- Timalin intramuscularly.
- Pyrogenal according to the intramuscular route.
The frequency of administration and dosage, as well as the relationship with antibiotic therapy and local treatment, depend on the specific situation.
What are the consequences of chlamydia if left untreated?
In the absence of timely treatment, chlamydia can be fraught with a number of unpleasant complications. As we already know, the disease is very often asymptomatic, so the risk of unpleasant consequences is quite high.
One of the most common complications of chlamydia is Reiter's syndrome (Fig. 2). It manifests itself as a combination of symptoms of conjunctivitis (inflammation of the mucous membrane of the eyes), arthritis (inflammation of the joints) and urethritis (inflammation of the urethra).
Figure 2. Reiter's syndrome is a complication of chlamydial infection. Photo: metmuseum.org
Consequences in men
The most common complications in men are:
- inflammation of the testicles and their appendages (orchiepididymitis),
- narrowing of the prostate ducts,
- chronic prostatitis,
- narrowing of the urethra (can only be treated surgically).
Consequences in women
If chlamydia is not treated for a long time, women may experience the spread of infection to the uterus, its appendages and fallopian tubes with further formation of adhesions in them. This, in turn, can lead to infertility or ectopic pregnancy. In severe cases, the inflammatory process spreads to the peritoneum, causing peritonitis and inflammation of the fibrous capsule of the liver (perihepatitis). The process is accompanied by the accumulation of fluid in the abdominal cavity. In medicine, this complication is called Fitz-Hugh-Curtis syndrome.
Consequences during pregnancy
Pregnant women may experience complications such as congenital chlamydia in the child, as well as an interrupted pregnancy (miscarriage).
HOW IS CHLAMYDIA TRANSMITTED?
Chlamydia is transmitted mainly sexually, also through blood, through damage to the integrity of the skin (at a surgeon, dentist, cosmetologist, etc.).
Chlamydia is capable of contaminating sperm, that is, attaching to them, and due to this, rapidly disseminating (spreading) throughout all parts of the reproductive system. For infection, only one unprotected sexual intercourse is enough. There is a risk of transmitting the disease to the child: transplacentally (during gestation through the placenta) and intrapartum (during childbirth during the passage of the fetus). If bacteria is detected in one of the partners, both should be tested. A gynecologist for a woman and a urologist for a man must examine the genital organs to detect manifestations of the inflammatory process, for example, hyperemia, swelling, and discharge. If in the past a married couple has had miscarriages, pregnancy pathologies, has infertility, or it turns out that the partner suffers from urogenital inflammation, then a comprehensive examination is prescribed. It includes general blood and urine tests, bacterioscopic analysis of vaginal discharge (smear), culture for dysbacteriosis and determination of susceptibility to antibiotics, as well as PCR diagnostics (smear from the affected area of the genital mucosa).
Prevention
First of all, reasonable caution should be exercised in choosing sexual partners. Using a condom significantly reduces the risk of infection, but does not provide a complete guarantee of safety. Therefore, after sexual contacts with unfamiliar people, it is better to play it safe and get diagnosed - this will help avoid unpleasant complications.
Regular health screening is also recommended for people who have close contact with our feathered cousins. This applies to both poultry farm workers and poultry owners. Symptoms such as pain when urinating, inflammation of the conjunctiva and joint pain should cause particular concern. In this case, it is better not to delay the diagnosis.
Chronic chlamydia: ways of spread
Outside the human or animal body, chlamydia quickly dies. They are sensitive to high temperatures and die within one minute at a temperature of 100 °C. At 60-70 °C, ten minutes of exposure is sufficient. Antiseptics, disinfectants containing 70% alcohol, hydrogen peroxide and chloramine solution can also be successfully used against this infection.
Established routes of transmission of infection are sexual contact through vaginal, anal and, less commonly, oral contact, as well as airborne droplets and household contact. According to one version, the probability of infection through unprotected sexual contact with a patient with UGC is more than 50%. Women, due to their anatomical characteristics, are more susceptible to this disease. Newborns can become infected when the fetus passes through the birth canal of an infected mother.
The incubation period of this infection lasts on average from two weeks to a month.iv Among the main features of chlamydial infection is the complex molecular-membrane mechanism of interaction of the microorganism with the host cells. Very often, this infection becomes chronic due to the fact that it is capable of long-term persistence – long-term survival and remaining in a functionally active state in the host’s body. This means that treatment of this disease may require several courses repeated one after another.
The most common reasons for the development of UHH are neglect of the principles of safe sex, sexual hygiene, uncontrolled use of medications and self-medication.
Types of chlamydia and features of its course
Chlamydia has 15 subspecies, which can cause several infectious and inflammatory diseases - urogenital chlamydia, lymphogranulomatosis venereum, eye diseases (trachoma), damage to the rectum. Some forms can provoke pneumonia and acute respiratory pathologies. Two types of these microorganisms can be transmitted from animals and birds to humans, causing a deadly disease - psittacosis.
Urogenital chlamydia, which affects the human genitourinary system, is one of the most common and frequently encountered types in clinical practice. This disease belongs to the group of sexually transmitted diseases. The main source of infection with chlamydia of the genitourinary system is a sick person with whom another had unprotected sexual contact. It does not matter what type of contact was present (genital, oral, anal), if it was carried out without a condom, the probability of infection is 100%. Cases of household infection with chlamydia through bedding have been diagnosed, but this occurs quite rarely.
Chlamydia has two types of progression - acute and chronic. The most common form is the chronic form, and in women in the vast majority of cases. The main danger of chlamydia lies in this factor; the chronic form in men and women for a long period of time passes hidden and is practically asymptomatic. That is, an infected person considers himself healthy, does not begin treatment, and at this time the pathology gradually progresses, covering more and more new tissues and internal organs.
It is impossible to detect the disease using conventional infection tests, since chlamydia is an intracellular microorganism. To detect them, an analysis of a scraping of the mucous membranes of the urethra is necessary; a smear examination is not enough.
The advent of research techniques using polymerase chain reaction (PCR) has made it possible to detect the presence of any pathogenic microorganisms in patient biomaterials with very high accuracy. It is possible to detect chlamydia using PCR even at the earliest stages of the disease; the high sensitivity of this test makes it possible to determine the presence of chlamydia even when their number is extremely small.
Used sources
- Dermatovenerology. National leadership. Brief edition / ed. Yu. S. Butova, Yu. K. Skripkina, O. L. Ivanova - M.: GEOTAR-Media, 2013. - 896 p.
- Skin and venereal diseases. Textbook for students of higher medical educational institutions. / E. S. Kozorez - M.: Publishing house VLADOS-Press, 2005. - 173 p.
- Dermatovenerology. Scientific and practical publication. / ed. A. A. Kubanova, V. A. Samsonova - M.: Publishing house "GEOTAR-Media", 2006. - 311 p.
- Clinical recommendations for the management of patients with sexually transmitted infections and urogenital infections / Russian Society of Dermatovenerologists and Cosmetologists - M.: Business Express, 2012. - 112 p.
- Syphilis and sexually transmitted infections: atlas / under general. ed. prof. N.V. Kungurova. – Ekaterinburg: Ural Publishing House. Univ., 2015. – 184 p.