Secondary syphilis
The development of secondary syphilis often begins with general symptoms similar to those of acute respiratory viral infection or influenza. This is malaise, fever, chills, headache. A distinctive feature of secondary syphilis is arthralgia and myalgia, which worsen at night. Only a week after the appearance of these prodromal symptoms do skin manifestations of secondary syphilis occur.
Rashes of secondary syphilis - secondary syphilides - are characterized by significant polymorphism. At the same time, they have a number of similar characteristics: a benign course without peripheral growth and destruction of surrounding tissues, a rounded shape and clear demarcation from the surrounding skin, the absence of subjective symptoms (occasionally slight itching is noted) and acute inflammatory signs, healing without scar formation. Secondary syphilides contain a high concentration of pale treponema and cause a high infectious danger for a patient with secondary syphilis.
The most common form of rash associated with secondary syphilis is syphilitic roseola.
or spotted syphilide, manifested by rounded pale pink spots with a diameter of up to 10 mm. They are usually localized on the skin of the limbs and torso, but can be on the face, feet and hands. Roseolas with secondary syphilis appear gradually, 10-12 pieces per day for a week. Typically, roseola disappears when pressure is applied to it. Rarer forms of roseola rash in secondary syphilis include scaly and raised roseola. The first has a small depression in the center and is covered with lamellar scales, the second rises above the general level of the skin, which makes it look like a blister.
The second most common cause of secondary syphilis is papular syphilide.
. Its most typical form is lenticular, having the appearance of densely elastic papules with a diameter of 3-5 mm of pink or copper-red color. Over time, peeling begins in the center of the papules of secondary syphilis, which spreads to the periphery. A “Biette collar” is characteristic - peeling along the edge of the papule while in the center it has already ended. Resolution of papules ends with the formation of long-lasting hyperpigmentation. Rarer forms of papular syphilide include seborrheic, coin-shaped, psoriasiform, weeping syphilide, papular syphilide of the palms and soles, as well as condylomas lata.
A rare form of secondary syphilis rash is pustular syphilide.
. Its appearance is usually observed in weakened patients (tuberculosis patients, drug addicts, alcoholics) and indicates a more severe course of secondary syphilis. Pustular syphilide is characterized by the presence of purulent exudate, which dries to form a yellowish crust. The clinical picture resembles manifestations of pyoderma. Pustular syphilide of secondary syphilis can have the following forms: impetiginous, acne-like, ectymatous, smallpox, rupoid.
With recurrent secondary syphilis, pigmentary syphilide
(syphilitic leukoderma), appearing on the side and back of the neck in the form of rounded whitish spots, called the “necklace of Venus”.
Skin manifestations of secondary syphilis are accompanied by generalized enlargement of the lymph nodes (lymphadenitis). Enlarged cervical, axillary, femoral, and inguinal lymph nodes remain painless and are not fused with the surrounding tissues. Impaired nutrition of the hair roots in secondary syphilis leads to hair loss with the development of diffuse or focal alopecia. Lesions of the mucous membranes of the oral cavity (oral syphilis) and larynx are often observed. The latter cause characteristic hoarseness in patients with secondary syphilis.
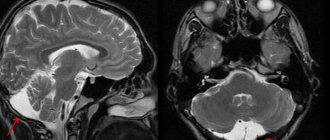
On the part of the somatic organs, mainly functional changes are observed, which quickly disappear during treatment and are absent during periods of latent secondary syphilis. Liver damage is manifested by its soreness and enlargement, and impaired liver function tests. Gastritis and gastrointestinal dyskinesia are often observed. From the kidneys, proteinuria and the occurrence of lipoid nephrosis are possible. Damage to the nervous system is manifested by irritability and sleep disturbances. Some patients with secondary syphilis experience syphilitic meningitis, which is easily treatable. Damage to the skeletal system is possible with the development of osteoperiostitis and periostitis, manifested by night pain mainly in the bones of the extremities and occurring without bone deformities. In some cases of secondary syphilis, otitis media, dry pleurisy, retinitis, and neurosyphilis may occur.
Causes of the disease
The causative agent of syphilis is Treponema pallidum or Treponema pallidum.
This bacterium resembles a spiral in shape, it can move, and reproduces by division. When it enters the body, it settles in the lymph nodes. It begins to show up in the blood much later. Treponema is practically unviable in the environment. It does not tolerate heat, light, or drying, but at room temperature it remains mobile for up to 12 hours. Sensitive to antibiotics and almost all antiseptics. But treponema tolerates low temperatures well. It is an anaerobic - it does not require oxygen to live and reproduce.
Most often, syphilis is transmitted sexually, which makes it possible to classify it as a sexually transmitted disease. This method of infection accounts for up to 98% of all diagnosed cases.
However, there are known facts of transmission from an infected person, as well as among drug addicts who use the same syringe when injecting drugs, in everyday life when using toothbrushes or razors with blood residues on them.
Household transmission of syphilis is extremely rare and most often occurs through close contact with a patient who already has tertiary syphilis. Treponema pallidum is found in saliva only in the presence of ulcers in the oral cavity, but is absent in urine, sweat and feces.
The cause of syphilis infection can be the milk of a woman nursing her baby. There are also known cases of transmission of the disease from a patient to a fetus during pregnancy.
Which doctor will help if symptoms of syphilis appear?
Often people who suspect they have a disease wonder which doctor to see.
First of all, you should visit a doctor specializing in venereology.
It is his area of work that includes syphilis and any of its manifestations.
The doctor will be able to soberly assess the symptoms and give recommendations regarding diagnosis.
Then, when the diagnosis is known reliably, treatment is recommended.
In addition to a venereologist, you can contact a syphilidologist.
This doctor specializes exclusively in syphilis and its various manifestations.
Unfortunately, not all hospitals have syphilidologists, and therefore it is easier and faster to visit a venereologist.
In addition to a venereologist and syphilidologist, you can contact a urologist or gynecologist.
These doctors are also familiar with sexually transmitted diseases, including syphilis, and can guide the patient regarding the diagnosis and treatment of the disease.
This is especially true if the hospital for some reason does not have a venereologist, and there is no opportunity to get an appointment with him in the near future.
Treatment
It should be noted: in advanced cases, when it is not possible to get rid of chancre, as well as with extensive tissue necrosis, they resort to surgical removal of syphiloma.
In all other cases, the chancre itself is not treated and specific treatment for uncomplicated chancre is not carried out. For secondary and combined infections, topical antibacterial drugs may be prescribed: baths with benzylpenicillin and dimexide, applications with mercury or mercury-bismuth ointment. If the chancre is located in the oral cavity, rinsing is recommended: a solution of furatsilin, boric acid (2%), or gramicidin (2%).
The main task is to get rid of syphilis as quickly as possible and with minimal losses. Therefore, to treat syphilis, penicillin antibiotics are used - short and long-acting (durant) penicillins: Bicillin-1, Bicillin-5, Oxacillin, Ampicillin (semi-synthetic penicillin). The drug of choice for the treatment of syphilis is benzylpenicillin.
Reserve drugs for penicillin intolerance: tetracyclines (doxycycline), macrolides (azithromycin, erythromycin), cephalosporins (ceftriaxone).
Administration of drugs is by injection - intravenous or intramuscular.
Source: CC0 Public Domain
The treatment regimen depends on the stage of the disease, location, degree of damage, etc. In any case, the dose of the drug and the number of courses of treatment are calculated by the doctor individually.
During treatment, control tests are carried out to confirm the effectiveness of the drugs.
Treatment of syphilis at an early stage is the most effective and creates all the prerequisites for a complete cure without consequences and complications.
Recommendations for the treatment period
During the treatment period, it is necessary to stop sexual intercourse. When chancre is localized on the fingers, it is recommended to wear protective gloves. If syphiloma is found in the mouth, it is necessary to separate personal items from common ones - dishes, toothbrushes, etc.
If there are chancres on the body, the use of bed linen, towels, and washcloths should be individual. Syphilis is not transmitted through public places (toilet, etc.).
Sexual partners of sick people receive preventive treatment without fail, including pregnant and lactating women.
Important! You should definitely complete the full course of treatment! Under no circumstances will syphilis go away spontaneously. Untreated syphilis will move to the next stage, increasing the risk of complications and persistent deterioration of the patient’s condition.
Clinical serological control (CSC)
All family members of the sick person, both adults and children, need to receive preventive treatment after sexual or close household contact with patients with early forms of syphilis. 3 months after the end of preventive treatment, a single clinical and serological examination is carried out.
Clinical serological control (CSC) after the end of specific treatment of the patient is carried out once every 3 months during the first year of observation. Then once every 6 months in subsequent years with non-treponemal (simple serological) tests, once a year with the corresponding treponemal test (a complex test to identify possible latent forms of syphilis), which was used in diagnosing the disease. The duration of CSC is determined individually depending on the results of treatment.
Children born to seropositive mothers who did not have congenital syphilis, regardless of whether they received preventive treatment or not, are subject to observation for 1 year. Children receiving specific treatment are on CSC for 3 years.
Prevention
Since the mode of transmission of the disease is mainly sexual, preventive measures consist of maintaining fidelity to sexual partners - this is the most effective prevention of sexually transmitted diseases. When having sexual contact with an unverified person, you should always use a condom.
Barrier contraception (condom) provides almost 100% protection against syphilis infection.
In any case, after accidental contact, it is necessary to independently treat the genital area with antiseptic agents: miramistine or chlorhexidine.
If an unplanned contact occurs without protective equipment, or the integrity of the condom is damaged in the process, doctors recommend visiting a prenatal clinic as soon as possible and receiving a preventive injection, which will almost 100% prevent the development of syphilis.
Diagnostics
To prevent the diagnosis of syphilis from showing a false positive or false negative result, it is necessary to do this only with the help of modern tests in a laboratory that has all the necessary equipment and reagents:
- Determination of antibodies to Treponema pallidum in the passive hemagglutination reaction (PHA) in the blood is one of the most popular methods for diagnosing both primary and secondary or tertiary syphilis. Used to confirm or refute the diagnosis at any stage of the disease.
- Determination of antibodies to Treponema pallidum in the blood using the ICL method is used for screening diagnosis of the disease before hospitalization, during a medical examination and obtaining medical certificates, as well as for the primary diagnosis of the disease in the presence of chancroid.
- Determination of class M antibodies (lgM) to Treponema pallidum using the enzyme immunoassay method (ELISA) in the blood allows one to determine the presence of the disease with a 100% result.
- Syphilis in men can be diagnosed by determining the DNA of the pathogen in urethral discharge using the PCR method. Also scraping of epithelial cells is carried out in women, but here it can be the cervical canal or discharge from the vagina.
- Determination of antibodies to Treponema pallidum in non-treponema tests (RPR, RMP) in the blood allows you to determine primary, secondary or tertiary syphilis, but it is recommended to use specific tests to confirm the diagnosis.
- Determination of Treponema pallidum DNA in blood, biological fluids, secretions from mucous membranes (except genitals), cerebrospinal fluid and effusion using the PCR method is done in the presence of such a clear symptom as chancroid, as well as during pregnancy. The test is recommended to be taken during treatment to monitor the effect of prescribed medications.
- Prescribing and monitoring the course of treatment for sexually transmitted diseases and sexually transmitted diseases.
An analysis for syphilis should be done during the primary period no earlier than 2 weeks from the moment of infection.
Until then, even the most sensitive test will show a negative result. The fact is that primary syphilis is divided into two periods - seronegative, when it cannot be detected, and seropositive, in which the disease can already be diagnosed. Specific serological reactions in people who have recovered from the disease will always be positive. Therefore, they are not used to monitor the effectiveness of prescribed therapy.
Localization
Since syphilis is transmitted primarily through sexual contact, chancroid is most often localized on the genitals. However, clinical practice shows that syphilomas are almost as often found in the mouth and anus.
This means that chancre can appear anywhere, the place of its localization can be:
- penis and scrotum
- labia and clitoris
- posterior commissure and anal area
- pubis
- oral cavity: lips, gums, tongue and throat
- inner thighs
- chest and stomach
- face
- rarely - eyelids, conjunctiva of the eyes
Chancre can be located inside the genital organs, for example, on the walls of the vagina or cervix, then syphiloma is difficult to detect.
Will folk remedies help with syphilis?
Patients often ask whether the treatment regimen for primary syphilis can include folk remedies.
Doctors generally answer this question quite categorically.
No, it cannot, since folk remedies are ineffective and sometimes even harmful to the body affected by Treponema pallidum.
First of all, it is worth remembering that folk remedies cannot be an alternative to antibiotics.
Even if they are famous for their ability to destroy bacteria.
Their strength is not enough to completely eliminate Treponema pallidum from the body.
But they can significantly blur the symptoms, making it more difficult for the doctor to make a diagnosis and choose treatment.
It is also worth considering that some traditional medicine weakens the effect of medications, including antibiotics.
The result may be a rapid chronicization of the syphilitic process, which will only become more difficult to combat.
If the patient wants to supplement his treatment with folk remedies, he is strongly recommended to first consult with his doctor.
Only after the doctor's approval can you use any prescriptions against the background of basic drug therapy.
Symptoms of primary syphilis in women
Signs of the primary period of syphilis in women are generally quite typical.
Pay attention to yourself:
- erosive chancre localized in the labia majora area
- development of indurative edema - a painful form accompanied by a number of unpleasant symptoms, which is typical only for women and affects the labia
- formation of chancres with a dense base in the urethra if the bacterium enters the urethra
- the formation of syphilomas - clearly defined erosions - in the cervical area (a special feature is that syphiloma can only be detected by a gynecologist or venereologist during a vaginal examination), etc.
The peculiarity of all types of primary chancre is that they do not cause any discomfort.
Because of this, they may be ignored by patients for a long time.
For example, a woman may see specific formations on her labia, but not give them meaning.
Since they do not cause pain, do not release any fluids into the environment, do not itch or cause other discomfort.
What is important to distinguish chancroid from?
In modern medical practice, as doctors note, the disease often transforms, taking on very unexpected forms.
For example, multiple chancre may form, which was previously unusual for syphilis, which can confuse the doctor.
It is important to distinguish the disease from the following diseases:
- chancroid is a venereal disease, but caused by another pathogen and distributed mainly in the tropics
- genital herpes can resemble chancre, when many blisters merge into one large erosion
- a simple boil can also in appearance resemble a manifestation of primary syphilis, but is usually distinguished by severe pain that is difficult to ignore
- aphtha is an ulcerative lesion of the oral mucosa, which occurs in some people with chronic diseases or a pronounced decrease in immunity
- classic injury - damage to the mucous membranes, which may resemble a chancre in shape or structure, but is non-infectious in nature and does not pose an epidemiological danger
Differential diagnosis is carried out only under medical supervision.
In many cases, it is impossible to distinguish one disease from another independently, without a series of tests.