Humeroscapular periarthritis (ICD 10 code - M75) is the most common cause of pain in the shoulder joint against the background of dystrophic lesions of the cervical spine. Pain syndrome is difficult to treat and leads to a decrease in quality of life and ability to work. In patients, the range of motion in the shoulder joint is limited, and the function of the upper limb is impaired. At the Yusupov Hospital, examinations are carried out using the latest diagnostic devices from leading European and world manufacturers.
Doctors take an individual approach to choosing a treatment method for each patient. For drug therapy, effective drugs are used that have minimal side effects. Rehabilitation specialists use innovative methods of rehabilitation therapy aimed at relieving pain and restoring movement in the shoulder joint. The medical staff is attentive to the wishes of patients.
Humeral periarthritis accounts for approximately 70% of lesions of the shoulder joint. This disease affects both young and old people. The peak of the disease occurs at 40-50 years of age. Which doctor treats glenohumeral periarthritis? At the Yusupov Hospital, an orthopedist, rheumatologist, and rehabilitologist treat patients suffering from joint disease. Severe cases of glenohumeral periarthritis are discussed at a meeting of the Expert Council with the participation of professors and associate professors, doctors of the highest category.
Causes of glenohumeral periarthritis
Humeroscapular periarthritis can develop after a shoulder injury, sudden and excessive physical exertion, or forced long-term immobility. Typically, several days pass from the moment of injury or overload before pain and inflammation occur. An acute attack of pain lasts several weeks.
The following diseases can contribute to the development of the pathological process:
- Diabetes;
- Obesity,
- Pathology of internal organs.
In some diseases of the cardiovascular system (myocardial infarction, coronary heart disease, peripheral vascular pathology), blood circulation deteriorates, especially in the left shoulder area, and glenohumeral periarthritis occurs. A common cause of the disease is osteochondrosis of the cervical spine, intervertebral hernia. Damaged vertebral discs wear out over time and lose their elastic properties. The distance between them decreases, the vertebrae come closer and pinch the nerve endings. When nerves are pinched, a reflex spasm of blood vessels occurs and blood circulation is disrupted. Inflammation of the shoulder tendons causes pain.
There are several theories that explain the mechanism of development of glenohumeral periarthritis. Muscle overstrain, professional overload, macrotrauma and microtrauma cause reactive inflammation in the tissues located around the joint, and reflex muscle-tonic reactions in the muscles that fix it contribute to the development of the degenerative process. In tissues with poor blood supply, as a result of constant tension and microtrauma, ruptures of individual fibrils are observed, foci of necrosis, hyalinization and calcification of collagen fibers are formed. Local damage to the periarticular tissues in the shoulder area is caused by the fact that the short rotators of the shoulder and the biceps tendon are constantly exposed to high functional load, often under conditions of compression, since the tendons are located in a narrow space.
Surgical intervention
If there is an imbalance between the rotator cuff and its stabilizing muscles, arthroscopic subacromial decompression is performed. The operation is performed to increase the gap between the acromioclavicular joint and the head of the humerus. As a result, sufficient space is created for the smooth sliding of the tendons located on the rotator cuff muscles. This also becomes a prevention of further injury to connective tissue structures during excessive physical activity. Main indications for surgery:
- persistent pain syndrome that was not eliminated by NSAIDs and periarticular administration of glucocorticosteroids;
- recurrent glenohumeral periarthritis lasting more than six months;
- the patient’s professional activity involves frequent active movements of the shoulder joint;
- tendon rupture leading to dysfunction of the periosteal muscle;
- transosseous injury to the rotator cuff tendon;
- The resulting complication of the pathology is tunnel syndrome.
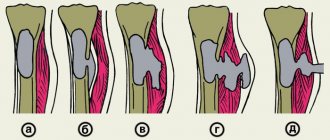
During the operation, the acromial end of the clavicle is removed to a length of less than 1.5 cm. The freed space is gradually filled with connective tissue, which leads to the formation of a kind of false joint. Its main function is to bind the connective tissue structures of the joint during movement.
The surgery is performed using miniature arthroscopic instruments inserted through punctures in the soft tissue. A few hours after suturing, the patient is discharged for further recovery at home. But sometimes, for better visualization of the surgical field, it is necessary to perform subacromial decompression in an open manner. In such cases, the patient remains in the hospital under the supervision of medical personnel for several days.
Symptoms and diagnosis of glenohumeral periarthritis
In the clinic of glenohumeral periarthritis, the main one is pain. The pain usually occurs for no apparent reason, sometimes at night, when lying on the painful side. It can be aching or sharp, intensifies with movement and radiates to the neck or upper limb. Pain may occur when the arm is abducted, placed behind the back or behind the head. Painful areas are identified in the teres major and pectoralis major muscles. Pain also occurs when the shoulder is abducted to 60-90°, which is associated with damage to the supraspinatus tendon.
The second important sign of glenohumeral periarthritis is contractures (stiffness) in the shoulder joint. The range of movements suffers sharply. When the arm is abducted, the scapula immediately moves (normally, it begins to rotate around its sagittal axis after the shoulder is abducted to 90°). The patient is unable to maintain the upper limb in lateral abduction. Rotation of the shoulder, especially inward, is difficult, but pendulum-like movements of the shoulder within 40° remain free.
When x-raying a joint, doctors identify the following signs:
- Osteosclerosis;
- Uneven or unclear bone contour;
- Deformation;
- Osteophytes (bone growths) at the sites of attachment of ligaments to the greater tubercle.
X-rays show osteoporosis in the area of the greater tuberosity or near the joint. Single or multiple clearings of bone tissue are visible in the area of the greater tubercle and humeral head, similar to a cyst. It is often possible to see calcifications in linear soft tissues. They are located under the acromion process of the scapula.
Doctors at the Yusupov Hospital make a diagnosis based on clinical manifestations and X-ray examination of the shoulder joint. In the most complex cases of glenohumeral periarthritis, magnetic resonance imaging is performed. It allows you to enhance the contrast of the image, which allows you to clearly differentiate soft tissue structures. The method avoids radiation exposure and provides horizontal, sagittal and frontal tomographic sections with reliable information about the magnitude of pathological changes.
Who's at risk
If a person’s occupation regularly overloads the shoulder joint, for example, working as a turner or painter, he automatically runs the risk of developing periarthrosis. Athletes performing similar exercises are exposed to the same risk. You should also think about the onset of shoulder arthrosis if:
- you are significantly overweight;
- you do not lead an active lifestyle or, on the contrary, are exposed to heavy physical activity;
- your limbs are immobilized for medical reasons;
- you are already familiar first-hand with the treatment of arthrosis or osteoarthritis of another joint;
- you have crossed a serious age limit.
Does your shoulder hurt? There are simple tests that allow you to independently determine, before visiting a doctor, which muscles, ligaments and joints of a limb or neck provoke pain:
Treatment of glenohumeral periarthritis
How to treat glenohumeral periarthritis? Conservative treatment of glenohumeral periarthritis begins with measures aimed at stopping the influence of provoking factors. First of all, limit the load on the affected joint. The patient is allowed movements that do not cause increased pain. In case of very severe pain, provide rest and immobilization of the affected limb for several hours a day (wearing the arm in a scarf). When pain decreases, physical therapy is prescribed. It is aimed at strengthening the muscles of the shoulder girdle, preventing future exacerbations. Gymnastics for glenohumeral periarthritis for the muscles of the shoulder girdle includes internal and external rotation, abduction.
Rehabilitation specialists use various methods of reflex therapy (physiotherapeutic procedures, acupuncture, segmental acupressure). The severity of pain is reduced by the use of electrophoresis of 0.5% or 2% novocaine solution. Sinusoidal simulated currents, including SMT phoresis of drugs, have a good therapeutic effect in scapulohumeral periarthritis. Subsequently, patients undergo mud applications and general sulfide baths. Good results are described with the combined use of ultrasound (US) therapy and SMT. For pain in the shoulder girdle, the following physiotherapeutic procedures are used in combination:
- Decimeter waves;
- Electrical stimulation;
- Electrophoresis of medicinal substances;
- Magnetotherapy.
Good results are achieved by combining microwave therapy with interference currents.
Drug treatment for glenohumeral periarthritis is aimed at reducing the severity of pain and tissue swelling, relieving muscle spasm and increasing the functional state of the shoulder joint. The degeneration process is affected with the help of chondroprotectors. To relieve pain, local blockade of trigger and painful points is performed with a 1–2% lidocaine solution or a 0.5%–2% procaine solution. Hydrocortisone and vitamin B12 are added to the local anesthetic solution. For lesions located near the shoulder joint, local treatment with glucocorticosteroids is performed.
Simple analgesics (paracetamol), non-steroidal anti-inflammatory drugs and muscle relaxants are widely used to reduce and relieve pain. In cases of severe pain, in some cases they resort to the use of narcotic analgesics - tramadol or a combination thereof.
In the complex treatment of glenohumeral periarthritis, pharmacological agents are used that stimulate the production of components of connective and cartilaginous tissue (including spinal structures), slow down their destruction, and thereby prevent the progression of degenerative changes. These include chondroitin sulfate and glucosamine.
Postisometric relaxation
As a complement to all treatment methods, we recommend post-isometric relaxation (PIR). Doctors note that relaxation helps 9 out of 10 patients with glenohumeral periarthritis.
The essence of the method is as follows:
- With the help of special movements, the maximum possible tension in the shoulder muscles is achieved in the patient’s condition.
- Muscle tension is maintained at maximum for 7–10 seconds.
- After which the muscles relax as much as possible - the relaxation phase.
Postisometric relaxation is aimed at relieving muscle spasm in the sore shoulder. This allows you to reduce pain and restore almost full mobility to the joint.
Exercise therapy for glenohumeral periarthritis
At the initial stage of treatment of glenohumeral periarthritis, patients do the following exercises from the starting position “lying”:
- They clench and unclench their fingers, shake the brush;
- Bend your arms at the wrist joint;
- Holding your arms along your body, turn your palms down and up;
- Keep your arms along the body, while inhaling, bring your hands to your shoulders, and while exhaling, lower them.
You can bend your elbows and spread your forearms to the sides, bringing the back of your hand as close as possible to the horizontal surface. The hands should be kept on the shoulders, the elbows in front of you, as you inhale, spread the elbows to the sides, and as you exhale, place them vertically again.
The following exercises for shoulder osteoarthritis are done while sitting:
- Place your hands on your waist, spread your elbows to the side and bring them towards each other at low speed;
- Hands are located at the waist, simultaneously rotate both shoulders forward and backward;
- As you inhale, bend your elbows, and as you exhale, lightly swing them back and forth;
- Place your hand behind your back and raise your palm to your shoulder blade.
Rehabilitation specialists at the Yusupov Hospital select an individual set of exercises for each patient for glenohumeral periarthritis. These exercises are suitable for treating the disease at home.
Massage for glenohumeral periarthritis
Massage for glenohumeral periarthritis is an important component of the treatment course and recovery process. Massage is combined with drug treatment, which will ensure a faster recovery. The method is aimed at preventing a decrease in joint activity and the development of rough scar tissue. muscle atrophy. It allows you to quickly restore the function of the upper limbs. In the acute phase of the disease, massage is not used.
With the help of massage, the collar area, glenohumeral joint and shoulder, deltoid and pectoralis major muscles are affected. Manual therapy is carried out only after acute inflammation in the joint capsule has been relieved and pain has been reduced. The procedures are carried out 14–20 days after immobilization of the joint. This allows you to obtain a pronounced therapeutic effect. Complete a course of effective treatment for glenohumeral periarthritis by making an appointment with a doctor by calling the contact center of the Yusupov Hospital.
Conducting physical therapy
In order for a speedy recovery to occur, you should use therapeutic exercises. A big plus is doing exercises in water. Swimming and hydrokinesotherapy are an integral part of the recommended complex during glenohumeral periarthritis. Exercising in the pool normalizes muscle tone, relieves excess tension, and increases the mobility of the damaged joint.
If we talk about the goals of the gymnastics complex, we can highlight:
- Blood flow is normalized.
- Tissues are enriched with oxygen.
- Stagnation is eliminated.
- Muscles are strengthened.
- Metabolic processes are normalized.
It should be remembered that physical therapy is contraindicated if glenohumeral periarthritis is in the acute stage or if there is severe pain in the joint.