Causes of shoulder arthritis Symptoms of shoulder arthritis Treatment of shoulder arthritis Drugs for the treatment of shoulder arthritis
The shoulder joint is the most mobile joint in the human body. Anatomically it is designed for multi-axis rotation. In addition, along with the hip and knee joints, it is considered one of the largest.
High mobility and load make this joint vulnerable to arthritis of the shoulder joint, an inflammatory disease that develops in the soft tissues and joint capsule. What are the symptoms and treatment of shoulder arthritis?
Arthritis of the shoulder joint imposes a lot of restrictions on the usual way of life
Causes of Shoulder Arthritis
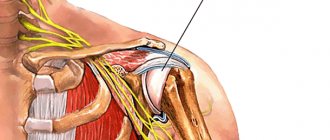
Arthritis of the shoulder joint is characterized by inflammation that begins with soft tissues (muscles, tendons, ligaments), moves to cartilage, and then affects the bone. First, the disease disrupts blood circulation, which provokes a lack of nutrition and rapid wear of the cartilage. After this, dystrophy of the muscular-ligamentous apparatus begins with further microdamage to the bone heads and joint deformation. Symptoms of shoulder arthritis can be caused by:
- Injuries and increased stress on the joint. Intense wear and tear due to repetitive motion (for example, weightlifters, tennis players, packers, overweight people), bruises, sprains and other injuries often provoke inflammation in the tissues. Often inflammation begins due to stress on “not warmed up” muscles - for example, during exercise in the gym after insufficient warm-up. In the early stages, post-traumatic arthritis of the shoulder joint is highly treatable.
- Hereditary predisposition and individual anatomical features of the shoulder joint capsule. Weak ligaments, insufficient collagen synthesis and other genetic characteristics can lead to frequent injuries. Minor but regular, they contribute to the development of arthritis.
- Infectious diseases (including chronic ones, such as caries). Some specific and nonspecific (purulent) infections can enter directly into the joint capsule, destroying cells, and can cause reactive arthritis. Most often, arthritis of the shoulder joint is provoked by urogenital and intestinal infections (chlamydia, mycoplasmosis, salmonellosis, dysentery).
- Autoimmune diseases and allergic reactions. With rheumatoid arthritis of the shoulder joint, systemic lupus erythematosus and a number of other diseases, the patient’s body begins to attack its own tissues using the so-called. killer cells. This causes chronic inflammation in the joint and periarticular tissues.
- Lack of physical activity and poor posture. Both factors lead to the fact that the load is not distributed between the joints and the muscular corset (as is normal), but falls entirely on the joint. A sedentary lifestyle also leads to stagnation of synovial fluid - it ceases to nourish the joint and eliminate waste products from it.
- An unbalanced diet (primarily a deficiency of vitamin C, zinc, calcium, selenium, omega acids), as well as an excess of salts and carbohydrates, leads to joint destruction and tissue damage.
- Age-related and hormonal changes. Natural wear and tear of cartilage tissue or endocrine disorders lead to changes in the properties of cartilage - its elasticity, shock-absorbing properties, and ability to regenerate.
- Metabolic disorders. Diseases such as type 1 diabetes or gout, which are associated with abnormalities in metabolism, often manifest themselves in the joints.
- Hypothermia and other stress (including psycho-emotional or chronic due to bad habits). These conditions lead to disruption of normal metabolism and a weakened immune system. In such a situation, cartilage tissue is one of the first to suffer - because it is deprived of blood supply. This means that it does not receive enough nutrition and accumulates breakdown products in stressful situations.
General information about the disease
Arthritis of the shoulder joint is an inflammatory disease that can be of a primary local nature (acute purulent arthritis) or be associated with some general infectious or non-infectious disease. Codes for the International Classification of Diseases, 10th revision (ICD-10) M00 – M25. The code is specified after the type and clinical form of the disease has been established.
The joint is formed by the round head of the humerus and the smaller glenoid fossa of the scapula, held in place by the surrounding soft tissue. It is the most mobile and the most loaded in the human body, so it is often injured and then inflamed.
Its peculiarity is the frequent development, along with arthritis, of lesions of the soft tissues adjacent to the joint - periarthritis.
Any clinical form of the disease requires active treatment and subsequent rehabilitation. If this is not done, the pathological process will progress and lead to gradual destruction of the shoulder joint, loss of function and disability.
Symptoms of shoulder arthritis
Characteristic signs of arthritis in the shoulder joint are:
- Frequent or constant pain. Pain syndrome can be expressed in dull pulling and aching sensations, acute “lumbago”, and aching. For example, infectious arthritis manifests itself with sharp pain, while psoriatic arthritis is dull. Degenerative-dystrophic (arthrosis-arthritis) can occur almost imperceptibly for the patient, without pronounced discomfort - especially in the presence of cardiovascular diseases or suppression of cognitive abilities. The pain can be localized in the shoulder area, in the front part (the acromioclavicular joint is affected) or radiate to the neck behind the shoulder, the shoulder blade (the scapulothoracic joint is affected).
- Impaired joint mobility. In the initial stages, it is caused by increasing swelling due to the accumulation of synovial fluid in the joint capsule. Later, the restrictions become permanent due to joint deformation. At first, the reduction in mobility is insignificant - for example, it is difficult for the patient to clasp his hands behind his back (during the test, one elbow should be directed up, the other down) or raise his forearms above his head, perform the “mill” exercise, or get something from the top shelves. However, over time, the patient can no longer hold onto the overhead rail on public transport or take off a sweater without severe pain. Stiffness and stiffness are especially noticeable in the morning - after waking up, the patient needs a warm-up to return to normal.
- Specific crunch - so-called. crepitus. It is very simple to distinguish an “arthritis” crunch from a healthy one, caused by the collapse of gas bubbles in the joint. If you hear a suspicious crunch during a sudden voluntary movement, immediately repeat it - if the crunch is heard again and again, then it is better to contact a rheumatologist. If crepitus is accompanied by a feeling of “tension” or uncomfortable resistance in the joint, this reliably indicates an inflammatory process.
- Swelling, local increase in temperature over the affected joint, redness of the skin. This symptomatology corresponds to local inflammation - the skin over the joint may be painful to touch, as with a sunburn.
- Systemic manifestations - such as an increase in general body temperature, chills, weakness, dizziness, nausea, loss of appetite and endurance (sharp - with reactive arthritis and gradual - with rheumatoid arthritis).
Over time, the joint may increase in size and eventually become deformed. In this case, dystrophy of the adjacent muscles is observed. In some cases, patients complain of numbness in the shoulder or arm (when swelling disrupts the healthy innervation of the limb).
Signs of arthritis of the shoulder joint intensify after a long stay in the same position (sleep, office work), monotonous physical work, or when the weather changes. The rest of the time, chronic arthritis may not make itself felt - until the late stages, when patients have disturbed sleep, and pain occurs with any movement of the hand.
What is shoulder arthrosis
Arthrosis of the shoulder joint is a chronic disease. It is accompanied by damage to cartilage tissue, the formation of osteophytes, and against this background, joint mobility is limited. Most often, this pathology is diagnosed in elderly people. Heavy physical activity and various inflammatory processes can also provoke its development. If there is no timely treatment, movement in the joint is completely blocked.
Cartilage tissue is the smooth layer between the bones that touch. With the help of cartilaginous structures, bones slide easily between each other. This ensures full, free and painless function of the joint.
With excessive loads, inflammation or injury, degenerative processes are triggered. Gradually they begin to spread over the entire articular surface. Against this background, a violation of the smoothness of the surface of the joint occurs. Any movement becomes painful, the intensity of pain increases as the disease progresses.
At the same time, growths called osteophytes form on the edges of the articular surfaces. They begin to replace the damaged cartilage. Gradually, not only bone structures, but also healthy tissues begin to be involved in degenerative processes. Deformation of the limb occurs, spasm occurs in the muscular system, ligamentous structures weaken and become less elastic. If there is no timely treatment, joint mobility is impaired.
Stages of shoulder arthritis
Regardless of the cause, experts distinguish 4 stages of arthritis of the shoulder joint:
Arthritis of the shoulder joint 1st degree
Most of the time there is no pain and occurs when the weather changes or the load on the joint. In the morning, the patient experiences some discomfort when trying to raise his arm or perform daily activities. The muscles begin to weaken, so your arms get tired faster than before. Otherwise, degree 1 arthritis of the shoulder joint is practically asymptomatic - but it is at this stage that it can be completely cured or slowed down, maintaining the mobility of the arms until old age.
Arthritis of the shoulder joint grade 2
The feeling of stiffness and deterioration in mobility become pronounced. Crepitation and unpleasant clicking sounds appear. At this stage, the cartilage begins to thin out, and focal erosions appear on the heads of the bones. Because of this, the patient experiences pain when trying to raise his arm or feel his shoulder, and tries to take care of the limb. Often it is at the 2nd stage that noticeable swelling and fever appear. Subluxations are possible due to weakening of muscles and ligaments. Discomfort does not disappear even with reduced loads - at this stage, patients most often seek treatment for symptoms of arthritis of the shoulder joint.
Arthritis of the shoulder joint grade 3
The disease affects the deeper structures of the joint and deforms it. Daily household activities are accompanied by acute pain, which prevents the patient from taking care of himself. Changes in the joint are already irreversible, but treatment of arthritis of the shoulder joint still allows the patient to maintain a satisfactory quality of life.
Arthritis of the shoulder joint grade 4
The hands are almost completely immobilized, and standard treatment does not help. The pain does not disappear completely even when taking analgesics. At this stage, patients often experience psycho-emotional disorders caused by depression and insomnia.
Complications and prognosis
The consequences of arthrosis of the shoulder joint can be:
- limitation of mobility, development of ankylosis, when the bones fuse together;
- intense pain that does not go away with rest;
- severe deformation of the shoulder joint and the entire limb.
Such consequences arise if there is no treatment for arthrosis or if the diagnosis is incorrect.
You should not ignore the symptoms of arthrosis. It is important to see a doctor as early as possible, who will help make the correct diagnosis and prescribe the correct treatment regimen. You should also strictly follow the doctor’s instructions, undergo medication treatment, and perform physical therapy. It is important to adhere to proper nutrition and visit a specialist at the slightest change in condition.
Treatment of shoulder arthritis
When treating arthritis of the shoulder joint with medications, a gentle regimen is recommended (for example, wearing the arm in a special bandage that is attached to the neck and healthy shoulder).
Please note: rheumatologists do not recommend abusing simple analgesics, as this gives the patient and the attending physician a wrong idea about the course of the disease.
Treatment of shoulder arthritis requires constant and systematic treatment
Physiotherapy for shoulder arthritis
For arthritis of the shoulder joint, the following procedures are recommended:
- amplipulse (SMT)
- laser therapy;
- magnetic therapy;
- balneotherapy;
- exercise therapy;
- manual therapy;
- special therapeutic massage for arthritis of the shoulder joint;
- cryotherapy;
- mechanotherapy;
- UHF;
- electrophoresis;
- electromyostimulation;
- acupuncture.
All these techniques help consolidate the effect of medications for arthritis of the shoulder joint, prolong drug-free remission, and promote better nutrition and cartilage regeneration.
Massage for arthritis of the shoulder joint
Massage for arthritis is prescribed by a doctor - only after acute tissue inflammation has been eliminated. Rehabilitation must be carried out by a specialist. Massage helps:
- reduce pain and spastic muscle tension;
- restore blood circulation, tissue nutrition and elasticity of ligaments;
- improve movement in the shoulder joint;
- eliminate muscle atrophy;
- Non-surgically remove a small amount of effusion from the joint.
Please note: in the acute phase of the disease, especially with infectious or post-traumatic arthritis, massage can be extremely dangerous!
Massage for arthritis of the shoulder joint helps reduce pain
Exercise therapy: exercises for arthritis of the shoulder joint
For arthritis of the shoulder joint, smooth passive movements are recommended (performed only in the absence of pain):
- swinging your arms (exercises like “pendulum”);
- exercises on the sore arm with support from the healthy arm;
- exercises with equipment (ball, gymnastic stick).
We offer a “home” set of exercises for arthritis of the shoulder joint:
- Sit up straight and place your palms on your waist. Bring your elbows in and out in front of you as much as possible.
- Sit up straight, lower your arms freely. Raise and lower both shoulders at the same time. Then repeat the exercise on each side in turn.
- Sit upright and make circular movements with your shoulders, first forward, then back.
- Stand with your feet shoulder-width apart. Spread your arms to the sides (cross pose). Raise both arms above your head and lower them, returning to the starting position.
- Stand up straight. Squeeze your shoulder blades together as much as possible.
Gymnastics should be performed daily, 2-3 times a day. It is advisable to consult with a physical therapy instructor: each rehabilitation stage has its own tasks, exercises and loads on the shoulder joint.
General clinical recommendations
For patients suffering from shoulder arthritis, it is recommended to:
- eat properly regularly, giving preference to low-fat animal products and vegetable and dairy foods;
- do not load the shoulder with increased physical activity, especially heavy lifting;
- regularly engage in exercise therapy: perform at home a complex of therapeutic exercises prescribed by the attending physician;
- do not overcool;
- get rid of bad habits - smoking and alcohol abuse - they disrupt blood circulation and metabolic processes;
- promptly treat all acute and chronic diseases, hormonal disorders;
- carry out maintenance treatment regularly.
We combine proven techniques of the East and innovative methods of Western medicine.
Read more about our unique method of treating arthritis
Drugs for the treatment of shoulder arthritis
In the treatment of arthritis of the shoulder joint with medications, drugs are used to relieve inflammation, eliminate infectious pathogens (there are some), dilate blood vessels and stimulate the growth of cartilage cells.
Drugs are the main remedy for pain in shoulder arthritis
Chondroprotectors
Preparations based on chondroitin and glucosamine in the form of sulfates are taken to prevent the disease, as well as at all stages except the last. These are: artracam, arthra, teraflex, collagen ultra, osteovit, osteomed, protecon, artron, alflutop and others.
Antispasmodics and muscle relaxants
Constant muscle tension can interfere with a patient's daily life, leading to pain and limiting mobility. In these cases, ketorol, baralgin, mydocalm, and papaverine are prescribed.
Nonsteroidal anti-inflammatory drugs (NSAIDs)
NSAIDs can be used both externally (in the form of ointments and gels - finalgel, ketonal, fastum, dolobene) and in the form of injections or tablets for the treatment of arthritis of the shoulder joint. These are: naproxen, indomethacin, xefocam, diclofenac, nurofen, ibuprofen, ketanov, celecoxib. It is recommended to combine them with warming ointments for arthritis of the shoulder joint - for example, with camphor oil, bee or snake venom (in the absence of allergies).
Steroid drugs
Steroid drugs with cortisol - glucocorticoids - are used for severe pain if NSAIDs are ineffective. Thus, short courses are prescribed: hydrocortisone, diprospan, triamcinolone, dexamethasone, prednisolone, kenalog.
Antibiotics
How to treat arthritis of the shoulder joint caused by infection is decided by the doctor based on professional experience or an antibiogram. For septic arthritis, cephalosporins, macrolides, and penicillins are used to eliminate purulent infections. For specific infections (for example, tuberculosis), specialized drugs are used as prescribed by a doctor.
Side effects
Side effects of Movalis - Headache
As with therapy with other NSAIDs, while taking Movalis, there is a possibility of adverse reactions from the body:
- From the urinary system: edema, hypercreatininemia, increased urea concentration. In rare cases - interstitial nephritis, glomerulonephritis, renal medullary necrosis, nephrotic syndrome.
- From the digestive system: nausea, vomiting, belching, abdominal pain, constipation or diarrhea, flatulence, increased activity of “liver” transaminases, hyperbilirubinemia, stomatitis, erosive and ulcerative lesions of the gastrointestinal tract, gastrointestinal bleeding (hidden or obvious), perforation of the digestive tract canal, colitis, dyspepsia, gastroduodenal ulcer, esophagitis, gastritis, hepatitis.
- From the cardiovascular system: increased blood pressure, “flushes” of blood to the skin of the face and upper chest, palpitations.
- From the nervous system: dizziness, headache, drowsiness, mood lability, confusion, disorientation..
- From the hematopoietic organs: anemia, leukopenia, thrombocytopenia.
- Allergic reactions: skin rash, itching, blisters, erythema multiforme, Lyell's syndrome, bullous dermatitis, Stevens-Johnson syndrome, angioedema, hypersensitivity to UV radiation, urticaria, anaphylactoid reactions.
- Other: ringing in the ears, blurred vision, conjunctivitis.
The combined use of Movalis and drugs that suppress the functioning of the bone marrow can provoke cytopenia (deficiency of one or more types of blood cells). If gastrointestinal bleeding, perforation or ulcer occurs during therapy with Moralist, this can lead to death.
In the case of using a d/i solution, the following are also possible:
- glomerular or interstitial nephritis;
- papillary necrosis;
- nephrotic syndrome;
- swelling and pain at the injection site.
Analogues of Movalis
Analogues of Movalis on the pharmaceutical market are the following drugs: Mirlox, Artrosan, Melox, Meloxicam, Mataren.
As for Movalis injections, the doctor can replace them with medications containing the same active ingredient: Amelotex, Arthrozan, Meloxicam, Melbek, Liberum, Bi-xicam, Movasin, Mesipol.
Analogues of the drug Movalis
Movalis/Meloxicam
The drugs are based on the same active substance, so their therapeutic effect is identical. The only difference is the price.
Movalis/Voltaren
The active substance of Voltaren is diclofenac. Frequent development of side effects is noted. Unlike Voltaren, Movalis has a positive effect on cartilage metabolism. Therefore, both drugs are effective for pain relief, but for osteoarthritis, Movalis is better.
Movalis/Nise
The active substance of Nise is nimesulide. Both drugs are characterized by effectiveness in treating heat, inflammation and pain.
But nimesulide is toxic to the liver, but Movalis is not and does not have a similar effect.
Movalis relieves pain more slowly, but its effect is prolonged, while Nise is good for quickly relieving pain.
Injections with Movalis: instructions for use
Movalis in ampoules is used exclusively intramuscularly (intravenous use is prohibited). The medicine is administered once in a dose of 15 mg. Typically, injections with Movalis are used in the first 2-3 days of therapy.
The medicine is administered slowly, by deep injection into the gluteus maximus muscle.
The recommended daily dose is 7.5 mg or 15 mg 1 time/day, depending on the intensity of pain and the severity of the inflammatory process.
- Osteoarthritis with pain: 7.5 mg/day. If necessary, the dose can be increased to 15 mg/day;
- Rheumatoid arthritis: 15 mg/day. Depending on the therapeutic effect, the dose can be reduced to 7.5 mg/day;
- Ankylosing spondylitis: 15 mg/day. Depending on the therapeutic effect, the dose can be reduced to 7.5 mg/day.
Movalis suppositories: instructions for use
For adults with osteoarthritis, rheumatoid arthritis or spondylitis, rectal suppositories are administered at a dose of 7.5 mg 1 time / day. If indicated, the dose can be increased to the maximum possible per day - 15 mg.