De Quervain's disease (Stenosing ligamentitis, Stenosing tenosynovitis, Chronic tenosynovitis)
The examination must be carried out in comparison of both hands - this makes it possible to accurately identify changes in the affected hand that are sometimes not too pronounced, but absolutely characteristic of de Quervain’s disease. In the area of the wrist joint on the side of the first finger, slight or moderate local swelling is determined. The anatomical snuffbox is smoothed or not visible due to swelling. The skin over the affected area is not changed, there is no local increase in temperature. Rare cases of peeling, redness and local hyperthermia are not caused by the disease itself, but by self-treatment, which patients sometimes carry out before seeing a doctor.
Palpation reveals pain in the affected area, reaching a maximum in the projection of the styloid process of the radius. Pressing on the area of the tendons of the first finger is painless. Just below the styloid process, a dense and smooth rounded formation is felt - the dorsal ligament, thickened in the canal area. After examining the affected area, the patient is asked to place his hands palms down and tilt the hands alternately towards the little finger and thumb. The patient's hands deviate almost equally towards the first finger. When deviating towards the little finger, movement is limited by 20-30 degrees compared to a healthy hand, and movement is accompanied by severe pain.
In addition, the limitation of thumb abduction is determined on the affected hand. To identify the symptom, the patient is asked to place his hands on the edge with palms facing each other. During movements, a significant limitation of abduction is noticeable (the difference between the diseased and healthy side is from 40 to 80 degrees). The difference when extending the first fingers is not so striking, but is also visible to the naked eye.
Another test to confirm the diagnosis is the Finkelstein test. The patient presses the thumb to the palm and squeezes it tightly with the other fingers, and then moves the hand towards the little finger. Movement is accompanied by sharp pain in the affected area. Also, with this disease, a violation of the ability to hold objects with the first finger is detected. The patient is asked to simultaneously take some objects (for example, pens or matchboxes) with the first and second fingers of both hands. When pulling on an object, pain and weakness are detected when holding on the affected side. The diagnosis of de Quervain's disease is made on the basis of clinical data. No additional research is required.
Predisposing factors
- Injury to the styloid process (acute or chronic)
- Occupational factors: de Quervain's disease most often affects people whose main workload is on their fingers (gardeners, musicians, tennis players, artists, sculptors, etc.)
- Anatomical factors: a narrow canal in which the tendon of the first finger passes.
- Diseases: rheumatoid arthritis.
Women are more susceptible to the disease than men.
If you have any questions, ask our specialist! Ask a Question
Preparation for surgery:
- Bleeding: The operation is performed on a hand that has been bled dry to ensure optimal visibility conditions and limit the risk of damage to important structures (nerves, blood vessels, tendons). The operated arm is wrapped in a rubber bandage and the shoulder is pressed with a pressure cuff during the operation.
- Disinfection of the skin and covering with a sterile cloth: To avoid infection, the skin is disinfected and the surgical site is covered with a sterile cloth.
- Magnifying glasses: The operation is performed using magnifying glasses, which help to clearly distinguish and thereby protect the important functional structures of the hand.
Healing process after surgery
Pain after surgery is usually minimal and most patients do not require painkillers.
Typical pain symptoms disappear after surgery, and the radiating pain goes away after a few days. In rare cases, friction is felt in the tendons, which completely disappears after a few weeks. Negative sensations in the postoperative scar largely disappear after the first 6-8 weeks; after 3-6 months, patients no longer complain of pain in the scar. However, only after 12 months can we say that the scar has completely healed. © Dr. Klaus Lovka
to the top of the page
Sequence of the operation:
- Skin incision (Fig. 4)
- Preparation of the superficial sensory branch of the radial nerve
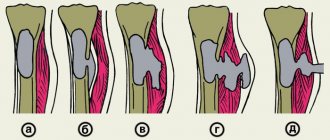
- Preparation of the 1st canal of the dorsal carpal ligament
- Dissection of the 1st canal of the dorsal carpal ligament and removal of the edges on both sides (Fig. 5))
- If necessary, incision in the canal of the septum between the APL and EPB tendons
- If necessary, removal of synovial tissue altered by inflammation
- Pulling both tendons, eliminating their possible adhesion to each other
- Tendons slide freely in the canal
- Ultimate control of the integrity of superficial nerve branches
- Closing the incision with a suture
- Sterile pressure dressing
Postoperative treatment
- After the operation, the patient returns home, his fingers and especially the thumb and wrist should remain in motion, but not overworked.
- 5-7th day after surgery: first change of bandage (can be performed by a family doctor).
- 14th day after surgery: change of bandage and removal of stitches (can be performed by a family doctor).
- One day after the stitches are removed, the bandage is no longer needed. Start regular (3-4 times a day) exercises in cold water (add ice if necessary). Cold relieves swelling and pain. Patients who cannot tolerate cold take warm water.
- Five days after the sutures are removed, treatment of the postoperative scar begins. Calendula ointment (or other fatty ointments) is rubbed into the scar 4-5 times a day, it softens, becomes elastic, less painful and sensitive. Patting the scar, for example with a soft brush, also helps.
- Therapeutic exercises and/or occupational therapy are rarely required, but are prescribed immediately if movement difficulties occur.
- The duration of the patient's disability is usually 2-3 weeks.
Why does my hand hurt with tendinitis?
The fact is that the muscles that work on the hand are mostly quite long and begin on the forearm just below the elbow. The contractile part of the muscle (belly) is located on the forearm, and the tendon (a thin cord connecting the muscle to the bone) passes past the wrist in special osteo-fibrous canals. There are six of them for the extensor muscles. The wrist that is most susceptible to tendinitis is the first one, which contains the abductor pollicis longus and extensor pollicis brevis muscles. With excessive load, chronic inflammation occurs and the channel becomes tight for the tendon to slide freely, which causes pain.
Symptoms
In the vast majority of cases, the disease progresses slowly. The main symptom of de Quervain's disease is pain along the inflamed tendon. The pain usually starts at the base of the thumb and spreads up the arm to the elbow, shoulder, and in severe cases to the neck. The pain is often aching in nature, intensifying with movement, so many patients try to “protect” this hand, bandage the wrist, or wear wristbands. You may also notice some swelling on that side of the wrist. Movements of the wrist are painful, it is impossible to clench your hand into a fist, movements of the thumb are painful. Hand strength may be significantly reduced.
Diagnosis of thyroiditis
- When collecting an anamnesis of the disease, an episode of acute respiratory viral infection is noted approximately 20-30 days before the onset of the disease.
- During an objective examination, palpation of the thyroid gland is difficult, since the patient has severe pain. The gland is dense and painful.
- Symptoms of thyrotoxicosis are noted in both physical and emotional aspects (sweating, rapid heartbeat, irritability).
- According to laboratory tests, a typical manifestation of subacute thyroiditis is a significant increase in the level of ESR (up to 50-70 mm/l) in the CBC with a normal level of leukocytes, but moderate lymphocytosis. An elevated ESR level has its diagnostic value only at the onset of the disease.
- An important indicator of the destructive process that develops in the thyroid tissues is an increase in the level of C-reactive protein.
- In the initial stages (acute, thyrotoxic), there is a transient increase in the level of T3-free and T4-free against the background of a reduced level of TSH. In order to exclude hypothyroidism, the TSH concentration is re-determined after a month, then after six months.
- Carrying out a radioisotope research method - reducing the uptake of 99mTc.
- Ultrasound of the thyroid gland reveals unclear and limited hypoechoic areas.
- An important diagnostic criterion is the rapid effect of glucocorticoid therapy (Kreil test).
What about pain in your thumb?
In acute conditions, when symptoms of inflammation and acute pain appear, it is recommended to avoid manual actions that cause pain. Cold compresses relieve pain in the thumb. They are used to reduce swelling.
It is recommended to wear a soft orthosis on the thumb to stabilize and relieve the affected tendon and wrist joint, immobilization should cover the forearm and wrist and reach the heads of the 2-5 metacarpal bones, it is advisable to use the orthosis throughout the entire period of manifestation of symptoms of tenosynovitis, i.e. at least 2 - 3 weeks. .
Pharmacotherapy includes the use of non-steroidal anti-inflammatory drugs, analgesics, vitamin B 6 and corticosteroids generally or locally by injection into the tendons or iontophoresis, that is, using direct current.