Extreme conditions (from the Latin extrema - excessive, extreme, extreme, limit) are usually called severe conditions of the body that arise when it is exposed to particularly pathogenic external factors or the unfavorable development of existing diseases, causing gross disturbances of metabolism and vital functions that pose a threat to life. and requiring urgent active therapeutic intervention.
The concept of “extreme states” should not be confused with the concept of “terminal states”. The main distinguishing feature of terminal conditions is their irreversibility without special emergency medical measures, while many forms of extreme conditions can be independently reversible. Even in cases of an unfavorable outcome during the development of extreme conditions, as a rule, a more or less long period of improvement in the body’s condition is noted - due to the inclusion of numerous compensatory and adaptive mechanisms. Terminal conditions are characterized by progressive depression of functions and extinction of life. Extreme conditions include shock, collapse, coma.
Clinical death: short-term reversible condition
The following signs cause medical staff to sound the alarm:
- loss of consciousness – indicates bleeding of the brain;
- cessation of breathing movements - indicates a lack of oxygen flow into the body;
- cessation of pulse indicates inactivity of the heart muscle.
Secondary symptoms may also include:
- lack of reaction of the pupils to light - this also happens with a powerful electric shock;
- lack of reflex blinking - this happens with temporary paralysis;
- pallor of the skin - this happens with frostbite of the extremities.
First of all, the actions of resuscitators are reduced to restoring breathing and blood flow. And the sooner the heart muscle begins to function again, and the lungs supply oxygen to the internal organs, the greater the chance of reviving the patient. Within five minutes, individual brain cells may die. However, during clinical death, the body can turn on its protective functions and enter hyperboric oxygenation. In this state, the available oxygen is slowly consumed, making a return to normal life possible within 10-20 minutes. Slow metabolism can be caused by hypothermia, electric shock, drowning and a number of other reasons.
Visions during clinical death
Ambulance workers and resuscitators deal with patients on the brink of death all the time. Most often, they are brought to life in a brightly lit room. It is the light of the spotlights that hits the eyes with tunnel vision that many patients interpret as “the light at the end of the tunnel.” The silhouettes of doctors trying to bring the dying back to life are perceived as visions from the Kingdom of the Dead, that is, as their deceased relatives. False memories are superimposed on the natural feeling of flight during cerebral ischemia. Together with the influence of medications, chemical reactions occurring inside the body give rise to serious distortion of sensory perceptions. These memories are then interpreted as contacts with the World of Souls.
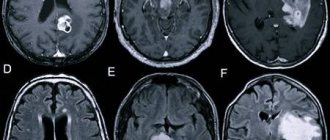
Pathogenesis
After clinical death occurs, tissue metabolism slows down sharply, but due to anaerobic glycolysis it does not stop completely. When breathing stops and blood flow stops, destruction processes begin very quickly in the body. Due to oxygen starvation, tissues are destroyed. In this case, the cells of the cerebral cortex experience the greatest sensitivity. As a result, when brain cells die, even after successful resuscitation, complete recovery does not occur.
When blood flow stops in the body, active blood clotting occurs, and microthrombi appear in the vessels. Due to toxic products of tissue breakdown entering the blood, metabolic acidosis . With prolonged absence of blood circulation, biological death occurs. In the case of urgent resuscitation, cardiac activity is restored, after which postresuscitation disease as a consequence of ischemia , thrombosis of the capillary network, and significant homeostatic changes.
The duration of the period of clinical death is determined by the period during which the cerebral cortex and subcortex can maintain viability under hypoxic . For 3-5 minutes, the higher parts of the brain can remain viable in the absence of oxygen supply under conditions of normal body temperature. The practice of doctors in all countries of the world indicates that if the specified period is exceeded, then the person can return to life, but in this case the phenomenon of decortication (death of the cerebral cortex) or decerebration (all parts of the brain die) is already noted.
However, in medicine there is a second period of clinical death, which can last longer, after which resuscitation measures allow the person to be revived. This is achieved by the fact that the processes of degeneration of parts of the brain due to hypoxia are slowed down due to the creation of certain conditions. Thus, it is possible to increase the duration of clinical death in a state of hypothermia , that is, artificial cooling of the body. This can also be done by physical influences - hyperbaric oxygenation , head hypothermia . Special pharmacological drugs are also used to ensure a sharp decrease in metabolic processes.
In the absence of resuscitation processes or the failure of such actions, biological death occurs, and all physiological processes in the body cease.
Biological death: irreversible death of cells, tissues, organs
One of the first signs of biological death is the drying of the cornea. It is determined by squeezing the eye from the sides - the pupil then takes the shape of a spindle or “cat’s” eye. It is known to doctors as Beloglazov’s symptom.
Next, the patient begins to exhibit the following symptoms:
- the mucous membranes of the nose, mouth, and genitals dry out;
- body temperature gradually decreases;
- characteristic cadaveric spots appear on the skin;
- rigor mortis is noticeable.
Although decomposition processes begin almost immediately, some organs are less susceptible to it. Thus, the heart can be implanted 1-2 hours after removal from a dead body, and the kidneys and liver can be preserved for about 4 hours. Skin transplantation from a deceased person to a living person can be performed within the first 6 hours. Bone tissue is considered the most resistant - due to its inertness to external factors, it can be implanted into the recipient within 1-2 days.
General information
Clinical death is a transition period between life and biological death of a person.
At its core, it is a reversible stage of death, when the activity of the heart and breathing stops, and no signs of vital activity are observed. Characteristic signs of this condition are the absence of pulse and consciousness, dilated pupils. An objective sign is small-wave atrial fibrillation or isoline on the ECG. However, in this condition, oxygen starvation does not lead to the development of irreversible changes in systems and organs. The ICD-10 code for this condition is G93 (Other brain lesions). Speaking about how long clinical death lasts, it should be noted that the duration of clinical death is no more than 3-4 minutes. The maximum time during which the body can remain in such a terminal state is 5-6 minutes. In rare cases, a longer duration was recorded.
How to identify such a condition and properly provide first aid will be discussed in this article.
Is it possible to confuse clinical and biological death?
Despite numerous media reports about supposedly resurrected people, in reality this happens quite rarely. And in cases of “miraculous” revival, we should talk about the correct resuscitation techniques and the same hyperboric oxygenation that was mentioned earlier. “Resurrections” after a few days or even ten hours are more likely an acted out hoax than the real state of affairs. For it is impossible to prevent or reverse these processes from obvious tissue decay and other signs of decomposition.
Causes
This condition can be caused by a variety of factors - illness, injury. All causes are divided into two groups – those associated with damage to the heart muscle ( cardiac ) and those not associated with it ( non-cardiac ).
Cardiac causes include primary disorders of myocardial contractility, provoked by acute coronary pathology or the influence of toxic substances. Among such causes are acute myocardial infarction , arrhythmias , electrolyte imbalance, rupture of aortic aneurysm, coronary artery disease, etc.
Non-cardiac causes include conditions that accompany the development of severe hypoxia. This can be suffocation, drowning , acute respiratory failure, electric shock, embolism , poisoning, airway obstruction, etc. There is a risk of fibrillation and subsequent cardiac arrest if potassium preparations, cardiac glycosides, antiarrhythmics, barbiturates are administered incorrectly.
Agony
Agony begins with a sigh or a series of short sighs, then the frequency and amplitude of respiratory movements increase - as the brain's control centers are switched off, their functions move to redundant, less advanced brain structures. The body makes its last effort, mobilizing all available reserves, trying to cling to life. That is why, just before death, the correct heart rhythm is restored, blood flow is restored and a person can even regain consciousness, which has been repeatedly described in fiction and used in cinema. However, all these attempts do not have any energy support; the body burns the remnants of ATP, the universal carrier of energy, and completely destroys cellular reserves. The weight of the substances burned during agony is so great that the difference can be detected by weighing. It is these processes that explain the disappearance of those very few tens of grams that are considered the “flying away” soul. The agony is usually short-lived and ends with the cessation of cardiac, respiratory and brain activity. Clinical death occurs.
Symptoms
The main signs of clinical death of a person are as follows:
- Lack of breathing.
- Lack of effective heart contractions.
- Lack of consciousness.
If these symptoms are present at the same time, this is a clear sign of such a condition.
If the heartbeat or consciousness persists, clinical death is not diagnosed. Within 30 seconds after the blood flow stops, spontaneous residual breathing is possible. Individual myocardial contractions and, accordingly, weak pulse impulses may also be observed. As a rule, no more than 2-5 such shocks are detected.
Speaking about secondary signs of this condition, the following symptoms should be noted:
- Lack of muscle tone, movements, reflexes.
- Unnatural body position.
- Pale sallow skin.
- Inability to determine blood pressure .
- Pupil dilation up to 5 mm without reaction to light (observed after 90 seconds).
- Pointed facial features (the so-called Hippocratic mask).
Speaking about how clinical death differs from biological death, it should be noted that in case of clinical death there is the possibility of resuscitation.
Upon initial superficial examination, signs of clinical and biological death may be similar. However, the definition indicates that biological death is the irreversible cessation of all physiological processes, in contrast to clinical death.
Tests and diagnostics
Speaking about how this condition is diagnosed, first of all, it should be noted that diagnosis and treatment are carried out in parallel. After all, the less time passes between the establishment of such a fact and the start of resuscitation, the greater the likelihood that the person will live a full life subsequently.
This condition is determined by the symptoms described above. But if this happens in a medical institution, additional diagnostic methods are used. They are important in determining how effective methods of resuscitating a patient are. Also, physical and instrumental methods make it possible to assess the degree of hypoxia and acid-base imbalance. During the diagnostic process, measures are simultaneously taken to restore the heart rhythm.
The following types of research can be practiced:
- Physical methods . The examination makes it possible to detect characteristic symptoms. During auscultation, no coronary sounds are heard and there are no breath sounds in the lungs. Visually assess the presence of respiratory movements of the chest. Blood pressure is not determined.
- Instrumental methods . Electrocardiography is performed. It should be taken into account that the isoline corresponding to complete cardiac arrest is not determined in every case. Sometimes there is a random contraction of individual fibers, but there is no blood flow. There are no clear ventricular complexes.
- Laboratory methods . They are used if resuscitation is successful. Biochemical parameters, electrolyte balance, etc. are examined. Metabolic acidosis , high levels of potassium, sodium, proteins, and breakdown products are determined in the blood. Hypocoagulation and decreased concentrations of platelets and coagulation factors are noted.
Test with answers on the topic “Emergency care”
Test tasks on the topic “Emergency Care” were developed by teachers based on the National Standards of the Russian Federation “Technologies for performing simple medical services”, and are intended for self-preparation of students for certification testing. These test tasks are designed in such a way that you need to choose one correct answer out of five proposed ones.
900. Resuscitation is
1) the section of clinical medicine that studies terminal conditions; 2) department of a multidisciplinary hospital; 3) practical actions aimed at restoring the basic vital functions of the body; 4) actions of rescuers within 5 minutes after the incident; 5) specialization of the emergency medical team.
901. Advanced resuscitation measures can be carried out
1) only specialists from intensive care units; 2) specially trained medical workers; 3) the entire adult population; 4) police officers who arrived at the scene of the incident; 5) road service workers.
902. Resuscitation indicated
1) only in the event of sudden death of young people and children; 2) in case of any sudden cardiac arrest; 3) only if the patient has previously given consent; 4) if it is reliably known that more than 30 minutes have passed since cardiac arrest; 5) all of the above is true.
903. In the preagonal state, the pulse is determined:
1) only on large vessels; 2) only on peripheral vessels; 3) on large and peripheral vessels; 4) there is no correct answer; 5) all answers are correct.
904. Blood pressure (systolic) in the preagonal state
1) below 60 mmHg/st.; 2) below 80 mmHg/st.; 3) below 90 mmHg/st.; 4) below 120 mmHg/st.; 5) not determined.
905. In the preagonal state consciousness
1) lost; 2) saved; 3) partially lost; 4) partially preserved; 5) retrograde amnesia is observed.
906. Pupil reaction to light in the pregonal state
1) not changed; 2) weakened; 3) detected only in bright artificial light; 4) determined only in bright daylight; 5) not determined.
907. In the agonal state, the reaction of the pupil to light
1) weakened; 2) absent; 3) detected only in bright light; 4) not changed; 5) there is no correct answer.
908. In accordance with the algorithm, the provision of emergency assistance for hanging begins with
1) ensuring airway patency; 2) performing cardiopulmonary resuscitation; 3) release from the compressive loop; 4) blood pressure measurements; 5) delivering a precordial blow.
909. Specify the symptoms of clinical death
1) absence of pulse in the radial artery, lack of consciousness, rare breathing; 2) lack of consciousness, lack of breathing, lack of pulse in the carotid artery; 3) preservation of the pupillary reflex, weakening of the pulse in the carotid artery; 4) lack of consciousness, absence of pupillary reflex, preservation of the pulse in the carotid artery; 5) lack of breathing, lack of pulse on the radial artery, weakening of the pupillary reflex.
910. Indicate a reliable sign of biological death
1) lack of consciousness; 2) lack of breathing; 3) absence of heartbeat; 4) lack of pupil reaction to light; 5) rigor mortis.
911. Specify the stages of cardiopulmonary resuscitation
1) artificial ventilation, chest compressions; 2) restoration of airway patency, indirect cardiac massage; 3) restoration of airway patency, artificial ventilation; 4) indirect cardiac massage, restoration of airway patency, artificial ventilation; 5) restoration of airway patency, intracardiac administration of adrenaline.
912. Name one of the main symptoms of clinical death
1) lack of breathing; 2) absence of blood pressure in peripheral vessels; 3) “cat’s eye” symptom; 4) cadaveric spots; 5) deathly pale skin color.
913. Name one of the additional symptoms of clinical death
1) lack of breathing; 2) lack of consciousness; 3) complete relaxation of all smooth and striated muscles; 4) lack of blood circulation; 5) “cat’s eye” symptom.
914. In critical situations, the pulse of a newborn must be determined
1) on the radial artery; 2) on the brachial artery; 3) on the temporal artery; 4) on the carotid artery; 5) on the femoral artery.
915. Resuscitation is underway
1) in each case of sudden clinical death; 2) only for children; 3) the adult population of working age; 4) only young and healthy people; 5) children from 1 month and adults up to 65 years old.
916. Cardiopulmonary resuscitation is not indicated in case of
1) presence of signs of biological death; 2) absence of pupillary reflex; 3) lack of breathing; 4) lack of consciousness; 5) lack of blood circulation.
917. To perform cardiopulmonary resuscitation, the victim must be laid down
1) in a stable lateral position; 2) on the back, at the level of the resuscitator’s knees; 3) with a cushion under the head; 4) with the head end lowered; 5) on the bed.
918. Indicate at what stage CPR begins
1) indirect cardiac massage; 2) artificial ventilation; 3) ensuring patency of the upper respiratory tract; 4) administration of drugs intravenously; 5) electrical defibrillation.
919. During transportation, a victim with a traumatic brain injury begins to vomit. Necessary
1) place the victim in the “frog” position; 2) turn the victim on his side; 3) turn the victim’s head to the side; 4) place the victim on his stomach; 5) there is no correct answer.
920. The victim has a head injury, there is no consciousness. To ensure patency of the upper respiratory tract it is necessary
1) place the victim in a stable lateral position; 2) lay the victim on his back, tilt his head back, placing a cushion under his shoulders; 3) put a Shants collar on the victim, push his lower jaw forward, insert an air duct; 4) place the victim on his stomach; 5) lay the victim on his back, turning his head to the side.
921. Artificial ventilation of the lungs is carried out with frequency
1) 12 - 14 breaths per minute; 2) 16 - 18 breaths per minute; 3) 1 - 2 breaths per 1 minute; 4) 9 - 12 breaths per minute; 5) 18 - 20 breaths per minute.
922. Maximum CPR time
15 minutes; 2) 30 minutes; 3) 1 hour; 4) 2 hours; 5) 45 minutes.
923. The resuscitator during CPR is located
1) on the right side; 2) from any side; 3) on the left side; 4) behind; 5) facing the victim.
924. When performing chest compressions on an adult victim, chest compressions are performed with frequency
1) 20 - 30 compressions per minute; 2) 100 - 120 compressions per minute; 3) 130 - 140 compressions per minute; 4) 50 - 60 compressions per minute; 5) 120 - 130 compressions per minute.
925. When performing resuscitation, the ratio of compressions and breaths
1) 18:1; 2) 15:1; 3) 30:2; 4) 10:2; 5) 15:2.
926. Ventilation is most effective
1) when bending the victim’s head; 2) when the victim’s head is straightened; 3) with the victim in a lateral left position; 4) with the victim in a lateral right position; 5) the position of the victim does not matter.
927. The reasons for the insufficient effectiveness of artificial lung ventilation include all except
1) frequency of artificial ventilation of the lungs is 10 - 14 per minute; 2) lack of airway patency; 3) poor sealing between the resuscitator’s mouth and the patient’s nose; 4) insufficient volume of air entering the patient’s respiratory tract; 5) there is no correct answer.
928. Clinical death is characterized by all symptoms except one
1) absence of heartbeat; 2) constriction of the pupils; 3) cyanosis or pallor of the skin; 4) pupil dilation; 5) lack of breathing.
929. The causes of terminal conditions are
1) acute (massive) blood loss; 2) severe (massive) injuries; 3) acute poisoning; 4) acute myocardial infarction, cardiogenic shock; 5) all answers are correct.
930. Ventilation is performed correctly if the patient
1) spontaneous breathing is restored; 2) the chest remains motionless; 3) the chest rises when air is blown in; 4) rare spontaneous breaths are observed; 5) a pulse appears in the peripheral arteries.
931. The size of the duct is determined by the distance
1) from the right eye to the tip of the nose; 2) from the nose to the lower lip; 3) from the upper incisors to the chin; 4) from the chin to the earlobe; 5) from the corner of the mouth to the earlobe.
932. The air duct is used for the purpose
1) eliminating tongue retraction; 2) restoration of patency of the upper respiratory tract at the tracheal level; 3) preventing aspiration of vomit; 4) the most convenient way to perform CPR; 5) fixation of the lower jaw.
933. The criterion for the effectiveness of CPR is
1) upward movement of the patient’s chest when air is blown in; 2) immobility of the patient’s chest when air is blown in; 3) the appearance of spontaneous breathing; 4) the appearance of pulsation in the peripheral arteries; 5) stabilization of blood pressure in peripheral arteries.
934. Criterion for the correct performance of indirect cardiac massage
1) the appearance of pulse waves on the common carotid artery during compression; 2) the appearance of an independent pulse in the common carotid artery; 3) increased blood pressure in the peripheral arteries; 4) the appearance of spontaneous breathing; 5) by changes in skin color.
935. Complications may occur during chest compressions
1) damage to the esophagus; 2) hypovolemia; 3) hypoglycemia; 4) rib fracture; 5) lung rupture.
936. Cardiopulmonary resuscitation may be discontinued
1) if resuscitation is ineffective within 10 minutes; 2) if the resuscitator has doubts about its effectiveness; 3) if the victim has signs of deep hypothermia; 4) in victims with an antisocial appearance; 5) if resuscitation is ineffective within 30 minutes.
937. Factor that prolongs the duration of clinical death
1) hypothermia; 2) hyperthermia; 3) normothermia; 4) oliguria; 5) dyspepsia.
938. Moderate throwing back of the head, pushing the lower jaw forward, opening the victim’s mouth is
1) Korotkoff maneuver; 2) Heimlich maneuver; 3) taking Saffar; 4) Marconi maneuver; 5) Zaitsev’s technique.
939. Closed cardiac massage should be performed with the palm of the working hand
1) in the area of the upper third of the sternum; 2) two fingers below the xiphoid process of the sternum; 3) in the epigastric region; 4) two fingers above the middle third of the sternum; 5) two fingers above the xiphoid process or at the border of the middle and lower third of the sternum.
940. Ventricular fibrillation of the heart can be distinguished from asystole
1) using an electrocardiograph; 2) according to the condition of the pupils; 3) by pulse wave; 4) by skin color; 5) by fluctuations in blood pressure levels.
941. The maximum duration of clinical death at an ambient temperature of 15 - 20 ° C is
1) 20 minutes; 2) 5 minutes; 3) 1 - 2 minutes; 4) 2 - 3 minutes; 5) 10 minutes.
942. Ventilation using an Ambu bag
1) less effective, but more convenient; 2) less convenient, but more effective; 3) no more effective and safe than using the mouth-to-mouth method; 4) in terms of transmission of infection, it is safer for the resuscitator than the “mouth-to-mouth” method; 5) can only be carried out by a resuscitator.
943. When performing chest compressions on an adult, the sternum should shift to
1) 1 - 2 cm; 2) 5 - 6 cm; 3) 10 cm; 4) 8 cm; 5) 6 cm.
944. Saffar's triple move includes
1) precordial beat, palpation of the pulse, determination of the pupil’s reaction to light; 2) opening the mouth, removing dentures, fixing the tongue; 3) cleansing the oral cavity, removing dentures, throwing back the head; 4) measurement of blood pressure, determination of skin color, determination of the pupillary reflex; 5) throwing back the head, shifting the lower jaw downwards, moving the lower jaw forward.
945. The first actions of a nurse after declaring clinical death in a patient (victim)
1) measuring blood pressure in peripheral vessels and calling a doctor; 2) calling a doctor through an intermediary and immediately administering cardiac medications; 3) calling a doctor through an intermediary and immediately starting cardiopulmonary resuscitation; 4) calling a doctor and trying to restore breathing by supplying 100% humidified oxygen; 5) from measuring blood pressure.
946. The main symptoms of clinical death are
1) lack of consciousness, lack of breathing, lack of pulsation in the common carotid arteries; 2) lack of consciousness, cyanosis of the skin, absence of the pupillary reflex; 3) lack of consciousness, absence of pupillary and corneal reflexes; 4) lack of consciousness, lack of pulsation in the radial arteries, convulsions; 5) lack of consciousness, lack of breathing, convulsions.
947. Swelling of the epigastric region during mechanical ventilation indicates
1) about the correctness of its implementation; 2) about the effectiveness of its implementation; 3) about air getting into the lungs; 4) about air entering the stomach; 5) the uselessness and hopelessness of mechanical ventilation.
948. Reversible terminal conditions include
1) agony; 2) biological death; 3) social death; 4) chronic diseases in their terminal stages; 5) anisocoria.
949. Pre-agony, agony and clinical death refer to the conditions
1) acceptable; 2) terminal; 3) extraordinary; 4) clinical; 5) irreversible.
950. Resuscitation is considered effective in the case of
1) the appearance of pulse waves on the common carotid artery during chest compressions; 2) if 15 minutes have passed since the start of resuscitation measures; 3) if 30 minutes have passed since the start of resuscitation measures; 4) timely arrival of the ambulance team; 5) the appearance of signs of vital activity during its implementation.
951. Triple reception of Saffar provides
1) protection against hyperventilation; 2) impossibility of aspiration of gastric contents; 3) airway patency; 4) patency of the lower respiratory tract; 5) better fixation of dentures.
952. Biological death begins with death
1) liver; 2) cells of the cerebral cortex; 3) kidneys; 4) cells of subcortical structures of the brain; 5) hearts.
953. The main symptom of a typical acute myocardial infarction
1) severe headache; 2) hypertension; 3) fear of death; 4) intense pain behind the sternum; 5) shortness of breath.
954. Aerosol form of nitroglycerin
1) nitromint; 2) nitrazepam; 3) nystatin; 4) Novigan; 5) no ticket.
955. Patients with acute myocardial infarction
1) register at the reception department; 2) undergo mandatory sanitary treatment; 3) immediately sent to the intensive care unit; 4) be sure to weigh yourself; 5) are hospitalized in the therapeutic department.
956. Acute vascular insufficiency is characterized by
1) increased blood pressure; 2) a sharp decrease in vascular tone; 3) bradycardia; 4) dry skin; 5) decrease in coronary blood flow.
957. Hypertensive crisis is a condition characterized by
1) loss of consciousness; 2) a sharp decrease in blood pressure; 3) a sharp increase in blood pressure; 4) involuntary urination; 5) convulsions.
958. To provide emergency care during a hypertensive crisis, it is preferable to use
1) nifedipine; 2) nitroglycerin; 3) nalaxone; 4) no-shpu; 5) norwax.
959. Name the main action of a nurse when a patient develops pulmonary edema
1) administration of adrenaline; 2) administration of clonidine; 3) supply of oxygen through a defoamer; 4) supply of 100% humidified oxygen; 5) laying the patient down with the leg end raised.
960. To provide emergency aid for nosebleeds, it is necessary to prepare
1) heating pad; 2) ice pack; 3) furatsilin solution; 4) 70% ethyl alcohol; 5) warming compress.
961. Before using nitroglycerin during an attack of angina, the nurse must
1) determine the presence of consciousness in the patient; 2) ask when the patient last took nitroglycerin; 3) calculate the patient’s respiratory rate; 4) determine water balance; 5) monitor the patient’s blood pressure level.
962. A sudden increase in blood pressure is characteristic of
1) hypertensive crisis; 2) cardiac asthma; 3) collapse; 4) state of shock; 5) diabetic coma.
963. A short-term loss of consciousness associated with a decrease in blood flow to the brain is called
1) collapse; 2) shock; 3) fainting; 4) hypertensive crisis; 5) an epileptic attack.
964. Ischemic necrosis of the heart muscle is observed when
1) angina pectoris; 2) myocardial infarction; 3) cardiac asthma; 4) pulmonary edema; 5) hypertensive crisis.
965. A persistent and long-term decrease in blood pressure due to acute vascular insufficiency is called
1) fainting; 2) collapse; 3) hypertensive crisis; 4) shock; 5) coma.
966. To lavage the stomach of an adult in case of poisoning, it is necessary to use
1) 5 l. water; 2) 12 l. water; 3) 1 l. water; 4) 10 l. water; 5) the more water, the better.
967. Attacks of suffocation, accompanied by a feeling of lack of air, inspiratory shortness of breath, the appearance of foam at the mouth, are characteristic of
1) bronchial asthma; 2) pulmonary edema; 3) hypertensive crisis; 4) myocardial infarction; 5) anaphylactic shock.
968. If a patient develops anaphylactic shock, it is necessary
1) call a doctor; 2) stop administering the drug; 3) give a stable lateral position; 4) administer adrenaline; 5) all of the above are true.
969. During an attack of angina, before giving the patient nitroglycerin, the nurse should
1) determine the NPV; 2) determine heart rate; 3) measure blood pressure; 4) measure body temperature; 5) measure body weight.
970. An attack of suffocation in bronchial asthma is characterized by
1) bubbling breathing; 2) the presence of foamy pink sputum; 3) expiratory shortness of breath; 4) the presence of acrocyanosis; 5) copious discharge of purulent sputum.
971. The erectile phase of shock is characterized by
1) lethargy; 2) psychomotor agitation; 3) convulsions; 4) low blood pressure; 5) high blood pressure.
972. The torpid phase of shock is characterized
1) excitement; 2) confusion, decreased blood pressure; 3) pathological type of breathing; 4) increased body temperature; 5) increased blood pressure.
973. If a victim who has received an electrical injury is unconscious, but there are no visible circulatory and respiratory disorders, the nurse should
1) immediately begin chest compressions; 2) immediately begin mechanical ventilation; 3) administer intravenous adrenaline; 4) bring a cotton ball moistened with ammonia to the victim’s nose; 5) deliver a precordial blow.
974. Electrical injury of the first degree of severity is characterized by
1) convulsive muscle contraction without loss of consciousness; 2) circulatory disorder; 3) breathing disorder; 4) clinical death; 5) biological death.
975. During a ski trip on a frosty day, a white spot appeared on his cheek, in the area of which there is no sensitivity when touched by fingers. In this case it is necessary
1) rub the affected area with snow; 2) rub your cheek with a mitten; 3) warm (apply your palm) the affected area; 4) rub the affected area with an alcohol-containing liquid; 5) apply a cold compress.
976. A woman spilled boiling water on her feet. The skin on both legs and feet is hyperemic, there are blisters filled with clear liquid on the skin. Determine the degree of the burn and its area.
1) 1st degree – 18%; 2) 2nd degree – 18%; 3) 2nd degree – 9%; 4) 1st degree – 9%; 5) 3rd degree – 4%.
977. The area of a burn to the head and neck in an adult is
1) 18%; 2) 9%; 3) 20%; 4) 2%; 5) 10%.
978. In case of pulmonary edema, an oxygen cushion of 25 liters must be used up
1) in 1 minute; 2) in 10 minutes; 3) in 60 minutes; 4) in 15 minutes; 5) in 5 minutes..
979. Specify the actions of a nurse in case of a thermal burn
1) remove the thermal agent; 2) call an ambulance; 3) sit or lay the patient down, depending on the location of the burn; 4) apply an aseptic bandage; 5) all of the above are true.
980. The oxygen supply rate for pulmonary edema is
1) 1 liter per minute; 2) 2 - 3 liters per minute; 3) 4 - 6 liters per minute; 4) 8 - 10 liters per minute; 5) 10 liters per minute.
Prognosis and possible prevention
Predicting the situation while a patient is in a coma is based on the degree of brain damage and the causes of the disease. The more severe the patient’s condition, the more likely an unfavorable outcome is possible. The patient's chances of recovery are assessed according to the following measures:
- precoma, coma I - the prognosis is favorable, complete recovery is possible without residual effects;
- coma II and III - an unreliable position that can lead to both recovery and death of the patient,
- coma IV - in most cases leads to the death of the patient, the prognosis is extremely unfavorable.
Early prevention is focused on timely diagnosis of major disorders of the cardiovascular system, various tumor pathologies and other conditions that can lead to coma.