- home
- Gynecology
- Adhesions in the pelvis
Interview with Prof. Puchkov on Medical Channel 1 on the topic: “Adhesive disease and infertility”
Adhesions in the pelvis are adhesions of connective tissue that appear on the surface of the pelvic organs. As a result, their mobility is limited and function may be impaired. When these organs are displaced, the adhesions become tense, which leads to pain.
The formation of adhesions refers to a protective reaction of the body aimed at delimiting a pathological focus from healthy tissues that appears due to various reasons: trauma, inflammation, exposure to air, circulatory disorders, etc. With any damage, the body strives to grow a new one on the unprotected area of the mesothelium, and substances are released , synthesizing fibrin. As a result, nearby organs are “glued together” with fibrin fibers.
Most often this occurs during surgical interventions, for example, after myomectomy, and adhesions in the pelvis after cesarean section are not uncommon. They also appear in urgent conditions associated with bleeding (for example, during ectopic pregnancy, ovarian apoplexy, abscesses, etc.), and adhesions in the pelvis in women are formed due to various diseases, for example, endometriosis, salpingitis, oophoritis, fibroids. The likelihood of the formation of adhesions depends on a number of factors: the properties of connective tissue determined genetically, weakened immunity and the individual predisposition of tissues to adhesions.
What are adhesions in gynecology
Adhesive disease of the pelvic organs in women is a complication after which fibrinous connective tissue grows between the pelvic and abdominal organs.
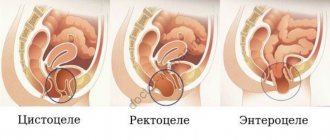
In this way, the body tries to protect the source of inflammation - due to excess tissue, the fallopian tubes, uterus, ovary and intestinal loops stick together, pull tightly together, which disrupts their functions. Adhesive processes can be of several types, depending on the “neglect”:
- Formation of single thin adhesions (synechia).
- Synechiae become denser, covering up to 50% of the surface of the ovary.
- The adhesions are dense and numerous, changing the position of organs or causing their deformation.
Adhesions cause pain and disturbances in the functioning of the pelvic organs. They appear after gynecological diseases or operations and can lead to serious complications: ectopic pregnancy, infertility, frequent inflammation and more.
To prevent the occurrence of adhesions, avoid complications and prescribe competent treatment, make an appointment with the doctors of the Doctor A clinic. We employ gynecologists of the first and highest qualification categories
Causes of vaginal ruptures
Unfortunately, no matter how ideally the perineal muscles are “designed,” there are many factors that reduce their elasticity and contribute to perineal rupture. Among them:
- the woman’s age is more than 35 years, especially if this is her first birth;
- high perineum (when the distance between the anus and the entrance to the vagina is more than 7-8 cm);
- developed muscles of the perineum (for example, in women who play sports professionally);
- scars on the perineum after injuries received during previous childbirth or as a result of plastic surgery;
- swelling of the perineum (with weakness of labor, prolonged pushing);
- fast and rapid childbirth;
- insufficient protection of the perineum (reception provided by the midwife) when removing the baby’s head and shoulders;
- inappropriate behavior of the woman in labor - during childbirth, especially during the second period, when the fetus is expelled, it is necessary to strictly follow the recommendations of the doctor and midwife who monitor the condition of the perineum. Premature pushing, strong pushing at the moment when it is necessary to breathe through the contraction (at the moment of removal of the fetal head and shoulders), contribute to the appearance of ruptures.
Do not forget that the inflammatory process in the vagina (colpitis, vulvovaginitis) contributes to significantly greater trauma to the soft tissues of the birth canal. Therefore, all women are recommended to undergo smears for vaginal flora at 36 weeks of pregnancy and, if necessary, undergo appropriate treatment.
Tears can be internal (on the cervix and inside the vagina) and external (at the exit of the vagina). Cervical ruptures most often occur at the end of the first stage of labor, when the cervix has not yet fully opened, and the fetal head is already pressed against the entrance to the pelvis, putting pressure on the bladder and rectum; at the same time there is a desire to push and thereby get rid of the pain. However, this should not be done under any circumstances, since pressure on the cervix that has not yet opened leads to its rupture.
In turn, according to the principle “the force of action is equal to the force of reaction,” the cervix puts pressure on the fetal head and leads to additional injuries to the unborn child. The fetal head should descend slowly, gradually expanding the tissues of the vagina and perineum. Any forcing can lead to vaginal injuries - abrasions and ruptures. To prevent this from happening, you need to listen to the recommendations of the doctor and midwife and not push before the head completely fills the entire vagina and reaches the exit from the pelvis. During the birth of the head and shoulders of the fetus, the mucous membrane of the labia may be injured. This occurs when the head is rapidly extended during birth.
What causes adhesions to form in the pelvis
Inflammation of the pelvic organs. The disease is diagnosed in women who have suffered acute inflammation or suffer from chronic:
- colpitis;
- endometritis;
- andexite;
- parametritis and other diseases.
Operations. Adhesive disease appears in 16% of those operated for the first time and in 96% of women after the third operation. The percentage is high for laparotomy operations:
- appendectomy;
- C-section;
- removal of appendages;
- hysterectomy;
- supravaginal amputation.
Pelvic hemorrhages. The trigger is ovarian apoplexy, bleeding due to a ruptured tube during an ectopic pregnancy.
Endometriosis. The formation of fibrinous ties is provoked by endometrioid growths, which spread to the organs and peritoneum of the pelvis.
Pelvic injuries. Open and closed damage after accidents, falls from a height received at work are one of the reasons for the appearance of adhesions.
Predisposing factors. The occurrence and development of the disease is influenced by:
- invasive gynecological interventions;
- promiscuous sex life;
- late visit to the clinic.
Adhesions in gynecology: symptoms
The adhesive process can be both acute and chronic, or have a periodic nature (with periodic exacerbation of symptoms). Often, women do not notice any symptoms of adhesions in the pelvis, and the disease is discovered only when examining the possible causes of infertility.
Signs of adhesions in the pelvic cavity:
- Painful sensations in the lower abdomen, lower back, above the pubis or in the sacral area;
- Discomfort during physical activity, before menstruation, after stressful situations;
- Pain during sexual intercourse or urination;
- Intestinal disorders: diarrhea, constipation, flatulence;
- Periodic attacks of nausea and vomiting.
Symptoms may worsen when consuming foods that increase gas formation.
Recommendations after posterior vaginoplasty with perineoplasty
- Avoid heavy physical activity for 4 weeks.
- Avoid intimacy for 4 weeks.
- Avoid using tampons for 4 weeks; use only pads to collect discharge.
- Until complete recovery, you should not wash in the bathroom, overheat, or introduce medications not recommended by doctors into the genital tract. It is allowed to use only drugs prescribed by a gynecologist.
Violation of recommendations can lead to bleeding, infections, swelling, pain, and prolongation of the healing period.
Diagnosis of the disease
Diagnosis of adhesions in the pelvis is carried out using various studies:
- Diagnostic laparoscopy. This method can most accurately see adhesions and assess the severity of the process. Diagnosis is carried out under local (or general) anesthesia; a small incision is made through which a camera is inserted.
- Ultrasound of the pelvic organs;
- Hysterosalpingography (performed using X-rays or ultrasound and contrast agents);
- MRI of the pelvic organs.
The necessary examination (or set of examinations) will be prescribed to you by your attending physician.
Results of posterior vaginoplasty with perineoplasty
All patients operated on since 2014 at the Department of Plastic and Reconstructive Surgery at the University of Toronto, Canada, were satisfied with the operation. These were women of different ages - from 23 to 58 years old. Among them, 86.7% of patients had previously given birth vaginally several times, and 13.3% had one birth. Only one had never had a vaginal birth. The average operative time was 68 minutes.
Two women stated that, despite improvement in preoperative symptoms, they would like to further narrow the genital tract. They underwent repeat corrective vaginoplasty under local anesthesia.
Many patients underwent other plastic surgeries simultaneously with perineal and vaginal plastic surgery. The most common of them was labiaplasty - changing the shape of the labia. Many also enlarged the mammary glands and performed tummy tuck - abdominoplasty. Other aesthetic surgeries were also performed, indicating the growing desire of modern women for beauty.
How to treat adhesions in the pelvis
What to do if adhesions are found in the pelvis? Depending on the severity of the adhesive process, the doctor will select the appropriate treatment for you.
To treat single thin adhesions in the pelvis in women, drug therapy is used. What is usually prescribed:
- Antibiotics and antimicrobial agents (to relieve inflammation);
- Non-steroidal anti-inflammatory drugs (as a pain reliever);
- Fibrinolytic agents (for resorption of adhesions);
- Vitamins and immune system regulators (to restore immune balance);
- Hormonal drugs (in cases where adhesions are caused by endometriosis).
Additionally, physiotherapy, balneotherapy and mud therapy may be prescribed as auxiliary measures.
In more severe forms of adhesive disease, a surgical method is used to treat adhesions in the pelvis, i.e. their dissection. The most gentle surgical procedure is manipulative laparoscopy. To prevent re-formation of adhesions, hyaluronic acid is injected into the surgical area.
Principles of treatment
Treatment of adhesions and elimination of the adhesive process is possible using conservative methods of therapy. These include:
- The use of physiotherapy is the impact of ultrasound, high-frequency current, magnetic waves on the commissure and the area where it is located. This allows you to slow down the process of proliferation of connective tissue.
- Drug treatment.
If adhesions are detected, surgical intervention by doctors is required. Surgical treatment will help solve this gynecological problem by eliminating already formed adhesions. The operation is a dissection of the commissure and is usually performed laparoscopically - through small punctures and under video control. If possible, the adhesive tissue is removed, and the attachment sites of the adhesions are cauterized using electrodes. Recovery after removal of scar tissue through laparoscopic access lasts several weeks. In the postoperative period, the woman is under the supervision of specialists.
Is it possible to get pregnant during adhesions?
Adhesions disrupt the proper functionality of the reproductive organs, which greatly reduces the chance of getting pregnant. There is a chance of pregnancy and its successful gestation, especially in cases where the adhesive process affected only one tube. But the likelihood of conception decreases, and the risk of ectopic pregnancy and miscarriage also increases.
In this case, IVF may help. The fallopian tubes are not involved in such fertilization, and a 3-5-day-old embryo is immediately implanted into the uterine cavity.
Classification
Intestinal adhesions are classified according to the degree of strength and some morphological characteristics. The scale for assessing the severity of the adhesive process is as follows:
- 0 points - no adhesions;
- 1 point - single fusion, membranous structure, without narrowing of the intestinal lumen (divided in a blunt manner);
- 2 points - two adhesions of a loose structure without blood vessels. The intestinal tube is moderately deformed, the lumen is not narrowed (divided in a blunt way, in rare cases sharp);
- 3 points - more than two adhesions. Dense, can grow blood vessels. The intestine is deformed, the lumen is narrowed to 50% (divided only by acute means);
- 4 points - conglomerate of adhesions. They are dense, permeated with blood vessels. The deformation of the intestinal tube is extensive, the lumen is narrowed by more than 50% (they are separated only by an acute method, it is difficult to avoid trauma to the fused organ).
Prevention of adhesions
For the prevention and treatment of adhesions, enzyme preparations based on hyaluronidase are used. Perhaps the most popular drug for the treatment of adhesions in gynecology is Longidaza suppositories.
Prevention is mostly aimed at preventing relapses of the disease or before an upcoming operation (since adhesions often appear after them).
Remember that the best prevention is regular visits to the doctor and timely diagnosis. Don’t delay until later and sign up for a pelvic ultrasound or a consultation with a gynecologist.
If you feel acute pain in the abdominal cavity or pelvic organs, do not delay visiting a doctor - prevent the development of the disease. Doctors at the Doctor A clinic will conduct an expert examination and prescribe competent treatment. Call or make an appointment online.
Selecting a method
Perineal incisions can be of two types: perineotomy - an incision directed directly towards the rectum, and episiotomy, in which the incision is directed to the side (if you imagine the perineum as a dial, then we can say that perineotomy is performed at 5 or 8 o'clock).
The method of dissection of the perineum during childbirth is chosen taking into account the characteristics and pathological changes of the perineum, the obstetric situation, and the size of the fetus.
Perineotomy
carried out during the normal mechanism of labor in case of a threat of rupture of the “high” perineum (increased compared to the norm the distance between the posterior commissure of the labia majora and the anus), as well as in case of premature birth.
Indications for episiotomy
are the threat of rupture of the “low” perineum (when the distance between the rectum and the entrance to the vagina is small), acute subpubic angle (the angle at which the bones of the pubic symphysis meet), breech presentation of the fetus, cicatricial changes in the perineum, obstetric operations (application of obstetric forceps, vacuum -extractor). Lateral episiotomy - an incision strictly to the side - is carried out only in case of pathological changes in the perineum that do not allow the use of another method of dissection (for example, for tumors) - such incisions heal worse.
Perineotomy and episiotomy are performed in the second stage of labor, when the presenting part of the fetus has sank to the pelvic floor and tension in the perineum appears, before its rupture occurs. The operation is performed by a doctor; in emergency cases, in his absence, by a midwife. The perineotomy operation does not require pain relief, since ischemia (lack of blood supply) of the perineal tissue leads to loss of pain sensitivity. Before dissection, the skin of the perineum is treated with tincture of iodine. The incision is usually made with scissors at the moment the fetal head erupts. Its length is on average 2-3 cm. Blood loss, as a rule, is small. Restoration of the cut perineum is carried out after the birth of the placenta.