Metrorrhagia is uterine bleeding that occurs outside of menstruation and is not cyclical. In order to avoid dangerous complications, it is very important to diagnose the pathology in a timely manner and undergo a course of treatment. You can make an appointment with a doctor by calling the number listed on the website or using the booking button.
The volume and duration of discharge may vary and depend on the reasons underlying the development of bleeding. Metrorrhagia, unlike menstrual bleeding, can occur at any age, and not just during the reproductive period.
How to assess the intensity of bleeding
At an appointment with a gynecologist, it is very difficult to determine the amount of blood lost per day, so some gynecologists focus on filling and changing hygiene products. One pad contains approximately 5 ml, and one pad contains from 5 to 15 ml, depending on the absorption strength. Based on this, more than 16 tampons or 6 to 16 blood-soaked tampons indicates 80 ml of wasted blood. There is a subjective scale for assessing the intensity of release:
- Minor discharge. A few spots on the female's smear at the end of the day correspond to a daily blood loss of 5-6 g.
- Very light. The hygiene product is changed 1-2 times a day, which is equivalent to the loss of 6-9 g of blood.
- Lungs. A feminine sanitary pad or regular tampon is changed 3-4 times a day. This blood loss corresponds to 8-13 g per day.
- Moderate. If a tampon or (normal) tampon is changed every 4-5 hours, we can talk about blood loss of 12-15 g per day.
- Strong. Super hygienic products must be replaced after 3 hours. This is 15-18 g of blood per day.
- They are very strong. Super absorbent tampons and pads get wet within an hour. This condition requires urgent medical attention; blood loss cannot be counted. This is a clear sign of menorrhagia.
It is important to consider that the intensity of blood loss during menarche varies and depends on the day of the cycle: in the first days the discharge will be moderate, and in subsequent days it will be light and barely noticeable. The normal amount of blood released is considered to be 250 ml, which corresponds to one glass. Anything is considered a possible menorrhagia.
What is menorrhagia
Menorrhagia (heavy menstruation) is blood loss during menstruation that exceeds the physiological norm (~ 150 ml). It can serve as a manifestation of inflammatory processes in the female genital area, uterine fibroids, ovarian dysfunction, and neuropsychic fatigue. This is associated with the development of anemia in women, disability and an increase in quality of life. Other complications depend on the cause of the underlying disease. Menorrhagia is diagnosed based on anamnesis, gynecological examination, and ultrasound of the pelvic organs. If necessary, a biopsy and cytological examination are performed. Treatment of menorrhagia can be therapeutic or surgical.
Menorrhagia is one of the variants of hypermenstrual syndrome (heavy menstruation), in which regular menstrual bleeding lasts more than 7 days and blood loss exceeds 100-150 ml. Heavy and prolonged menstruation bothers about 30% of women, but not all of them turn to a gynecologist with the problem of menorrhagia. There is a distinction between primary menorrhagia, which occurs simultaneously with the first menstruation, and secondary menorrhagia, which develops after a period of normal menstruation.
Juvenile metrorrhagia
Juvenile metrorrhagia occurs in adolescence and is usually due to the following reasons:
- imbalance of hormones due to psycho-emotional stress, infectious diseases, significant physical activity, PCOS.
- disorders in the hemostatic system (for example, thrombocytopenia)
- development of space-occupying formations (for example, ovarian cysts).
It is necessary to differentiate between juvenile bleeding and menstruation when the cycle has not yet been established.
Types of menorrhagia
Pubertal (primary) menorrhagia
The diagnosis of abnormal uterine bleeding or pubertal menorrhagia is made in adolescent girls from the first day of menstruation to 17 years of age inclusive. Bleeding does not correspond to the parameters of normal menstruation and causes discomfort to girls. Menorrhagia can occur due to the formation of normal, regular menarche, but sometimes indicates pathological disorders of the reproductive system of a teenage girl. Most often, menorrhagia occurs in the first 3 years from the first day of the first menstruation. Complications of pubertal menorrhagia can be acute blood loss syndrome and anemic syndrome.
Idiopathic menorrhagia
Abnormal bleeding in adolescents and mature girls coinciding with menstruation for an unknown reason. Idiopathic menorrhagia is difficult to treat; the doctor prescribes a symptomatic treatment regimen for menorrhagia to alleviate the girl’s condition. The patient requires a thorough examination to identify the cause of menorrhagia.
Secondary menorrhagia
Develops in mature women with a regular menstrual cycle. Typically, menstruation has been normal in the past. Secondary menorrhagia indicates possible diseases of the female reproductive system and requires a thorough examination by a gynecologist.
Treatment and possible complications of menorrhagia
Depending on the etiology of menorrhagia, different treatment options are possible:
- Non-steroidal anti-inflammatory drugs that can reduce the severity of bleeding in menorrhagia by up to 46%.
- Oral contraceptives and progestin therapy, drugs limit the proliferative function of estrogen on the endometrium.
- Hemostatic medications that reduce the severity of bleeding and the duration of menarche.
- Sometimes ablation (resection) of the endometrium is prescribed. This is a minor surgical intervention for menorrhagia, in which the thin lining of the uterus is removed. It is used in women with anemic syndrome who have achieved reproductive goals.
Menorrhagia in adolescents
Since adolescents are characterized by hormonal instability, menorrhagia often occurs in girls 13-16 years old. The main cause of teenage menorrhagia is an imbalance between the levels of progesterone and estrogen, which affect the maturation and shedding of the uterine endometrium. Exacerbation of the menstrual cycle can develop with an enlarged thyroid gland, poor blood clotting and genital tract infections. A common cause of teenage menorrhagia is hereditary forms of coagulopathy (hemostasis disorders).
Menorrhagia is especially severe in adolescents and requires immediate consultation with a doctor to determine the causes and correct the disorders. Without treatment for teenage menorrhagia, 30% will develop polycystic ovarian disease in the future.
At the initial consultation with the girl, the mother must accompany her and inform the doctor about her family history, the course of pregnancy and the illnesses of the child. The doctor evaluates the patient’s anthropometric data (height, weight), the degree of development of secondary sexual characteristics in order to exclude pathological processes affecting the girl’s development. The time of onset of menstruation, features of the course and characteristics of the menstrual cycle (cycle length, duration, profuseness and pain of menstrual bleeding, etc.) are identified. Attention is drawn to the problems of the influence of menstruation on the general well-being and performance of the girl (misses classes due to menorrhagia, attends sports clubs, etc.). This information is an important indicator of the adolescent’s general and gynecological health.
In case of menorrhagia in adolescents, it is mandatory to study the hemoglobin content in the blood to detect anemia. In the presence of iron deficiency anemia, patients with menorrhagia are prescribed iron supplements. To regulate the menstrual cycle during teenage menorrhagia, hormonal contraceptives are used in small doses, containing no more than 35 mcg of the estrogen component in 1 tablet of the drug. It will be useful to teach a girl how to keep a menstrual calendar, recording the features of the menstrual cycle.
The effectiveness of the treatment of menorrhagia is assessed after approximately 6 months, and its indicator is the restoration of the normal volume of menstrual bleeding. Further observation by a gynecologist is standard - 2 times a year.
Prevention of menorrhagia
Compliance with preventive measures will help prevent the development of menorrhagia in both adolescents and mature women. Such preventive measures should include abstaining from heavy physical activity and avoiding heavy strength exercises. It is necessary to avoid stressful situations and not be overtired. Changes in climatic conditions also play a role in the development of menorrhagia. Taking multivitamin preparations such as vitamins B and C, iron and folic acid are also preventive measures in preventing menorrhagia.
Causes of menorrhagia
In 40-60% of cases, the cause of heavy menstruation remains unclear.
In other cases, the causes of large blood loss during menstruation may be the following:
- polyps (benign growths) in the uterus or cervix;
- endometriosis is a gynecological disease when cells of the uterine mucosa grow in its muscle layer or in other organs;
- Uterine fibroids are benign growths in the uterus that can cause pain in the pelvic area
- intrauterine device - after its installation, blood loss may increase by 40-50%;
- pelvic inflammatory disease (PID), an infection of the uterus, fallopian tubes, or ovaries that can cause pelvic pain, fever, or bleeding after sex or between periods;
- polycystic ovary syndrome - the formation of cysts in the ovaries;
- bleeding disorders;
- underactive thyroid gland (hypothyroidism) – can cause fatigue, constipation, cold intolerance and changes to the skin and hair;
- liver or kidney disease;
- uterine cancer (very rare).
Sometimes heavy periods can be caused by medical intervention, namely:
- prescribing drugs that prevent blood clotting (anticoagulants);
- chemotherapy (cancer treatment method).
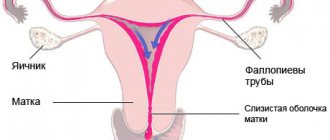
How does the menstrual cycle work?
To understand why metrorrhagia is a pathology, you should study the menstrual cycle and all the changes that occur during this period.
Menstruation is the first phase of the menstrual cycle. It is called follicular, because during this period the follicle with the egg inside begins to mature. During this time, the levels of various hormones, especially estrogen, increase.
The follicular phase ends, giving way to ovulation, approximately in the middle of the cycle. The onset of ovulation is promoted by the hormones estradiol and luteinizing hormone. On this day, the egg leaves the follicle and moves through the fallopian tubes to the uterus. Fertilization occurs in the removed tube.
The second phase of the cycle is the luteal phase (corpus luteum phase). It occurs after ovulation and characterizes the period of development of the corpus luteum, which appears at the site of the egg in the ovary. The corpus luteum actively produces progesterone (pregnancy hormone). During the luteal phase, the body actively prepares for a possible pregnancy. The endometrium of the uterus thickens. This period lasts on average 13 days.
If fertilization does not occur, the egg dies. The brain receives the command, the corpus luteum dies. The inner layer of the uterus is shed and discharge begins. The corpus luteum leaves the body along with them.
Symptoms of menorrhagia
So, having learned that menorrhagia is prolonged and heavy uterine bleeding during menstruation, it is not difficult to determine the symptoms of this disease. The main symptom is heavy menstrual flow, during which a woman loses much more blood than during normal menstruation. Another symptom should be considered a long period of bleeding, which once again confirms the diagnosis of menorrhagia. If menstruation lasts more than seven days, this is a sure sign of the development of menorrhagia in a woman. Menstrual flow during menorrhagia occurs with blood clots. Additional symptoms of menorrhagia are weakness, dizziness, general malaise and fainting.
Symptoms and signs of menorrhagia
The most important symptom of menorrhagia is the patient’s complaint about an unusually heavy discharge of blood during menstruation, which contains blood clots in fairly large quantities. The symptom is subjective, but is easily verified by the number of hygiene products used per day. Menorrhagia is characterized by frequent changes of pads: one per hour.
But there are other signs that indicate to an experienced gynecologist a diagnosis of menorrhagia:
- Decrease in the quality of general condition. Complaints of malaise, constant fatigue, body weakness, dizziness, nausea.
- Uncontrolled bruising on the body for no reason, frequent bleeding from the nose or gums.
- Paleness of the skin and visible mucous membranes.
Diagnosis of menorrhagia
Contact your gynecologist if you have heavier menstrual bleeding than usual. Your doctor will review your concerns and suggest treatment options.
Take a calendar with you to your doctor's appointment in which you write down the start and end dates of your menstruation and the characteristics of your discharge.
To determine the cause of heavy bleeding (menorrhagia), your doctor will ask you the following:
- illnesses you have suffered;
- if the accompanying symptoms are bothersome;
- There are hereditary diseases in the family, blood diseases, etc.
He will also ask the following questions about your period:
- how many days do they usually last;
- how heavy is the bleeding;
- How often should you change your tampon or tampon?
- if blood drips and stains clothing or bedding;
- if heavy periods interfere with daily life.
It is important to tell your gynecologist if you have bleeding between periods (uterine bleeding), or if you notice blood after sex, or if you have pelvic pain.
Your doctor will examine you and also ask you which method of contraception you are using, if you are planning a pregnancy, and when was the last time you visited your gynecologist and had a cervical smear (cytology smear) taken.
Gynecological examination
A pelvic exam is a routine part of a gynecologist's examination during which the doctor examines the vulva, vagina, and cervix using a speculum and palpates the vagina, uterus, and ovaries with his hands. In this case, the doctor places one hand on the skin of the lower abdomen and inserts two gloved fingers of the other hand into the vagina.
A gynecological examination reveals areas of pain, signs of infection, external bleeding, etc. This study is carried out only with the consent of the woman. The doctor must answer in detail all questions regarding his manipulations.
Biopsy
In some cases, a biopsy may be required to determine the cause of menorrhagia. This is the removal of pieces of the lining of the cervix or lining of the uterus for subsequent microscopic analysis. The biopsy is performed by a gynecologist.
Blood analysis
Typically, all women with heavy periods have a complete blood count done. Helps detect iron deficiency anemia, often caused by iron loss due to prolonged heavy bleeding.
There are special medications for the treatment of iron deficiency anemia. They are prescribed by a gynecologist; in more complex cases, you may be referred to a hematologist.
If your doctor suspects an endocrine disorder is causing your heavy menstrual periods, blood tests for sex hormones or thyroid hormones may be ordered.
Ultrasound of the pelvic organs
Ultrasound of the pelvic organs (or the uterus with appendages, genital organs) is prescribed to identify causes of heavy menstruation, such as uterine fibroids, polyps, uterine cancer and others.
Ultrasound examination of the uterus with appendages is carried out both with an abdominal sensor - through the abdominal wall, and with a vaginal sensor - through the vagina. Transvaginal ultrasound allows you to examine the female genital organs at close range.
Metrorrhagia during pregnancy and childbirth
During pregnancy, as well as during and after childbirth, bleeding is also possible, the causes of which may be different:
- Abortion
- Ectopic pregnancy
- Placenta previa (a feature of the placenta being attached in such a way that it completely or partially covers the uterine os)
- Placental abruption (separation of the placenta from the wall of the uterus at any stage of pregnancy before birth)
- Uterine atony (sharp decrease in uterine tone and contractile activity in the postpartum period)
- Injuries to the lower part of the birth canal (in particular, cervical ruptures as a result of rapid labor, large fetal size, etc.)
- Retained placenta (impaired separation of the placenta from the uterine wall or the process of expulsion of the placenta)
- Inversion of the uterus
- Disorders of the hemostasis system
When to call an ambulance
If there is abundant and massive blood flow, you should immediately call an ambulance:
- blood loss;
- pallor, blue discoloration (cyanosis) of the skin;
- dizziness;
- loss of consciousness;
- a sharp decrease in blood pressure against the background of a rapid and weak pulse.
Before the ambulance team arrives, it is necessary to lay the woman on her back, raise her legs, placing a pillow or cushion under them. Place a cold compress on your lower abdomen. This could be a cold water bottle or a plastic bag of ice wrapped in a cloth. The ice pack can be left on for 10-15 minutes, followed by five-minute breaks.
Diagnosis of metrorrhagia
Diagnosis of metrorrhagia begins with a study of complaints and a gynecological examination. This disease is characterized by irregularities in the menstrual cycle. The doctor also measures your pulse and blood pressure. An important step is to assess the condition of the skin and mucous membranes. It is necessary to determine the body mass index.
Upon direct examination, the doctor determines the condition of the uterus and the intensity of bleeding. A colonoscopy may be needed to detect cervical abnormalities.
To confirm the diagnosis, an analysis of the uterine mucosa is performed. The material is taken by scraping. Histological examination helps determine the cause of dysfunction. Also, curettage is a therapeutic measure and leads to stopping bleeding.
Treatment of menorrhagia
Medicines are the main treatment for heavy periods (menorrhagia), but in some cases, cleaning the uterus may be necessary.
Treatment for heavy periods is only required when they significantly interfere with daily life and even if a medical condition is identified during testing. The goal of therapy is to restore the normal menstrual cycle, improve quality of life and combat anemia caused by heavy and prolonged bleeding.
If no deviations are found, it is recommended to lead a healthy lifestyle and consult a gynecologist every six months to monitor your health. Heavy menstruation may be a temporary phenomenon due to body characteristics.
The various treatment methods, their advantages and disadvantages are described below.
Tranexamic acid
Tranexamic acid is often recommended to shorten menstruation and reduce blood loss. This remedy accelerates blood clotting, so menstruation becomes less heavy. Blood loss is reduced by 29-58%.
Tranexamic acid can be taken as tablets or injections. The doctor selects the regimen and dosage. If there is no improvement within three months, treatment is stopped.
Tranexamic acid tablets do not affect fertility, meaning you can still become pregnant during treatment. If necessary, tranexamic acid can be combined with non-steroidal anti-inflammatory drugs (see below).
Possible side effects: stomach upset and diarrhea.
Intrauterine device "Mirena"
For the treatment of heavy menstruation, intrauterine contraceptives with a constant release of the hormone levonorgestrel are suitable. In Russia, the only system registered with this promotion is Mirena.
This is a small plastic device that is inserted into the uterus for several years and slowly releases the hormone progestin.
This substance inhibits the growth of the uterine mucosa - the endometrium and has a contraceptive effect. After removal of the intrauterine device, the chances of getting pregnant are restored.
Possible side effects:
- irregular bleeding for six months or more;
- pain in the mammary glands;
- blackheads (acne);
- lack of menstruation (amenorrhea).
The levonorgestrel-releasing intrauterine device reduces blood loss by 71-96% and is the preferred treatment for menorrhagia for postpartum women requiring long-term contraception.
Combined oral contraceptives
Combined oral contraceptives (COCs) contain estrogen and progestin, two sex hormones. COCs are taken one tablet per day for 21 days. So they take a break for seven days. During this pause the cycle begins. Then the cycle repeats.
COCs prevent eggs from maturing, that is, they block ovulation. If you follow the pill regimen, a reliable contraceptive effect is guaranteed. Oral contraceptives also reduce pain during menstruation.
Unlike the intrauterine device, oral contraceptives provide more freedom when planning a pregnancy - they can be easily terminated without visiting a gynecologist. In addition, oral contraceptives are preferable to intrauterine devices for nulliparous women and girls.
Common side effects of oral contraceptives:
- mood swings;
- nausea;
- fluid retention - swelling;
- pain in the mammary glands.
In addition, other hormonal agents are used for heavy menstruation. Some of them reduce the thickness of the uterine lining, thereby reducing blood loss during menstruation. Others cause artificial menopause, where your periods temporarily stop. Any hormonal treatment must be carried out strictly under the supervision of a gynecologist.
Nonsteroidal anti-inflammatory drugs (NSAIDs)
Nonsteroidal anti-inflammatory drugs (NSAIDs) can also be used to treat heavy periods. They reduce blood loss by 20-49% and are prescribed as tablets at the start of menstruation (or just before the start of menstruation) until the bleeding stops.
The following NSAIDs are recommended for the treatment of menorrhagia:
- mefenamic acid;
- naproxen;
- ibuprofen.
They are usually taken 3-4 times a day.
NSAIDs reduce the production of prostaglandins, which increases blood loss during menstruation. These drugs have an analgesic effect. They do not have a contraceptive effect, but if necessary they can be combined with combined oral contraceptives.
Common side effects include stomach upset and diarrhea.
NSAIDs can be used for an unlimited number of menstrual cycles as long as they relieve the symptoms of heavy periods and do not cause serious side effects. However, if NSAIDs do not produce results within three months, they are discontinued.
Operation
Surgical treatment methods may be offered in cases where the cause of heavy menstruation is certain diseases, for example, uterine fibroids, endometriosis, polycystic ovary syndrome, uterine cancer, etc. You can learn more about the operations in each specific case by following the links.
If the cause of heavy menstruation is not clear and medications cannot cope with the problem, the doctor may suggest a minimally invasive intervention: curettage of the uterus or removal of the endometrium. Another indication for such treatment is polyps of the cervix or uterine body.
Curettage of the uterus
Scraping the uterus and cervix is the removal of the top layer of the endometrium (mucous membrane) using a special surgical instrument inserted into the uterus.
First, as a rule, the mucous membrane of the cervix is removed, then the body. As a result, monthly bleeding stops. After scraping, the resulting material is sent to the laboratory to search for and exclude benign and malignant formations.
Curettage can be done “blindly,” when the doctor inserts a surgical instrument into the uterus and removes the mucous membrane according to a certain pattern. Lack of visual control can lead to various complications or incomplete curettage.
A more modern manipulation is curettage of the uterus during hysteroscopy. In this case, the gynecologist has the opportunity to visually check the removal of the endometrium using an optical endoscope - a hysteroscope, which is carefully passed through the cervix.
Curettage is most often performed under general anesthesia (anesthesia), but other methods of pain relief are possible and must be discussed with your doctor in advance.
Endometrial ablation
Endometrial ablation is prescribed as a last resort for heavy menstruation, most often in women 45 to 50 years of age and older. With this operation, the lining of the uterus is completely removed.
There are various endometrial ablation techniques, namely:
- microwave ablation of the endometrium: a probe is inserted into the uterus that uses microwave energy (a type of radiation) to heat and destroy the lining of the uterus;
- Heat balloon ablation: A balloon is inserted into the uterus, then inflated and heated to destroy the lining of the uterus.
Both local and general anesthesia (anesthesia) are used to relieve pain during ablation. The operation lasts about 20 minutes. They are usually allowed to return home the same day.
Light vaginal bleeding may persist for several days after endometrial curettage or ablation. In some women, spotting lasts up to 3-4 weeks.
GYNECOLOGICAL COMPLICATIONS IN WOMEN WITH INCREASED BLEEDING
Rice. 2.
Blood clot formation
Fibrin clot formation
At this stage, a network-like covering of the blood clot is formed - a fibrin clot (blood clot), formed through the interaction of 13 plasma clotting factors, numbered in Roman numerals from I to XIII (Fig. 3).
Deficiency of any of these proteins can result in delayed or incomplete clot formation and subsequent resumption of bleeding when the clot forms temporarily, requiring reinforcement with a fibrin clot. Rice.
3. Fibrin clot formation
Problems with increased bleeding in women
Bleeding problems can be inherited or acquired during a woman's life. Acquired increased bleeding can be caused by certain types of medications, treatments, malignant diseases and autoimmune disorders. Let us dwell on hereditary problems, which most often cause bleeding problems in women.
von Willebrand disease
Von Willebrand disease (VWD) is reported to be the most common cause of excessive bleeding in humans.
Rice.
4. Inheritance of von Willebrand disease
The presence of von Willebrand disease (VWD) is caused by a gene passed from parent to child. The abnormal von Willebrand disease gene is located on one of the regular chromosomes, not on the sex chromosome (like hemophilia), and therefore VWD occurs with equal intensity in both men and women. Often, an accurate family history can help a doctor diagnose the condition. Sometimes an abnormal gene may manifest itself for the first time in a patient when neither of the parents possessed it. This is called a new "mutation", and the disease can then be passed on to successive children in the usual way. A specific test for the von Willebrand factor gene (DNA test) is now available for some forms of von Willebrand disease. It is sometimes possible to trace von Willebrand disease over several generations. The figure above shows the usual pattern of dominant inheritance. Although the genetic defect is inherited in an autosomal manner, it does not follow the classical pattern of autosomal dominant or autosomal recessive inheritance. Moderate VWD and some forms of the disease (type 2A or 2B) appear as a consequence of the autosomal dominant model; severe VWD, with von Willebrand factor, occurs only when two genes are defective.
The exact prevalence is unknown, but some estimates suggest it is present in 1% of the world's population. BV occurs throughout the world among people of all socioeconomic and ethnic groups. This is an autosomal disease (that is, it affects both men and women equally) (Fig. 4). There are three main types of VWD depending on whether the VWF defect is quantitative or qualitative. In VWD type 1, there is a deficiency of von Willebrand factor (vW). Type 2 VWD, which has four subtypes, occurs when there is a qualitative defect in vWF (the factor does not function properly). In type 3, vWF is almost or completely absent. Most types are inherited in an autosomal dominant manner. Type 3 and 2N are inherited in a recessive manner. It is important to know which type of BV each individual patient has because treatment for different types of disease is different. If there is a significant decrease in vWF, as in type 3, or a problem with vWF associated with factor VIII, as in type 2N, then a significant decrease in factor VIII relative to normal may also occur. Sometimes people with type 3 or 2N BV are misdiagnosed as having hemophilia due to significantly reduced factor VIII. To prevent such misdiagnosis, it is necessary to check the level of factors VIII and von Willebrand when determining a blood coagulation disorder in a patient.
Signs of BV are expressed in the body's inability to form a blood clot. Bleeding mainly occurs from the mucous membrane and (or) skin. The most common signs are the presence of a large number of bruises on the body, frequent or prolonged nosebleeds, heavy or prolonged menstrual bleeding (menorrhagia) and prolonged bleeding from wounds, surgery, tooth extraction and in women in labor during childbirth. Gastrointestinal bleeding may also occur. Joint bleeding in BV is less common than in hemophilia and usually occurs in patients with low levels of factor VIII in the blood.
Hemophilia
Since the inheritance principle of hemophilia A (factor VIII deficiency) and hemophilia B (factor IX deficiency) is a sex-linked recessive trait, women extremely rarely suffer from these diseases. It is more possible, but unproven, that bleeding occurs in female carriers of hemophilia A or B. A symptomatic carrier with low levels of factor VIII or IX may experience increased bleeding in the same way as a patient with mild hemophilia during surgery or trauma. In women, however, abnormal periods may be the only symptom. Irregular, heavy or prolonged menstrual periods are the most common symptoms among carriers of the hemophilia A and B genes. Excessive bleeding associated with pregnancy and childbirth can also occur in cases where factor levels are below 30%. Female carriers whose factor level allows them to be classified as having a mild form of hemophilia require the same treatment for bleeding as men with a mild form of hemophilia. Clinically there is no difference.
Mixed diseases
Deficiency of any of the blood clotting proteins (factors) may indicate signs of varying degrees of severity as well as quantitative and qualitative platelet defects. Most symptoms of such defects will resemble those of von Willebrand disease. Some diseases associated with deficiency of blood clotting factors are quite mild (for example, factor XII deficiency). Others, such as hypofibrinogenemia (deficiency of the clotting factor fibrinogen) are particularly problematic. Many of these diseases are inherited autosomalally by women and men equally.
Gynecological symptoms observed in women with increased bleeding
Menorrhagia/metrorrhagia
Prolonged and heavy menstrual bleeding is the most common hemorrhagic symptom observed in women with bleeding problems. Some suffer from excessive bleeding during the menstrual cycle (menorrhagia); others experience similar problems immediately after the end of the menstrual cycle (metrorrhagia). The uterus is a highly vascular organ capable of losing large amounts of blood over a short period of time. Prolonged bleeding can cause iron deficiency anemia. Therapeutic interventions such as dilatation and curettage of the walls of the uterine cavity usually only worsen the situation, since the alignment of the lining tissues of the uterus prevents the formation of a fibrin clot, the uterine cavity remains unprotected and the resumption of hemostasis is complicated.
Dysmenorrhea and mid-cycle pain
Another common complaint among women with excessive bleeding is pain during menstrual periods and mid-cycle pain. One can only speculate about their reasons, since no reliable scientific data on this issue exists. Some women may experience pain as a result of heavy bleeding and incomplete formation of clots in the uterus. In other cases, there is pain in the pelvis or abdomen, which occurs with endometriosis. Endometriosis is an abnormal condition in which the growth of endometrial tissue occurs in the abdominal cavity outside the uterus. When any woman is on her menstrual period, the intrauterine tissue - wherever it is - will bleed. If a woman has a bleeding disorder and endometriosis, tissue outside the uterus may bleed, causing peritoneal irritation (irritation of the peritoneum) and pain.
I have spoken with women who experience excessive bleeding during ovulation and experience severe pelvic pain. When the egg is released from the ovary, healthy women experience very little bleeding. But in women with bleeding disorders, this can be a significant problem. I once met a woman with von Willebrand disease type 3 whose bleeding during ovulation was so intense that she had to take birth control pills for the rest of her life to avoid ovulation.
Conception/fertility problems
Many women with bleeding problems use birth control pills or other hormone therapy. Obviously, this affects a woman's ability to conceive. The long-term effect of such long-term hormonal therapy is not known. It is also unknown whether von Willebrand factor deficiency has any effect on the ability of a fertilized egg to attach to the uterine wall, which in turn may affect the ability to carry a fetus to term. It seems casuistic that there is a higher likelihood of miscarriage in women with BV than in the general case. This may be simply because when a miscarriage occurs, the subsequent excessive bleeding forces the woman to seek medical attention and her diagnosis is noted. At the same time, a miscarriage that occurs in the early stages of pregnancy in an ordinary woman may not even be perceived as such. The bleeding that follows spontaneous termination of pregnancy can be quite significant, since the high level of clotting factors naturally maintained in the blood during pregnancy decreases sharply after the loss of the fetus. Postpartum bleeding can be a problem for women with bleeding disorders. Depending on the disease, problems may be small or very minor because hormones that rise during pregnancy cause clotting factors to increase. This is especially true for factors VIII and von Willebrand. However, even if there are no complications immediately after birth, postpartum hemorrhage may occur a few days later, when hormone levels and levels of clotting factors begin to decline. Patients with von Willebrand disease have a greater number of primary (immediate) and secondary (delayed) postpartum hemorrhages. In women who breastfeed, hormone levels remain high, but it is not known whether this protects against postpartum hemorrhage. Pregnancy does not provide any protection to women with VWD type 2, since hormonal increases and increases in von Willebrand factor do not alter the functional impairment of vWF. Factor IX levels do not increase during pregnancy.
Diagnosis of hereditary diseases that cause increased bleeding
For non-hematology physicians, including obstetricians-gynecologists and family physicians, diagnosing a bleeding disorder can be challenging at best. First responders typically rely on prothrombin time (PT) and activated partial thromboplastin time (aPTT) tests and, to a lesser extent, clotting-bleeding time to make a diagnosis. The difficulty with this is that the most common bleeding disorder in women, von Willebrand disease, cannot be detected using these tests.
In von Willebrand disease, there are no changes in PT, and the aPTT is only occasionally prolonged. Increased PT occurs only with a deficiency of factors X, VII, V, II, I, or with certain liver diseases. The aPTT is prolonged only when the patient has a deficiency of factors XII, XI, X, IX, VIII, V, II or I. The aPTT in von Willebrand disease is prolonged only if the level of factor VIII is below 40%. For patients with qualitative type 2 VWD (except 2N), the aPTT will usually be normal. Bleeding time can be normal or prolonged. Bleeding time testing is not very accurate. This is a superficial test to assess platelet function and can be affected by various external factors, such as a cold. VWF testing should include a ristocytin cofactor test, which assesses the function of VWF, the antigen to VWF, which measures vWF levels and factor VIII levels. Many doctors also use the test to evaluate the binding capacity of vWF collagen. Additional tests, such as the vWF multimer assay, are used to study protein structure, which is especially useful in studying the different subtypes of von Willebrand disease type 2. There is no perfect test for diagnosing VWD.
Laboratory tests to determine the presence of BV are often negative or inconclusive and may require repeat testing for confirmation. People with BV may have cyclical variations in their levels, making diagnosis difficult, especially in its milder forms. The timing of the test is important. It is better to test a woman during her menstrual cycle, when hormonal and factor norms are at their lowest. When performing a coagulation test, it is important for the examiner to consider any environmental factors or medications that may affect the accuracy of the test. Hormonal therapy such as oral contraceptives, due to their stimulating effect on vWF and factor VIII, should be interrupted before testing. The use of certain drugs that have contraindications that affect platelet function should also be discontinued. This is aspirin and most non-steroidal anti-inflammatory drugs (NSAIDs) such as ibuprofen, diclofenac, Voltaren, Celebrex, etc. Because of a number of reasons that can affect the accuracy of the result and normal fluctuations in factor levels, it is necessary to repeat tests in women with a history of bleeding, even if the test results are normal at the time. It is also necessary to refer the woman to hematologists with experience in treating bleeding disorders.
These hematologists are typically affiliated with treatment centers throughout the United States and around the world. Special tests necessary to establish a diagnosis usually require the use of specialized equipment, reagents and technology. Laboratory errors in the assessment of coagulation problems are common among non-specialized laboratories. Very few of the women I interviewed were diagnosed without repeated testing. This is a huge waste of time and money.
Treatment of gynecological complications in women with increased bleeding
The various treatments described below have been successful in the women I interviewed. This list is not final. You should consult your doctor to determine the appropriate method for your particular case.
Hormone therapy
Oral contraceptives (OCs) are very effective in increasing levels of factors II, VIII, and von Willebrand factor. For this reason, they are especially useful in treating heavy menstrual periods as well as other bleeding in women. Women often report that during their menstrual period and taking placebo pills (pacifiers), they also have an increase in the number of strokes and nosebleeds, which decrease once they take the contraceptives again. For symptomatic carriers (factor VIII), OC may be the only possible treatment option. For women with qualitative VWF defects, the effectiveness of oral contraceptives is reduced because the hormones increase VWF levels but do not correct the inherent structural defects. For these women, OCs probably have some success in helping regulate their menstrual periods and reduce bleeding, but other treatments may also be necessary. For bleeding not sensitive to OCs, the use of pure progestin components, such as Norulat and Provera, can be very useful because they cause thickening of the lining uterine tissue (secretory myometrium) and stop bleeding. Question: How long can you stop menstruating? Some doctors prefer the use of progesterone components such as Depo-Provera for intramuscular administration, although the results, according to surveys of women, vary. Progesterone components when deposited intramuscularly are unsafe for a number of reasons:
1. They require an intramuscular injection, which is not recommended for people with bleeding problems. 2. If side effects occur in some patients during administration, they may last for several months, whereas the half-life for oral contraceptives is much shorter. 3. Dosage can be better managed with the assistance of a specialist. Strictly speaking, in case of life-threatening bleeding, the use of intravenous combined estrogens (Premarin) is very effective.
Desmopressin acetate
This medication is usually administered by injection (intravenously or subcutaneously - DDAVP) and intranasally (nasal drops - Stimate). It is chemically related to antidiuretic hormone (vasopressin). When used, DDAVP causes a dramatic increase in circulating plasma factor VIII and von Willebrand factor, stimulating the production of these proteins from blood vessel walls. This drug is very effective in treating bleeding in women with type 1 BV and symptomatic carriers of hemophilia A with factor VIII deficiency. It is less effective for women with type 2 VWD because it does not correct the molecular defects in von Willebrand factor. The drug is ineffective in VWD type 3, where little or no VWF is produced, and should not be used in type 2B due to excessive platelet binding and subsequent thrombocytopenia. (Thrombocytopenia is a condition characterized by a decrease in the number of platelets and, accordingly, an increase in bleeding). Unfortunately, DDAVP does not provide any benefit to female symptomatic carriers of hemophilia B because it has no effect on factor IX. When a "strong" spray (Stimate) is prescribed, doctors do so because there is a less concentrated formulation of intranasal desmopressin called DDAVP used to treat nocturnal enuresis. This less concentrated form of the drug is correspondingly ineffective for patients with increased bleeding.
Plasma preparations
Women with increased bleeding who are not sensitive to desmopressin or active hormonal therapy are indicated for replacement therapy for clotting factor deficiency or defectiveness. Today, with the advent of more reliable, virus-inactivated lyophilized plasma preparations (factor concentrates) in many countries, the use of preparations such as cryoprecipitate or fresh frozen plasma is unacceptable. The US National Hemophilia Organization and Scientific Advisory Board recommend against their use if virus-inactivated drugs are available. In the United States and other countries where safe and hemostatically effective drugs are available for the treatment of bleeding associated with disorders of factors II, VII, VIII, IX, X, and von Willebrand factor. In the United States, the two most widely used drugs for treating von Willebrand disease are Humate-P (Haemate-P in other countries) and Alphanate SD. Both of these drugs are concentrates with high levels of factor VIII and von Willebrand factor. Monoclonal or recombinant factor VIII preparations should not be used for VWD because they do not contain von Willebrand factor.
Antifibrinolytics
Drugs such as aminocaproic acid may be useful in treating menstrual bleeding, as well as bleeding from the mucous membranes of the nose and mouth. These medications do not form a clot, they simply keep the clot in place longer by blocking the enzymes responsible for fibrinolysis (the spontaneous, normal process of breaking up a clot once it has formed). These drugs should not be used for joint and kidney bleeding.
NSAIDs and analgesics
Most NSAIDs tend to interfere with platelet function. They interfere with platelet adhesion and aggregation (platelets become unable to join to form a clot). Data exist to show that two anti-inflammatory drugs, choline-magnesium-trisalicylate (Tri-lisate) and salsalate (Disalcid), do not alter platelet function and may therefore be useful for use in individuals with bleeding disorders. These medications are often useful for managing pain associated with ovulation and menstruation. A new class of NSAIDs, Cox-2 inhibitors (Celebrex), do not cause platelet dysfunction and may be useful for people with bleeding problems.
Surgical issues
Intrauterine ablation
In women who do not respond to other treatments, the uterine lining may need to be removed to prevent menstruation, although this will render it sterile. This may serve as a safe alternative to hysterectomy for bleeding problems. There is scientific evidence in the literature supporting the safety and effectiveness of this procedure for women with a range of bleeding problems.
Hysterotomy
For some women who are minimally responsive or completely resistant to other therapies, hysterotomy may be the only acceptable treatment. Vaginal or transabdominal hysterectomies have been safely performed in women with bleeding problems after adequate and appropriate plasma factor concentrations have been achieved.
Laparoscopy
In women experiencing pain due to endometriosis (bleeding from endometrial tissue growing outside the uterine cavity), removal of migrating tissue using a laparoscopic technique can be effective. In this procedure, two small incisions are made in the abdomen. A special probe for visual manipulation is guided by the surgeon through one of the incisions, while the tissue is removed through the second incision.
Dilatation and curettage of the uterine cavity
These procedures entail relaxing and sufficiently dilating the cervix and scraping the endometrium. The use of these procedures with the intention of reducing the intensity of bleeding cannot be effective for women with bleeding, since this technique prevents thrombus formation on damaged vessels of the subendometrial location. Also, if dilatation and curettage of the uterine cavity are not performed for diagnostic purposes, this is unacceptable in cases with patients with increased bleeding.
Ovariectomy
Ovariectomy (removal of the ovaries) may be an acceptable option for women who experience bleeding during ovulation and who, for one reason or another, cannot benefit from hormone therapy. However, this procedure not only makes the woman sterile, but also stimulates menopause. It is imperative that women considering any of these options fully understand the risks, benefits, and alternatives before making a definite decision.
Conclusion
I hope that this article will be useful for women and practitioners looking for answers to some of the questions that arise in patients with problems with increased bleeding. I also hope the article will raise many questions that the medical and scientific communities will try to find answers to. The time has come to join forces to solve these problems.
additional literature
1. "Females Bleed Too." HANDI Quarterly (Fall 1993).
2. "Symptomatic Carriers." HANDI Quarterly (Fall 1994).
3. Medical and Scientific Advisory Council "Recommendations Regarding Women With Bleeding Disorders." Medical Advisory #303 (1997), National Hemophilia Foundation.
4. Medical and Scientific Advisory Council “Treatment of von Willebrand Disease.” Medical Advisory #314 (1998), National Hemophilia Foundation
5. Bottini, E., et al. “Prevention of Hemoperitoneum during Ovulation by Oral Contraceptives in Women with Type III von Willebrand Disease and Afibrinogenemia. Case Reports." Haemoatologica 76 (1991): 431-33.
6. Brenner, P.F., Ed., “Management of Bleeding Disorders in Women, The Role of the Obstetrician/Gynecologist.” American Journal of Obstetrics and Gynecology. (1996): Suppl. 175(3) Part 2. 761-792.
7. Bunschoten, EP, et al. "Bleeding Symptoms in Carriers of Hemophilia A and B." Thrombosis and Hemostasis (Germany) 59, no. 3 (1988): 349-352.
8. Caldwell, David, et. al. "Hereditary Coagulopothies in Pregnancy." Clinical Obstetrics and Gynecology 28, no. 1 (March 1985).
9. Conti, M., et al. "Pregnancy in Women with Different Types of von Willebrand Disease." Obstetrics and Gynecology 68 (1986): 282.
10. Cohen, S., et al. "Epidural Analgesia for Labor and Delivery in a Patient with von Willebrand Disease." Regional Anesthesia 14 (1989): 95-97.
11. Ewenstein, B. “von Willebrand's Disease.” Annual Reviews in Medicine 48 (1997): 525-42
12. Kouides, P “Females with von Willebrand disease: 72 years as the silent majority.” Haemophilia 4 (1998): 665-676
13. Lee, CA "Women and von Willebrand disease." Haemophilia 5 (1999): Suppl. 2. 38-45
14. Murray E. and Lilicrap, D. “von Willebrand Disease: Pathogenesis, Classification, and Management.” Transfusion Medicine Reviews Vol. X, no 2 (1996): 93-110
15. Paper, R., Baker J and Larson K. “Women Can Have Bleeding Disorders.” Slide presentation. National Hemophilia Foundation. 1999
16. Robertson, L. E., et al. "Hereditary Factor VII Deficiency in Pregnancy: Peripartum Treatment with Factor VII Concentrate." American Journal of Hematology 40 (1992): 38-41.
17. Scott, J. P., and R. Montgomery. "Therapy of von Willebrand Disease." Seminars in Thrombosis and Hemostasis 19, no. 1 (1993).
18. Vosburgh, E. “Rational Intervention in von Willebrand Disease.” Hospital Practice (March 1993).
Prevention
The best prevention is to closely monitor your menstrual cycle. Control of the amount of blood released and the duration of discharge. Availability of a calendar with signs of the beginning and end of menarche.
Preventive examination in a gynecological chair once a year. Regular examination will allow you to monitor women's health and identify signs of ailments in the body.
Openness in conversation with the doctor. Do not hesitate to tell your gynecologist about your subjective feelings, even if they seem stupid and frivolous.
Regular (once a year) detailed blood tests to identify abnormalities in the body.
Attention to your body: if you have any unknown bruises or discomfort, be sure to make an appointment with a specialist.
A rational regimen for taking oral contraceptives and other drugs that contribute to the development of menorrhagia.
Menorrhagia is a female disease that women themselves often do not notice due to the subjectivity of judgment and the difficulty of assessing blood loss at home. Uterine bleeding coincides in time with true menstruation, but exceeds the permissible blood loss, or the period of menarche itself is prolonged. Menorrhagia is common in both teenage girls and mature women. This may be a variant of the norm or indicate problems of a different nature. In modern conditions, menorrhagia is easily treatable; all you need to do is make an appointment with a good specialist.
Complications of menorrhagia
Menorrhagia is often not diagnosed on time, while potential complications can occur at any time and ruin a woman's social and emotional life. The main complications include:
- Anemic syndrome. Develops due to excess blood loss and decreased hemoglobin concentration. General health worsens, chronic fatigue and pale skin appear. Hair may fall out.
- Acute blood loss syndrome. The amount of blood released becomes too large, the volume of circulating blood drops to a critically low level, which is a threat to life.
- Very rarely, death due to multiple organ failure due to anemic syndrome or a blood clotting disorder with chronic abnormal uterine bleeding that occurs on a regular basis.