Delicate and complex problem
Coccyx cyst (epithelial coccygeal duct) is one of the most delicate and complex health problems.
Those who have dealt with her understand what we are talking about. Coccyx cyst occurs in both men and women. According to statistics, the stronger sex suffers three times more often. The delicacy lies in the localization of the pathological focus. The formation is located in a fairly intimate place (the area of the coccyx, sacrum and intergluteal fold) not far from the anus. Not everyone will easily want to share this with others, even with relatives and loved ones. Not everyone is ready to immediately show the sore spot, discuss their complaints and discomfort, even with doctors. When an epithelial cyst of the coccyx becomes complicated (abscess formation, suppuration, relapse), a person in most cases is deprived of the opportunity to maintain his usual lifestyle and quality of life. Irritating pain, excruciating discomfort, serous or purulent discharge, an unpleasant odor appear, laundry gets dirty, and additional hygiene procedures become necessary. Often it is simply impossible to sit normally. And this is not the whole list of inconveniences.
Many in this situation are forced to give up their usual activities, sports, and even intimate life. All this is depressing. Adding to the delicacy is that a coccyx cyst clinically manifests itself more often in adolescence or puberty. Teenagers are known to be especially sensitive to such problems, although they will try their best not to show it. Wise advice, understanding, help and timely consultation from a surgeon are especially important for them.
The complexity of this pathology lies in the fact that very often there are relapses (repeats) after improper preparation for surgery, an insufficiently radical operation (incomplete removal of cysts, fistulas and leaks), inattentive management in the postoperative period, failure to follow doctor’s recommendations, ignoring basic hygienic procedures and other reasons. Some people have to undergo surgery for coccyx cysts not once, not twice, but multiple times. You won’t believe it, but there are still people who suffer all their lives due to relapses. This reduces the quality of life and is certainly a tragedy. It shouldn't be like this!!!
It is necessary to initially take this disease and the initial operation very seriously. Agree, no one wants to have multiple surgeries. However, repeated surgical intervention should be taken no less seriously, and perhaps more seriously, if the clinical situation has recurred. It is very important to prevent chronicity and continuation of the sluggish process. A coccyx cyst is not a very common and not at all an ordinary problem. The choice of clinic and doctor is extremely important to minimize the risk of relapse. Consultation and surgery with a qualified surgeon who has experience in treating this pathology is necessary.
How to Diagnose an Injury
To understand whether a patient has damage, a doctor can use several simple diagnostic methods:
- Visual inspection. There will be severe swelling at the site of injury, and some will develop a hematoma. Upon palpation, a person feels a twinge of pain.
- Radiography. It is done in frontal and lateral projections. Finding signs of a coccyx fracture using this technique is quite difficult.
- CT scan. Helps to accurately determine the current condition of bones, find confusion and cracks.
- MRI. The magnetic resonance imaging method shows not only the condition of the bones, but also the space surrounding them - blood vessels and muscles. It is this kind of examination that helps to “look” into a person’s tissues and understand whether everything is in order with his nerve fibers.
Previously, when assessing the condition of patients, the method of rectal or vaginal examination was also used. Now it is not used unless absolutely necessary, because it is associated with great discomfort for the patient.
Coccyx cyst. What is this? What is the reason? Classification
Coccyx cyst (epithelial coccygeal duct, pilonidal cyst, ECC) is a closed small cavity (tube-shaped canal), which is located subcutaneously in the area of the upper part of the intergluteal fold. It does not have a direct connection with the coccyx and sacrum. The inside of the cyst cavity is covered with a special epithelial lining, which contains ordinary hair follicles, hair, sweat and sebaceous glands.
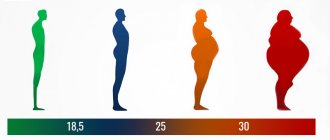
According to the main generally accepted version, a coccyx cyst is a type of congenital pathology. An unusual defect (anomaly) in the area of the intergluteal fold is formed in the prenatal period. As a result, a person has a cavity (canal or passage) with a special internal epithelial lining under the skin in the upper part of the intergluteal fold in the coccyx area. According to another version, a cyst (epithelial tract) is formed as a result of hair ingrowth into the skin due to improper inward growth with intussusception (immersion). The appearance of the formation is often associated with injury to the sacrococcygeal region or prolonged sitting (professional drivers often suffer). The cause of suppuration is most often the addition of a specific infection (present in the anus).
In childhood, a coccygeal cyst practically does not make itself felt, since there is no infection in the formation cavity, there is no active hair growth and gland secretion. Clinical manifestations of the disease usually occur between 13 and 30 years of age. As a rule, during these years of life there is increased hair growth, active secretion of sweat and sebaceous glands, including inside the cyst. The hair in the cyst grows, and the glands secrete their secretions inside the formation. It all adds up.
When the cavity becomes full, unpleasant discomfort appears, excruciating pain, weeping, itching and other symptoms may appear. Then one or more primary serous holes (serous fistulas) open between the buttocks in the coccyx area. The contents of the formation (serous discharge, tufts of hair) are released. When holes appear, microorganisms actively colonize the cavity (infection) in which they were not previously present. If for some reason the connection with the external environment is closed, there is a delay in the evacuation (removal) of the discharge from the formation. Overflow, tension, acute inflammation and abscess formation (suppuration) occur.
It so happens that this pathology has many different names. This can sometimes be confusing or misleading. If there is no inflammation, the formation is called an uncomplicated coccyx cyst, dermoid cyst, or epithelial coccygeal duct. In the English literature, a pilonidal cyst or pilonidal sinus (pilonidal cyst, pylonidal sinus, hairy or hairy cyst, “hair nest”) is more common due to the presence of hair inside. Holes or holes that occur primarily or secondary are called fistulas in the coccyx region. When acute inflammation and exacerbation of chronic inflammation occurs, suppuration occurs and abscess formation, the diagnosis sounds like an abscess, a festering coccyx cyst or a festering epithelial coccygeal tract. All these names describe different stages or features of the same process.
However, the following classification is most often used in clinical practice:
- Coccyx cyst uncomplicated by inflammation (without clinical manifestations)
- Acute or exacerbation of chronic inflammation of the coccyx cyst
- Chronic inflammation (sluggish process) of coccyx cysts
- Remission of the inflammatory process (cold period)
Interesting facts about the bird
- The bird feels good in captivity. The falcon can be kept in a spacious cage. In such conditions, the bird is able to reproduce and get used to purchased feed.
- The birds are trained to hunt pigeons and sparrows.
- The voice of the winged creature sounds like a high and squeaky “ki-ki”. Individuals near the nest are especially noisy.
- The bird got its name from the ancient Russian word “kobets”, which means “small hunting falcon”.
- Often, sharpwings can be found in pastures with farm animals. Birds accompany livestock, snatching insects flying around.
- In captivity, birds can eat not only raw beef or chicken, but also store-bought ham.
- Despite their miniature size, falcons are ready to mate with a heron.
- Birds benefit humanity by eliminating pests in agricultural fields. They also drive away other birds that might eat crops.
- Previously, people clipped the wings of falcons in order to tame them and curb their passion for flying.
- The majority of birds are females, which leads to gender imbalance.
Basic preventive measures:
- Observe all rules of personal and intimate hygiene
- Rinse the intergluteal fold
- Wear loose, clean, eco-friendly clothing (avoid tight, tight, synthetic clothing)
- Avoid trauma to the coccyx area
- Avoid prolonged sitting
- Epilation and/or depilation in the tailbone area
- Promptly treat and sanitize primary holes, wounds and microtraumas in the coccyx area.
- Immediately contact a surgeon if the first signs of discomfort and inflammation appear
If clinical manifestations or relapse appear, then the only correct preventive measure will be surgical treatment.
What worries you about a coccyx cyst? Symptoms
If the coccyx cyst is not complicated or is in the “cold period” after inflammation, then in the vast majority of cases it does not manifest itself and is asymptomatic. From time to time there may be some discomfort in the coccyx area, serous discharge or moisture above and between the buttocks. Sometimes anal itching can be disturbing. Small points (retractions) of the skin in the area of the coccyx and intergluteal fold are visually determined.
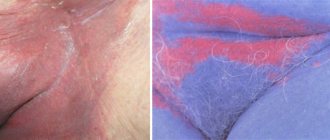
When an infection enters the cavity, discomfort increases significantly, inflammation and pain occur in the area of the coccyx and sacrum. Primary openings (holes, fistulas) may appear from which serous, sanguineous or purulent discharge is released. With suppuration and abscess formation, secondary purulent fistulas can form.
In the absence or delay of discharge from the cyst, a painful infiltrate (swelling, edema, tumor, lump) appears through the holes with clear contours in the area of the coccyx and intergluteal fold, which interferes with movements and walking. When the contents of the cyst become infected, acute inflammation develops. Pain, swelling, and redness appear in the area of infiltration. Increased body temperature (fever). Abscess formation occurs (formation of a cavity with suppuration).
After the abscess of the coccyx cyst is drained independently or as a result of surgery (outflow of pus), relief occurs. Pain, swelling and redness disappear, inflammation subsides. The fistula gradually closes, and the postoperative incision wound heals. A period of imaginary well-being begins (the cold period). There is no point in waiting for a complete cure, since there remains a focus of dormant chronic infection (the substrate of chronic inflammation), which becomes aggravated or becomes re-inflamed under certain favorable conditions.
If radical surgery is not performed, then periods of exacerbations and remissions (the interval between exacerbations) can alternate for months and sometimes years. During remission, there is usually no edema or hyperemia. Periodic dull pain or discomfort in the tailbone area may be bothersome. Inconvenience occurs when sitting and in the presence of scanty discharge from holes or fistulas. Fistulas can function, open and close. With prolonged remission, pigmentation and scar tissue changes appear around the holes.
Anatomy of the sacrum in humans
The sacrum is a triangular-shaped bone located at the base of the spinal column (lumbosacral region).
Structure and muscular system
The sacrum consists of five sacral vertebrae fused together. The function and anatomy of this bone may vary depending on age. So, up to 25 years, the sacrum consists of separate vertebrae with cartilage, and after 25 it is a solid bone. Such fusion ensures withstanding and distribution of loads.
The structure of the human sacrum
The existence of the sacral region is impossible to imagine without the following muscles:
- Pear-shaped . The origin of the piriformis muscle is the ligamentous apparatus, the sacrum, and the greater sciatic foramen. From here, bundles of muscle fibers depart, which subsequently connect and go towards the greater trochanter of the femur. The task of the piriformis muscle is to provide rotational movements of the hip joint.
- Ileum . The iliacus muscle originates from the bone and ends in the area of the lesser trochanter of the femur. The task of this muscle is to provide flexion of the lower limb.
- Multipartite . Multifidus muscle fibers are located in the grooves of the sacrum and are involved in bending the back backward.
- Gluteal . The gluteal muscle fibers begin at the sacrum and coccyx and extend to the gluteal tuberosity. The gluteal muscle is the largest in the sacral region. It is responsible for rotation and flexion of the lower extremities.
Functions
The sacrum performs several important functions:
- protects internal organs located in the pelvic cavity;
- helps the skeleton maintain an upright position;
- is responsible for uniform load distribution.
Note! The vertebrae of the sacrum are immobile, so it is not capable of performing motor functions.
Video: “Structure of the sacrum”
Treatment of coccyx cyst (preoperative examination, preparation, operations)
Treatment of coccyx cyst is surgical.
To clarify the diagnosis and exclude other pathologies (rectal fistulas, presacral teratoma, osteomyelitis), an examination of the rectum is necessary; in some cases, radiography, colonoscopy or irrigoscopy may be required. Before surgery, thorough depilation of the surgical field is very important and cleansing enemas are required. In case of abscess of a coccyx cyst (festering epithelial coccygeal duct), acute inflammatory phenomena or exacerbation of a chronic process, the first stage is to drain the purulent contents of the cyst (open, drain). The abscess is opened urgently with a small incision under local anesthesia. The cavity is emptied, sanitized with antiseptic solutions and drained. After the drainage of pus, relief occurs. Bandages with water-soluble ointments (levomekol) are applied. The pain goes away, the inflammation subsides, and the postoperative incision wound heals. A period of imaginary well-being begins (full recovery does not occur). A focus of dormant chronic infection remains. Without the second stage - radical surgery (complete excision or removal of the coccyx cyst), as a rule, suppuration is repeated again and again. With a long delay of radical intervention, inflammation can become chronic with the formation of new infiltrates and secondary fistulas.
Primary radical surgery (uncomplicated coccyx cyst) or the second stage of treatment after the subsidence of acute inflammatory phenomena during the period of remission (“cold period”) is carried out as planned. The operation is performed under local infiltration, spinal anesthesia or intravenous anesthesia. Surgical intervention consists of removing (excision) the pathological formation (cyst, canal, tract) along with the internal lining, the contents of the cavity, the surrounding tissues that have changed after repeated inflammatory processes to the fascia. All primary and secondary holes (holes, fistulas) are also excised. To minimize the risk of relapse, all passages and fistulas must be painted with a special dye. After excision of the coccyx cyst, the postoperative wound is usually sutured tightly. Donati sutures are applied to ensure good bleeding control and accurate alignment of the wound edges.
In a number of clinics, the postoperative wound is left open or the edges of the wound are sutured to its bottom for secondary healing (marsupilization). In our opinion, this tactic of postoperative wound management has many disadvantages:
- traumatic
- decrease in the patient's quality of life
- possible secondary infection
- high probability of relapse
- vicious postoperative scars after secondary healing
Postoperative period. Dressings after surgery
In the postoperative period, bed rest must be observed during the first day after surgery.
You can get up and walk the day after surgery. You can sit down on days 5-6-7. Fully sit for 8-9 days. It is very important to avoid stress on the seams. It is necessary to avoid traumatizing the postoperative wound, and subsequently the scar. In the postoperative period, antibacterial therapy is prescribed if the process was accompanied by acute inflammation and abscess formation. Painkillers are used in the presence of pain. A modern breathable aseptic dressing with an absorbent pad is applied to the sutures. Dressings are done daily. On days 4-5, if there is no discharge from the wound, you can bandage it every other day. During primary healing, the sutures are removed 12-14 days after surgery. If the postoperative wound is treated openly, then secondary healing takes a fairly long period. In such a situation, it is best to use modern medical dressings and fixation means for dressing and care. In the postoperative period, the patient's quality of life should not suffer. We can select special dressings to care for an open wound, even if you had surgery in another clinic.
Features and differences in the structure of the sacrum and coccyx in women and men
In women, the sacrum is wider, shorter and less curved than in the stronger sex. At the same time, this structure is more mobile: ligaments allow it to deviate by an angle from 8 to 14 degrees. Actually, it is due to this that the female body is more flexible than the male one.
There are also differences in the structure of the coccyx. The female pelvis is shorter and wider, adapted to labor. The size of the hole also differs: in women it is large enough for the baby’s body to pass through it.
It is noteworthy that this hole, thanks to the movable coccyx, increases during labor . As for men, their tailbone is less mobile and therefore less susceptible to bruises and injuries.
Video: “Structure of the spine”
Complications and consequences
If the process is severe, the following complications may develop:
- relapse
- coccyx osteomyelitis (purulent bone lesion)
- fistulous pyoderma (purulent skin lesion)
- fungal infection
- multiple communicating purulent fistulas and pathological tracts with epithelial lining (sacrococcygeal region, perineum, scrotum, inguinal folds, anterior abdominal wall, anus)
Complications require painstaking, lengthy, often multi-stage treatment. Competent prevention, the right choice of clinic and doctor, timely treatment, radical surgery, and compliance with all recommendations will help you avoid such problems.