Structural features
The structure of the urethra, which is called the urethra, differs according to a particular gender:
- In women, the urethra is short - 3-4 cm and wide - 1-1.5 cm.
- In men, the urethra is long – up to 30 cm and narrow – up to 8 mm. In addition, it has curves.
The anatomical features of the structure of the organ are the reason why women often develop cystitis. This is explained by the fact that the infection quickly penetrates the bladder through the short urethra and causes inflammation. In men, the urethra is connected to the vas deferens, so the secretion of the sex glands is also excreted through the urethra.
The inner surface of the urethra is covered with mucous membrane. When it becomes inflamed, which can be caused by various reasons, urethritis develops. In women, this pathology does not lead to disruption of the outflow of urine, which eliminates the occurrence of severe discomfort and speeds up treatment of the disease. Due to the anatomical features, the infection in the male urethra lingers for a long time, causing severe swelling of the mucous membrane. This leads to disruption of the outflow of urine, and in severe cases to painful retention of urination.
Postcoital cystitis in women symptoms
The problem arises some time (usually 1-3 years) after the onset of sexual activity due to the formation of urethro-hymenal adhesions, that is, fusion of the remnants of the hymen with the external opening of the urethra. In some cases, postcoital cystitis occurs after childbirth, accompanied by ruptures followed by the formation of adhesions.
The manifestations of postcoital cystitis are no different from banal acute cystitis, with the only difference being that they occur several hours (usually about a day) after each sexual intercourse.
The problem of postcoital cystitis is, in essence, the problem of the impossibility of normal sexual life. Indeed, no sexual intercourse means no problem of postcoital cystitis! However, looking at the young and sexually active women who come to me with this problem, you understand the tragedy and insidiousness of this disease!
There are simple and ineffective “folk” remedies for preventing postcoital cystitis, for example, urinating before and after sexual intercourse (obviously, drinking a lot of water beforehand). There are also more complex, but equally ridiculous methods, such as taking prophylactic antibiotics with every sexual intercourse (and at the same time, not a drop of alcohol and chronic dysbiosis).
Causes of inflammation
Understanding what the urethra is in women and men, one can understand how inflammatory processes occur in the organ. It can be caused by infectious and non-infectious factors.
Non-infectious urethritis often occurs with the development of urolithiasis. In this case, small stones move with the urine current, which can damage the mucous membrane of the urethra, which causes inflammation. Also the cause of the development of non-infectious urethritis are:
- Injuries. They most often occur during cystoscopy and catheterization.
- Tumors. Malignant neoplasms always cause inflammation of the mucous membrane.
- Allergy. Negative body reactions can be caused by negative reactions of the body to certain foods or substances.
Inflammatory processes in men can occur when the urethra is narrowed due to prostatitis or benign prostatic hyperplasia. In such cases, urinary stagnation occurs.
Non-infectious urethritis must be treated in the early stages of development. To do this, on the recommendation of a doctor, you should buy the necessary medications at the pharmacy to relieve inflammation. If therapy is not carried out quickly, infection may occur and complications may arise.
Infectious urethritis can be caused by various pathogens. Before treating the disease, it is necessary to conduct research aimed at determining the type of pathogen. Nowadays you can buy various medications in pharmacies that will quickly overcome the most severe infection. But at the same time, it is necessary to urgently take the required measures. The infection that causes the development of urethritis can enter the body sexually or hematogenously.
Causes of stricture urethral disease
There are four main reasons for the development of the disease:
- Iatrogenic (after medical interventions).
- Traumatic.
- Idiopathic.
- Inflammatory.
The leading causes of the formation of iatrogenic urethral strictures are transurethral interventions, including injuries during urethral catheterization. Complications after radiation or brachytherapy; bougienage of the urethra, prostatectomy, penile replacement, treatment of hypospodia. In women, urethral strictures can occur after birth trauma or hysterectomy.
The development of post-traumatic urethral strictures is usually associated with blunt trauma to the perineum, penetrating wounds of the urethra, foreign bodies in the urethra, fractures of the pelvic bones (road accident, fall from a height, etc.), chemical and thermal damage to the urethra.
Idiopathic urethral strictures (of unclear etiology). The likely cause of the development of the disease, in this case, is a minor injury undetected in the past, for example, damage to the perineum while riding a bicycle, motorcycle or horse.
Urethral strictures of inflammatory origin can develop as a result of previous urethritis (with gonorrhea, chlamydia, tuberculosis, syphilis), balanitis and balanoposthitis, chronic degenerative-dystrophic processes (lichen sclerosus), etc. Twenty years ago, post-inflammatory urethral strictures were much more common than today time, which is associated with the active introduction of antibacterial drugs in medical practice and early diagnosis of certain infectious diseases. Also, the cause of urethral stricture can be diseases associated with deterioration of blood supply and metabolism of the tissues of the urethra - Leriche syndrome, etc.
Along the flow they distinguish:
- primary stricture (identified for the first time);
- recurrent (occurs again after treatment);
By localization:
- in the anterior urethra;
- in the posterior urethra;
By length:
- short (up to 2 cm);
- extended (over 2 cm).
Symptoms
At the initial stage of development, urethritis does not manifest itself with severe symptoms. Almost always, men experience slight discomfort in the penile canal, and women experience slight discomfort in the lower abdomen, slightly above the pubis. Such symptoms often go unnoticed.
As a rule, patients consult a doctor when the disease becomes acute. This is manifested by severe pain and burning when urinating. There is also a frequent urge to urinate, but the bladder cannot be emptied completely. In severe cases, the following symptoms are noted:
- Cloudy urine, possible inclusions of blood and mucus;
- Purulent discharge with an unpleasant odor.
In addition, a symptom of inflammation of the urethra is redness:
- In men, the external opening of the urethra.
- In women, the labia majora and minora.
What is the urethra?
According to its purpose, the urethra (urinary canal) is necessary for the body to remove urine accumulated in the bladder. In women, it is a tubular cavity connected to the bladder and has a relatively short size than in men.
The walls of the urethra are represented by three layers:
- the inside of the organ is covered with a mucous membrane;
- the middle part consists of muscle tissue;
- the outer layer has a connective structure.
The mucous membrane of the organ is represented by numerous folds.
Due to the anatomical features of the female urethra, it has the following parameters that are largely different from the male urethra:
- the length of the urethra is from 3 to 5 cm;
- when stretched, forms a wide diameter;
- there are narrowed areas along the entire length of the organ;
- When entering the bladder, the urethra expands.
The urethra in women and men has significant differences.
The location of the organ is in front of the anterior wall of the vagina and lies among the pelvic floor muscles. The external opening is located under the clitoris between the labia minora. At the exit of the urethra there is a slightly weakened muscle tone.
Fact. Full maturation of the urethra in girls occurs already at 12 weeks of pregnancy.
Functions of the urethra
The urethra, like other organs of the urinary system, performs important functions, which are as follows:
- removal of urine accumulated in the bladder;
- muscle tone of the organ allows you to create a reservoir and prevents spontaneous emptying;
- The urethral opening is considered an erogenous zone.
Important. The urethra is not a simple tube that acts as a conductor for urine to the outside. When various organ diseases develop, a woman may experience reflex disorders, which subsequently affect the intimate intimacy of a woman with a man.
Let's move a little away from the topic of what the urethra is in women and focus on the functions of the urethra in the male body. Thus, in addition to the urinary function, the organ performs another important role - the release of seminal fluid. Thus, the urethra in men is an integral part of reproductive activity.
Microflora
Microflora begins its development at the moment of human birth. Bacteria, when they get on the skin, penetrate inside and are distributed on the mucous membrane of organs, which creates a special microflora.
It is believed that the urethral mucosa contains:
- lactobacilli;
- epidermal and saprophytic staphylococci;
- peptostreptococci;
- bifidobacteria.
The combination of microorganisms living in the microflora of the urethra is called the Doderlein microflora.
Microorganisms that have penetrated inside and settled on the mucous membrane do not spread further to other organs and departments; this is prevented by urine accumulated in the bladder and internal secretions. The ciliated epithelium serves as an additional barrier.
Fact. The number of living microorganisms populating the mucous layer of the urethra in women is much greater than their number in men. This feature predominates in women due to the anatomical structure of the organ and its proximity to the rectum.
In the healthy microflora of the female urethra, 90% of microorganisms produce acid, which helps suppress the development of an alkaline environment, which results in the formation of inflammatory processes.
Urethral mucosa
The inside of the urethra is covered with a mucous layer, which in some areas has a flat structure and in others a high structure. It turns out that if you cut the urethra across, you can see the shape of a star. The largest and highest section of the mucosa is located on the posterior wall; it is called the ridge of the urinary canal.
The entire mucous membrane is covered with lacunae. In the lower parts of the urethra there are the so-called openings of the secretory glands. On both sides of the external exit of the organ there are opening tubules (ducts). The connective tissue of the urethra contains many elastic fibers and blood vessels.
Muscle
The muscle tissue of the organ has several layers:
- outer;
- circular;
- longitudinal;
- interior.
It consists of smooth muscles and elastic fibers. Joining the circular canal, the muscle tissue forms the lower urethral sphincter.
Diagnostics
In order to purchase effective medications in order to carry out effective treatment that will quickly restore the condition, you need to conduct a diagnosis. The general analysis of power is indicative. Elevated leukocytes in its results indicate the presence of an inflammatory process. Similar deviations from the norm are also observed during a general blood test.
To confirm the diagnosis, smears from the urethra are examined. Biomaterial is collected from the affected area using a special instrument. For the most effective antibacterial treatment, bacteriological urine culture is performed. With its help, the causative agent of the disease is determined. If a viral infection is suspected, a PCR test is additionally prescribed. Also, on the doctor’s recommendation, various instrumental examinations may be prescribed.
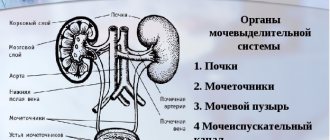
How is blood purified and urine formed?
Healthy kidneys filter about 100 ml of blood every minute, removing waste and extra water to eventually form urine.
There are three main stages of urine formation:
- filtration
- reabsorption
- secretion
In the process of purifying the blood, the kidneys retain all the necessary substances and selectively remove excess fluid and waste from the body.
- per day, the kidneys produce 140-180 liters of primary urine; in 24 hours, all circulating blood is cleansed several times; with age, these processes slow down
- the purification process takes place in small filter units known as nephrons.
- each kidney contains about a million nephrons, and each nephron consists of glomeruli and tubules.
- glomeruli are filters with very small pores, characteristic of selective filtration. Water and small substances are easily filtered through them. But larger red blood cells, white blood cells, platelets, protein, etc. cannot pass through these pores. Therefore, such cells are usually not visible in the urine of healthy people.
- The first stage of urine formation occurs in the glomeruli, where urine is filtered in an amount of 100-125 ml per minute, thus 140-180 liters of primary urine are formed in 24 hours. It contains not only industrial waste and toxic substances, but glucose and other useful substances.
- Each kidney performs the process of reabsorption (reabsorption). Of the fluid entering the tubules, 99% of the fluid is selectively reabsorbed and only the remaining 1% of the fluid is excreted as secondary urine. Thanks to this process, all the necessary substances are reabsorbed in the tubules, while 1-2 liters of fluid containing waste and other harmful substances are excreted from the body in the form of secondary urine.
Thus, the kidneys have filtration and concentration abilities.
Can there be a change in urine volume in a person with healthy kidneys?
YES. The amount of water consumed and atmospheric temperature are the main factors that determine the volume of urine that a normal person excretes.
Depending on the amount of fluid consumed, the amount of urine excreted changes: the more fluid enters the body, the more it is excreted and the less concentrated the urine, its color becomes light, even transparent. If the amount of fluid decreases, then the amount of urine excreted becomes less, it will be more concentrated, and the color will be dark straw.
During the summer months, sweating caused by high ambient temperatures causes urine volume to decrease. During the winter months the opposite is true - low temperatures, lack of sweating and more urine.
In a person with normal water intake, if the urine volume is less than 500 ml or more than 3000 ml, this may indicate that the kidneys need more attention and additional examination.
Make an appointment
Make an appointment with a gynecologist by calling 8(812)952-99-95 or filling out the online form - the administrator will contact you to confirm your appointment
guarantees complete confidentiality
Treatment
In most cases, treatment of urethritis does not require hospitalization. Therapy is carried out at home with medications recommended by the doctor. To monitor the dynamics of treatment, it is necessary to periodically visit the clinic during the treatment process.
If a bacterial infection is confirmed, therapy is carried out using antibacterial drugs. These can be pills, intramuscular or intravenous infections. Women can also use vaginal suppositories. When treating men, instillations may be prescribed. During the procedures, a medicinal substance is infused through a catheter into the urethra.
With proper and rapid therapy using highly effective medications, which can now be purchased inexpensively in pharmacies, a positive result is guaranteed in the shortest possible time. In the absence of correct timely treatment, urethritis quickly becomes chronic.
Treatment at the VMT MI Clinic. N.I. Pirogov St. Petersburg State University
North-West Center for Pelviperineology (NWTCPP), founded in 2011 on the basis of the Department of Urology of the Clinic of High Medical Technologies named after. N.I. Pirogov St. Petersburg State University, specializes in modern low-traumatic methods of treating stress urinary incontinence (SUI), painful bladder syndrome (interstitial cystitis), overactive bladder (OAB), its leader is Doctor of Medical Sciences, urologist Dmitry Dmitrievich Shkarupa.
Today we have no doubt that the ability to adjust the sling is the cornerstone that was missing to build a clear and effective system for performing sling operations.
Every year, our Center performs more than 600 implantations of an adjustable sling, which has become the standard of care for SUI. The use of this approach made it possible to almost completely eliminate obstructive complications and increase the real (!) effectiveness of the operation to 90%, even in complicated patients.
We consider tracking long-term treatment results to be the most important element of our work. More than 80% of our patients are regularly examined by the Center’s specialists in the late postoperative period. This allows you to see a real picture of the effectiveness and safety of the treatment.
COST OF TREATMENT FOR URINARY INCONTINENCE:
Most patients receive care free of charge as part of compulsory health insurance (compulsory medical insurance).
It is also possible to pay for treatment in cash. The price depends on the volume and complexity of the operation. On average: from 60,000 to 80,000 rubles
(The price includes: surgery, anesthesia, hospital stay, mesh implant and other expenses).
Bibliography
- AskMayoExpert. Female urinary incontinence and voiding dysfunction (adult). Rochester, Minn.: Mayo Foundation for Medical Education and Research. 2021.
- What is urinary incontinence? Urology Care Foundation. https://www.urologyhealth.org/urologic-conditions/urinary-incontinence. Accessed March 18, 2021.
- McAninch JW, et al., eds. Urinary incontinence. In: Smith and Tanagho's General Urology. 18th ed. New York, NY: McGraw-Hill; 2013. https://accessmedicine.mhmedical.com/content.aspx?bookid=508§ionid=41088107. Accessed March 18, 2021.
- South-Paul JE, et al. Urinary incontinence. In: Current Diagnosis & Treatment in Family Medicine. 4th ed. New York, NY: The McGraw-Hill Companies; 2015. https://accessmedicine.mhmedical.com. Accessed March 18, 2021.
- Lukacz ES. Evaluation of women with urinary incontinence https://www.uptodate.com/home. Accessed March 18, 2017.
- Bladder control problems in women (urinary incontinence). National Institute of Diabetes and Digestive and Kidney Diseases. https://www.niddk.nih.gov/health-information/urologic-diseases/bladder-control-problems-women. Accessed March 18, 2021.
- AskMayoExpert. Male urinary incontinence. Rochester, Minn.: Mayo Foundation for Medical Education and Research. 2021.
- Bladder control problems in men (urinary incontinence). National Institute of Diabetes and Digestive and Kidney Diseases. https://www.niddk.nih.gov/health-information/urologic-diseases/bladder-control-problems-men. Accessed March 18, 2021.
- Gameiro SF, et al. Electrical stimulation with non-implanted electrodes for overactive bladder in adults. Cochrane Database of Systematic Reviews. https://onlinelibrary.wiley.com/doi/10.1002/14651858.CD010098.pub4/full. Accessed March 18, 2021.
- Jelovsek JE. Surgical management of stress urinary incontinence in women: Choosing a primary surgical procedure. https://www.uptodate.com/home. Accessed March 18, 2021.
- Frawley J, et al. Complementary and conventional health-care utilization among young Australian women with urinary incontinence. Urology. 2017;99:92.
- Mo Q, et al. Acupuncture for adults with overactive bladder: A systematic review protocol. BMJ Open. 2015;5:1.
- Solberg M. A pilot study on the use of acupuncture or pelvic floor muscle training for mixed urinary incontinence. Acupuncture Medicine. 2016;34:7.
- Vinchurkar AS, et al. Integrating yoga therapy in the management of urinary incontinence: A case report. Journal of Evidence-Based Complementary & Alternative Medicine. 2015;20:154.
- Brown A.Y. Allscripts EPSi. Mayo Clinic, Rochester, Minn. Jan. 24, 2021.
- Ziegelmann MJ, et al. The impact of prior urethral sling on artificial urinary sphincter outcomes. Canadian Urological Association Journal. 2016;10:405.
- Linder BJ, et al. Autologous transobturator urethral sling placement for female stress urinary incontinence: Short-term outcomes. Urology. 2016;93:55.
- Lukacz ES. Treatment of urinary incontinence in women. https://www.uptodate.com/home. Accessed May 9, 2021.
- American College of Obstetricians and Gynecologists (ACOG) Committee on Practice Bulletins - Gynecology and the American Urogynecologic Society. ACOG Practice Bulletin No. 155: Urinary Incontinence in Women. Obstetrics & Gynecology. 2015;126:e66.