In the famous TV series House, Olivia Wilde's character suffered from Huntington's chorea. Thanks to the film, more people learned about this disease. But was it possible to cure the heroine or are her prospects not bright? Let's discuss this disease in more detail.
ALENA PARETSKAYA
Pathophysiologist, immunologist, member of the St. Petersburg Society of Pathophysiologists VALENTINA KUZMINA PhD, neurologist at SM-Clinic Huntington's chorea is a serious disease that affects young people aged 20 to 40 years, occurs with a frequency of one case per 10 thousand population, leading to serious consequences.
What is Huntington's chorea
“According to the modern definition, Huntington’s disease is a chronic, gradually progressive hereditary autosomal dominant disease of the nervous system,” says neurologist Valentina Kuzmina. – The disease is manifested by speech impairment, memory disorders and the presence of obsessive pretentious movements (the person takes awkward poses, twitches, grimaces). Over time it leads to disability; a fairly young person needs constant care and supervision from others. Unfortunately, the disease is still incurable, although there are attempts to treat it, and new methods are constantly being tested.
Pathogenesis
It has been proven that Huntington's chorea develops as a result of an increase in the number of trinucleotide repeats - cytosine-adenine-guanine, located in the first exon of the gene. The cytosine-adenine-guanine triplet encodes the amino acid glutamine, so an elongated polyglutamine tract is formed in the protein. Forming something like a zipper, the extended polyglutamine region of the huntingtin protein changes its own information and binds tightly to other proteins. As a result, protein aggregation occurs, protein-protein interactions are disrupted, which leads to cell apoptosis.
Causes of Huntington's chorea in adults
This is a pathology that is inherited from parents if they pass on defective genes to their child, and they themselves do not get sick.
Neurologist Valentina Kuzmina explains: Huntington's disease is inherited in an autosomal dominant manner, that is, even if a child has inherited one gene, it will manifest itself and give rise to the disease. The prevalence of this disease is 4 - 8 cases per 100,000 population. The reason is that the genetic defect in Huntington's disease prematurely causes the death of certain populations of neurons in the extrapyramidal pathways of the central nervous system.
Due to a defect in genes, the nervous system becomes very fragile, vulnerable, its cells, reaching a certain age, begin to die and are not restored. The extrapyramidal system, which is responsible for our voluntary and involuntary movements, helps us hold posture, coordinate our actions, and regulate muscle tone, is especially affected.
Models for studying Huntington's disease
Animal models of HD appeared more than 30 years ago. The first were models based on the introduction of neurotoxic substances into the striatum (for example, quinolinic acid, an NMDA receptor agonist), which caused neuronal death. Currently, most researchers are working on transgenic animal models, which include not only mice and rats, but also invertebrate animals - the fly Drosophila melanogaster and the worm Caenorhabditis elegans.
Mouse models of Huntington's disease differ from each other in the number of CAG repeats and the level of expression of the transgene - the artificially introduced huntingtin gene. Because The development of HD depends on these factors; different strains of mice differ from each other in the rate of development of pathologies. The most widely used models include the R6/2, R6/1, and YAC128 mouse strains, which were also used in our work. In mice of these lines, the symptoms of the disease are most pronounced and appear quite quickly. In addition, these animals develop cognitive and motor impairments with age and develop partial loss of neurons in the striatum and cortex.
Another way to model HD is to use cell culture. In the simplest case, cell cultures with stable transfection of the huntingtin gene are used. For example, these are PC12 cells containing an inducible transgene of the first exon of huntingtin or striatal neurons expressing huntingtin fragments of different lengths. In addition, primary cultures from neurons from transgenic mice or immortalized neurons can be used.
Signs of Huntington's chorea in adults
“The disease usually manifests itself in the 3rd to 5th decade of life,” explains neurologist Valentina Kuzmina. – Initially, it makes itself felt with barely noticeable signs, but gradually manifests itself in the form of generalized choreic hyperkinesis, namely:
- the presence of obsessive pretentious movements;
- speech impairment;
- memory impairment;
- emotional and personality disorders.
Chorea usually begins in the face or distal extremities (fingers or toes), then gradually spreads and impairs voluntary movements.
Patients cannot hold their tongue out for a long time or clench their hand in a fist. The gait becomes unstable, “dancing”, slow and tense. Speech is difficult to understand, unclear, blurred. Later, dysphagia develops (impaired swallowing of food and water), which causes aspiration (choking and food entering the bronchi), leading to suffocation and pneumonia. Urinary incontinence also appears.
The ability of the gene to manifest itself is close to 100% - by the age of 70, the disease manifests itself in almost all its carriers. Such patients become disabled.
Optogenetics
Optogenetics is a method that combines the approaches of genetics and optics for fine control of the electrical activity of electrically excitable cells (neurons and muscle fibers) [9]. To do this, genes of special light-sensitive proteins—microbial opsins, which are ion channels or pumps—are introduced into the cells under study (Fig. 7). The first work showing the possibility of controlling the electrical activity of neurons using opsin was published in 2005. Over the next few years, a number of experimental works appeared that made it possible to refine this technique and prove its applicability under various experimental conditions.
In recent years, many different opsins have been discovered, of which halorhodopsins and channelrhodopsins have found the most application in optogenetics. When the opsin gene is delivered using genetic engineering methods into a neuron, light-sensitive channels appear on the plasma membrane, and the cell itself becomes light-sensitive. When exposed to blue light, the channelrhodopsin pore opens (maximum absorption - 470 nm), which causes the movement of positively charged ions into the cell, ensuring depolarization of the neuron membrane and the generation of action potentials. When exposed to yellow light, halorhodopsin is activated (maximum absorption - 580 nm), the neuron membrane is hyperpolarized, causing inhibition of the neuron. The high temporal resolution of optogenetics allows for very fine regulation of synaptic events and is therefore an important tool for studying interneuronal connections.
The combined use of optogenetics and classical electrophysiology techniques allows us to benefit from the positive qualities of each of these approaches. The precision of electrophysiological recording is combined with the ability to use light stimuli of varying durations and intensities to help scientists study the workings of neural connections in detail.
The electrical activity of neurons is expressed in sharp voltage surges on the cell membrane and the resulting appearance of an electric current. These sudden jumps are called spikes or action potentials and last a few milliseconds (Figure 8). We found that the longer a neuron is illuminated with blue light, the more spikes it creates during this time. If the illuminated neuron is connected by a synaptic contact with another neuron, then response activity can be recorded on the second neuron, also in the form of individual spikes.
Figure 8. An example of a recording obtained from electrophysiological recording of neuron activity. Spikes (action potentials) are reflected in the recording as vertical lines showing sharp jumps in membrane current.
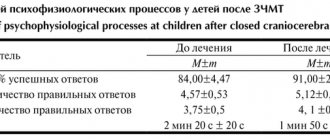
In our experiments, we used a pair of young (14 days) cortical and striatal neurons connected by synaptic contact. The cortical neuron was activated with blue light, and the response activity was recorded on the striatal neuron. It turned out that for a response to occur on a striatal neuron, a certain duration of illumination (activation threshold) is required. If the duration of illumination was below the threshold value, then a spike on a striatal neuron did not occur in response to every flash of light. And most importantly, the activation threshold for neurons from the brains of healthy mice was different from YAC128 mice (with a mutation in the huntingtin gene). This difference was most clearly visible at 50% activation of the striatal neuron, i.e. the duration of illumination at which a spike occurs in response to every second flash of light. The threshold for 50% activation of a striatal neuron in response to irradiation of a cortical neuron for the YAC 128 cell culture was approximately two times (more precisely 2.3 ± 0.8) higher compared to the positive control [10].
It turns out that a mutation in the huntingtin protein leads to the fact that synaptic transmission deteriorates even in young neurons, and the disturbances occur at the functional level (without morphological changes). Could it be that it is these functional disorders that subsequently lead to the appearance of morphological changes, such as the disappearance of spines in old striatal neurons?
To answer this question, we again turned to optogenetics for help, but now with its help we suppressed the activity of neurons with light (Fig. 9a). If our assumption is correct, then the temporary absence of the activating influence of the cortex should lead to the disappearance of spines on striatal neurons in the YAC128 culture. Indeed, after the experiment, the number of spines in the positive control remained unchanged, but in the YAC128 culture it decreased significantly (Fig. 9b, c). It turns out that neurons modeling HD are especially sensitive to weakening the activating influence of cortical neurons , therefore, long-term weakening of the synaptic connection between these neurons leads to a decrease in the number of spines on the 20th day of cultivation [10].
Figure 9. Influencing neurons using optogenetics. a — suppression of cortical neuron activity using optogenetics. When a neuron is illuminated with yellow light (orange stripe), it becomes inactive—there are almost no spikes in the electrophysiological recording during this period of time. b — influence of long-term optogenetic inhibition on the morphology of neurons. Micrographs show a decrease in the number of spines on the dendrite of the YAC128 neuron. c — change in the density of dendritic spines after optogenetic inhibition. In the wild-type culture, the number of spines does not change, but in the YAC128 culture, spine density is significantly reduced.
In summary, we found that in our HD model there is a disruption of synaptic transmission that develops in two stages. At an early stage (young neurons, on day 14 of neuron culture), a functional weakening of the synaptic connection occurs, which at a later stage (old neurons, on day 20 of culture) leads to morphological disturbances of synaptic contacts.
Modern methods of treatment
“Treatment of Huntington’s disease,” explains neurologist Valentina Kuzmina, “is exclusively symptomatic.
To reduce hyperkinesis, antipsychotics and myospasmolytics are used, both in tablets and injectables. To reduce the akinetic-rigid form of the disease, antiparkinsonian drugs are used. For depression, tricyclic antidepressants and selective serotonin reuptake inhibitors are prescribed. For outbursts of aggression - antipsychotics. Rehabilitation will help expand the functional abilities of patients.
Improving the functional capabilities and social adaptation of such patients is a priority task for the doctor.
Conclusion: synaptic transmission disorders and neurodegenerative diseases
The study confirmed our initial guess: disruption of the striatum in HD is associated primarily with disruption of synaptic transmission. The striatum neurons stop “hearing” the commands of the cortical neurons, and, as a result, the person begins to lose control over his movements. But at an early stage of the disease, these disorders are functional in nature and are probably reversible. If we find out the reasons leading to disruption of synapses, then it is possible to develop a drug that will help stop pathological changes, provide striatal neurons with the necessary level of activation and, thus, prevent the development of irreversible morphological disorders.
The results of this work also lead to another important conclusion: when studying neurodegenerative diseases, scientists should pay more attention to synaptic transmission and the interaction of neurons. We know quite a lot about how the accumulation of amyloid aggregates in Alzheimer's disease affects cell activity, and which neurons die during the development of Parkinson's disease, but this has still not led to the emergence of effective therapy. A possible reason for these failures is that we do not take into account the consequences of disruption of synaptic connections - those that we discovered in the study of Huntington's disease. We hope that our findings will point researchers in the direction of developing effective treatments for Huntington's disease, and Thirteen will finally be healthy!
The study was carried out in the laboratory of molecular neurodegeneration of St. Petersburg State Polytechnic University (head of the laboratory - Prof. Ilya Borisovich Bezprozvanny, University of Texas) under the guidance of Ph.D. Dmitry Nikolaevich Artamonov.
Prevention of Huntington's chorea in adults at home
“Currently,” says neurologist Valentina Kuzmina, “rehabilitation using a comprehensive program of therapeutic measures with training of relatives by a team of specialists is applicable: a physical therapy doctor, a physiotherapist, a speech therapist, a clinical psychologist and a neurologist.
Since Huntington's chorea is a hereditary disease, prenatal diagnosis or preimplantation genetic testing of embryos (PGT-M), that is, medical genetic counseling of the family, can be offered as prevention.
Diagnostic Basics
Diagnosis is carried out using physical examination and psychological examination methods, which help to establish the main signs of the disease and assess the extent of the disease. *MRI image (on the left is a person suffering from Huntington’s chorea, on the right is a healthy person)
Of the instrumental diagnostic methods, the main place is occupied by computer and magnetic resonance imaging, which visualize the site of brain damage. Thus, the results of a CT or MRI show an area of atrophy or gliosis in the region of the striatum.
Using magnetic resonance spectroscopy, one more diagnostic sign can be determined - an increase in lactate levels in the tissue of the basal ganglia.
Of the screening methods, the “gold standard” is genetic testing, which is based on identifying an increased number of CAG trinucleotide residues in the HD gene. In the case when their number is 38 or more, the disease will occur over time in 100%. At the same time, there is a pattern that the greater the number of residues, the earlier chorea will appear.
Epidemiology
Huntington's syndrome is most susceptible to Europeans, and among them - Americans. In comparison: the incidence rate among Europeans is 10 cases per 100,000 people, and among other races combined: one case per 100,000 people. In the United States, more than 7,000 people suffer from this disease. Huntington's chorea occurs in both women and men. However, as a percentage, it is much more common among the stronger sex. The disease is genetic and is inherited in about half of the cases. Moreover, the risk of having a child with Huntington's disease from a sick father is much higher than from a sick mother. In addition, in a child who inherited the disease on the paternal side, the most significant increase in trinucleotide repeats is observed and the course of the disease usually has a juvenile form. The reason for the greater paternal inheritance is unknown.
List of sources
- Shtok V.N., Ivanova-Smolenskaya I.A., Levin O.S. Extrapyramidal disorders: Guide to diagnosis and treatment. - M.: Medpress inform, 2002. - 700 p.
- Shtok V.N., Levin O.S. Drug-induced extrapyramidal disorders //In the world of drugs. - 2000. - No. 2. - P. 3-7.
- Seliverstov Yu.A. and others // Nervous diseases. 2014. No. 3. P. 24.
- Tyurin N.A., Artamonova V.A., Alexandrova K.A. and others. Features of the modern course of minor chorea in children. Pediatrics. 1987; 2:20–23.
- Pediatric rheumatology (Guide for doctors) / Ed. Baranova A.A., Bazhenova L.K., 2002; 49.