Benign prostatic hyperplasia (BPH) is the most common urological disorder in men and, up to a certain point, may even be considered a normal physiological process.
In BPH, the cells that make up the prostate begin to proliferate, causing the prostate gland to increase in size. In this sense, it is actually a type of prostate tumor, which, however, is benign in nature and causes negative symptoms only due to growth. It does not disperse or metastasize in the body.
What is the prostate
The content of the article
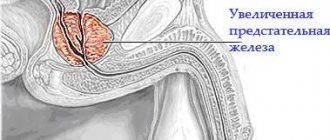
The prostate is a unique organ located in the male pelvis between the bladder and rectum at the beginning of the penis. The organ surrounds the cervical part of the bladder and the initial part of the urethra. It consists of connective tissue, smooth muscle and glandular tissue.
The glands of the prostate produce secretions, which during ejaculation (the release of sperm during sexual intercourse) penetrate the urethra and mix with the secretion of the seminal vesicles. The role of the secretor is to ensure the viability and fertilization of sperm cells with the carbohydrates, enzymes, minerals and other ingredients it contains.
How does the prostate gland grow?
The development of BPH is an almost normal physiological process if the enlarged gland does not cause characteristic symptoms that worsen the well-being and quality of life of a man.
- At birth, the prostate is the size of a pea.
- Then, during adolescence, the organ begins to noticeably enlarge. At this point, it reaches the size of a chestnut, characteristic of sexually active men.
- At the age of forty to fifty years, after several decades of rest, the prostate begins to grow again and hyperplasia develops.
The histological basis of prostatic hyperplasia is the concomitant proliferation of connective tissue, smooth muscle and glandular tissue. Initially and most often it develops in the area of the prostate gland, which immediately surrounds the urethra. Since the prostate has a strong, non-stretchable capsule of connective tissue, the urethra is pinched and becomes narrower. This phenomenon is responsible for the characteristic symptoms.
Accordingly, the incidence of prostate hyperplasia increases significantly with age:
- we can say that hyperplasia practically does not occur until the age of 30;
- between the ages of 40 and 50 years, pathology is detected in 20% of men;
- from 50 to 60 years of age, prostate hyperplasia is diagnosed in every second man;
- Men over 80 years old have BPH in 90% of cases.
Complaints related to hyperplasia are present in every fourth patient at the age of 50 years and in every second at the age of 75 years. The difference in numbers is because not all BPH causes symptoms.
Reasons for the development of prostate adenoma
Stopping cell death.
The reasons for the formation of this process are not fully understood. It is believed that as we age, the relationships between the cells that make up the prostate change, the balance is disrupted, and the number of cells increases. This may play a role in the fact that over time, prostate cells lose their ability to undergo apoptosis.
The process of apoptosis, or programmed cell death, is very important for human tissue as it prevents unrestricted organ growth and eliminates damaged cells, such as cancer cells.
BPH
Aptosis plays a critical role in suppressing the development of cancer processes. An important difference, however, is that while cancer cells lose their organ-specific properties, in the case of BPH this is not the case for newly formed cells - they retain all the properties.
Testosterone and estrogen.
Androgenic hormones, that is, male hormones, primarily testosterone, one of the effects of which is an increase in the size of the prostate gland, probably play a role in the development of prostatic hyperplasia. Elevated testosterone levels predispose to the condition.
Another important factor in the development of BPH is changes in the ratio of female sex hormones, in particular estrogen, to androgens. In the presence of estrogen, the effect of testosterone on the prostate is enhanced. As we age, testosterone levels in the body decrease and estrogen levels increase, so testosterone can continue to function to an increasing degree.
Drug therapy
Drug therapy for prostate adenoma is designed to solve several important problems:
- eliminating difficulty urinating,
- decreased frequency of urination,
- reducing the size of the prostate gland and inhibiting its growth.
The therapy is developed by a urologist who weighs all the pros and cons when prescribing each specific drug, otherwise the drugs can only do harm and worsen the condition.
First stage
“First-line therapy” in the treatment of prostate adenoma is alpha-blockers, which eliminate obstruction of the lower urinary tract and improve urination and bladder emptying. They can be taken for life or until the cause of the obstruction is eliminated.
This group includes 5 drugs that have approximately the same effect:
- Tamsuzolin at a dose of 0.4 mg/day is the most popular drug in Russia; the drug does not require dose selection.
- alfazosin – at a dose of 10 mg/day – has a safe profile.
- silodosin - dose 8 mg/day - have greater selectivity in terms of eliminating unpleasant symptoms.
- Terazosin - the dose is increased gradually - from 1 to 10 mg, it can reduce blood pressure, so it is better to take it at night.
- doxazosin - the dose is selected individually from 1 to 8 mg, significantly reduces blood pressure.
Second phase
The next stage of drug therapy for prostate adenoma is the prescription of drugs from the group of 5-alpha reductase inhibitors, the only drugs that can actually reduce the size of the prostate gland (by an average of 30%). These are the two main medications:
- finasteride - 5 mg per day, course 12 months;
- dutasteride – 0.5 mg per day, course 6 months.
When taking these drugs, the condition can significantly improve: signs of compression of the urethra decrease, the risk of surgery and acute urinary retention are reduced.
Some foreign experts recommend prescribing reductase inhibitors as early as possible in order to early prevent the growth of hyperplasia and eliminate undesirable effects, but this issue is under study.
In addition, 5-alpha reductase inhibitors have a very unpleasant side effect - impaired sexual function, so the use of the drug is limited in young patients.
Important! During therapy with finasteride and dutasteride, PSA levels should be monitored.
Combination therapy
To improve the results of treatment of prostate adenoma, combination therapy tactics are used, which affects various pathological links in the pathogenesis of the disease.
The combination of adrenergic blockers and 5-alpha reductase inhibitors is quite effective. This is the optimal therapy for patients at high risk of further development of prostate adenoma.
Another combination has also proven itself well: muscarinic receptor inhibitors in combination with the same adrenergic blockers. This therapy significantly improves the quality of life of patients with concomitant urinary incontinence.
When prostatic hyperplasia is combined with prostatitis, anti-inflammatory drugs and antibiotics are added to the treatment for adenoma, taking into account the current microflora.
Drugs to normalize urination
With frequent, painful urge to urinate, including at night, the issue of prescribing muscarinic receptor blockers, represented by such drugs as:
- solifenacin,
- tolterodine.
Important! You need to know that the use of antimuscarinic drugs is limited in case of large prostate glands and a significant volume of residual urine, since their use can cause the opposite effect and lead to acute urinary retention.
Desmopressin
With a painful urge to urinate at night, more than 5 times a night, a person is practically deprived of sleep. In this case, it is promising to use an analogue of the antidiuretic hormone - the drug desmopressin, which reduces urination.
But this medicine is prescribed very carefully, by a urologist together with a therapist, under the control of sodium levels in the blood.
Drugs to improve erection in prostate adenoma
An interesting question is the use of a drug similar to the famous Viagra - a phosphodiesterase type 5 inhibitor (PDE-5):
- Tadalafil at a dose of 5 mg per day, in addition to improving erection, has a positive effect on the process of emptying the bladder - it eliminates difficulty urinating and prevents inflammation of the prostate gland.
Important! Tadalafil (Cialis) is used exclusively. Viagra has a different active ingredient (siddenafil), which in this case will not have a therapeutic effect. Levitra (vardenafil) is also not used.
Symptoms and consequences of prostatic hyperplasia
Symptoms of an enlarged prostate can significantly impair quality of life, but the condition is currently treatable. Therefore, if you suspect an adenoma, you should immediately consult a practicing urologist.
Unfortunately, patients often seek medical help only after a long period of distressing symptoms. Men feel embarrassed and find it difficult to share their complaints with strangers, even with doctors. However, it should be emphasized that the condition is well managed, but the symptoms can have a significant impact on the quality of life, so you need to put aside prejudices and make an appointment with a doctor.
In case of prostatic hyperplasia (BPH), the patient experiences the following symptoms:
- difficulty passing urine;
- the urine stream is thin and may be intermittent;
- complete emptying of the bladder is possible with tension;
- passing a small amount of urine at a time, but frequent urges, even at night.
The above symptoms are called obstructive. To understand, an enlarged prostate can be thought of as a valve, and the bladder as a balloon filled with air. In order for the air to escape, we must apply pressure. The narrower the valve, the more force is required to push the air out.
The diameter of the valve is an indicator of the size of the prostate gland: the larger the prostate, the more it compresses the urethra, narrowing its diameter.
Another group of symptoms, irritation symptoms, include: a sudden, strong urge to urinate, drops of blood in the urine, and urinary obstruction.
Because you are unable to completely empty your bladder each time you urinate, the urine begins to stagnate or become infected with bacteria, leading to an inflamed bladder. This leads to more frequent, painful urination. Urine may change color.
Symptoms and stages of BPH
The average age at which a patient experiences discomfort with prostatic hyperplasia is 65 years.
Symptoms vary depending on the severity of the disease, and are usually caused by narrowing of the urethra by an enlarged prostate.
As a result, the most common complaint is weak urine flow and increased frequency of urination.
Other signs that may indicate both benign prostate enlargement and other pathologies of the genitourinary system:
- Passing only a small amount of urine.
- Frequent urination with a feeling of incomplete emptying of the bladder.
- A sudden urge to urinate.
- Involuntary loss of urine (urinary incontinence).
- Burning or other discomfort when urinating.
- Pain in the lower abdomen
- Multiple bladder infections
- Burning or pain during intercourse
- The development of erectile dysfunction, as well as a decrease in sexual desire (libido).
Benign prostatic hyperplasia is divided into three stages:
- First stage: compensated
At this stage, clinical symptoms such as weak urine flow, frequent urination, especially at night, have already begun to manifest themselves.
However, at this stage, the formation of residual urine is not observed, and the symptoms of the disease themselves do not particularly bother the patient.
This stage can last up to three years.
Although some men, especially in the early stages, adapt to the symptoms and cope with them relatively well.
But complaints related to urinary urgency become a serious burden on daily life.
- Second stage: subcompensated
The capacity of the bladder decreases, it is no longer able to function adequately, the volume of residual urine can be 50-100 ml or more.
At this stage, the walls of the bladder thicken and signs of renal failure may develop.
- Third stage: Decompensated
Discomfort, such as urinary retention and bladder fullness, are pronounced at this stage.
Clear signs of renal failure appear, the patient loses weight, the mouth is constantly dry and smells like urine.
Bladder wall pseudodiverticulosis (protrusion of the bladder wall) may also occur.
Also hydronephrosis (enlargement of the renal pelvis with potential destruction of kidney tissue).
Similar symptoms also appear with prostate cancer and bladder cancer.
To make an accurate diagnosis and prescribe effective treatment, you need to make an appointment with a urologist immediately after the first signs of BPH appear.
Symptoms of benign prostatic hyperplasia can be divided into two groups.
1. Neurogenic bladder
Weak, intermittent outflow of urine, urination drop by drop, difficulty starting urination, pressure in the abdominal cavity, a feeling of incomplete emptying of the bladder, urinary retention.
2.Overactive Bladder Syndrome
Urination at night, urgency, urinary incontinence.
Complications of prostate adenoma
Complications of advanced cases of prostatic hyperplasia:
- bilateral dilatation of the renal pelvis and, as a consequence, renal failure;
- bladder stones;
- stagnation, obstruction of urine, when the prostate gland is completely suppressed in the initial part of the urethra, making urination impossible.
With urinary obstruction, the patient suddenly experiences severe pain in the lower abdomen. The condition requires immediate treatment, consisting of prompt insertion of a catheter to drain urine.
Strong pain
Stages of development
Conventionally, there are three stages of manifestations of prostate adenoma. The main criteria are the volume of the prostate and the presence of “residual urine” - the amount that remains in the bladder after complete urination (determined by ultrasound).
Symptoms of the disease are grouped according to the International Index of Prostate Symptoms (IPSS), presented in points:
- minor symptoms - 0–7 points;
- moderate - 8–19 points;
- pronounced - 20–35 points
In stage I - the volume of the gland is 30-40 cm3, residual urine is insignificant, up to 40 ml.
In stage II - the volume of the gland reaches 40-60 cm3, residual urine can be up to 100 ml.
In stage III - the volume of the gland is very large, 60-80 cm3 or more, residual urine reaches a volume of more than one liter. At this stage, paradoxical ischuria develops, when, through a very weak external sphincter, urine randomly leaks from an overstretched bladder.
It should be understood that the stage of prostate adenoma does not always depend on the size of the prostate gland; the location of the gland in relation to the area of the urethra, as well as the time at which the process is neglected, is of great importance.
Prostate Exam – What to Expect
The most unpleasant, but quick and painless part of the examination is a rectal examination of the prostate, which provides very important information for the urologist.
As a first step in assessing a patient for BPH symptoms, the urologist will ask you for detailed information about urinary and genital complaints and previous medical conditions.
An important element of the subsequent physical examination is careful palpation of the abdomen, which allows the expert physician to confirm that the bladder is full.
"Ethnoscience
Many patients with prostate adenoma use herbal preparations for therapy. Herbal preparations undoubtedly have some effect, but extensive clinical international studies have not been conducted on them! Therefore, the use of these drugs is of an auxiliary nature. In Russia, products isolated from African palm trees are widely used: Serenoa repens (Prostamol UNO, Permixon), Pigeum Africanum (Pidgeum), Hypoxisrooperi (Hypoxis).
Of the domestic traditional medicines, the following are most often used as additional restorative therapy for prostate adenoma:
- Beekeeping products (honey, bee bread, dead bees, propolis) - inside;
- A decoction of young aspen bark;
- Decoction of fireweed (angustifolia fireweed);
- Red root decoction (Altai endemic - forgotten kopeck) decoction;
- Pumpkin seeds (contain zinc, so necessary for the prostate) up to 50 pieces per day orally;
- Burdock root decoction.
In addition, in Russia, products from animal raw materials are actively used - the prostate of bulls, in suppositories and injections.
Such drugs as Vitaprost, Prostatilen, Prostakor and Samprost. There are only Russian studies on these drugs, and a certain effect occurs, especially with concomitant prostatitis, but, again, there have been no broad international research programs.
Hirudotherapy (leech treatment), which reduces inflammatory edema and improves blood circulation in the prostate area, is of some importance in terms of symptomatic treatment of prostate adenoma. However, such therapy is fraught with bleeding and should be carried out only by qualified specialists.
Important! It should be clearly understood that all of the above remedies have a rather uncertain effect, therefore, if symptoms of prostate adenoma develop, a visit to a urologist is mandatory!
Useless remedies and contraindications
The following have a completely incomprehensible effect: shock wave therapy, Sytin's moods, salt dressings, urine therapy, Thermex, magnetotherapy, microenemas, Vitafon, Almag, hydrogen sulfide baths, phonation, Chinese urological patch, radon baths, various dietary supplements, homeopathy, treatment salt according to the method of Professor Okulov, hydrogen peroxide according to Neumyvakin, beaver stream, indigal, adenorphine and other “exotic” agents.
Important! In case of prostate adenoma, are contraindicated , otherwise this can lead to progression of the disease and even the development of oncology.
Blood tests
When examining for any prostate pathology, blood tests are required. The results may indicate certain diseases and also provide important information about kidney function.
Determining the amount of a specific protein, prostate-specific antigen (PSA), is important for the study of prostate diseases. PSA is produced in the body only by prostate cells, and its concentration in the blood is proportional to the size of the prostate. However, the test is not specific for BPH and the results may be elevated in other prostate diseases.
PSA blood test
PSA can increase with inflammation of the prostate gland, cancer, and even immediately after ejaculation. Some treatments (such as transurethral resection of the prostate) and some medications lower the amount of PSA in the blood. PSA comes in two forms, free and bound, and it is important for your doctor to know the amount of both.
Urine tests
Because BPH causes problems with emptying the bladder, a laboratory urine test is required to diagnose the condition.
Measuring urine flow is a simple method of determining the maximum flow rate and average urine flow rate. There is a curve regarding the dynamics of urine output, the shape of which conveys important information to the urologist, although decreased urine flow can be caused by other diseases of the prostate and bladder or urethra. The examination is painless.
It is also important to measure the amount of urine remaining in the bladder after urination. This is done using an ultrasound machine. The amount of residual urine can also be determined using catheterization.
Diagnostic procedures: detection of BPH
An accurate diagnosis is made based on medical history, physical examination, imaging, and laboratory tests of blood and urine.
At the first stage of the examination, the urologist will conduct a thorough interview with the patient.
Based on the information received, he will be able to suspect or make a preliminary diagnosis of the presence of benign prostatic hyperplasia.
The next step is to examine the prostate through the rectum - rectal palpation.
This is a key diagnostic method.
Allows an initial assessment of the size of the prostate gland and its consistency, which is part of the differentiation of hyperplasia and malignant process in the prostate.
Laboratory diagnostics are mandatory, which includes:
- general urine analysis
- biochemical indicators of renal function (urea, serum creatinine)
- culture of prostate secretion (if an infectious process is suspected)
- PSA test, that is, the concentration of prostate-specific antigen in serum (to exclude prostate cancer)
Normal PSA values range from 0 to 4.0 ng/ml and increase with age and prostate volume.
An increase in PSA levels is most often caused by prostate cancer.
But it can also be against the background of acute or chronic prostatitis, after a rectal examination, catheterization of the bladder or various endoscopic procedures performed in the lower urinary tract.
To confirm the diagnosis and additionally assess the condition of the genitourinary system, other instrumental studies can be used:
- Ultrasound of the urinary tract to evaluate their morphology and determine the volume of urine remaining after urination.
- Transrectal ultrasonography, which allows for accurate diagnosis of lesions and foci located deep in the prostate gland, with the possibility of puncture, that is, collection of biological material for histological examination and biopsy.
- A pressure-flow urodynamic test (urofluometry) performed when there is doubt about the cause of urinary problems.
The appropriate specialist for prostate disease is a urologist.
Depending on the type and severity of your symptoms, your doctor will determine whether other tests are needed.
For example, such as cystoscopy (endoscopic examination of the bladder)
Rectal ultrasound, abdominal ultrasound
Rectal ultrasound examination of the prostate gland gives a clear picture of the prostate gland, its size and structure. An experienced urologist may also look for other conditions, such as prostate cancer.
At the same time, an ultrasound of the abdominal cavity is performed. It is necessary to evaluate the kidneys, bladder and, to a lesser extent, the prostate gland.
Abdominal ultrasound
Other tests
- Intravenous urography.
The urinary system (kidneys, urinary tract, bladder, urethra) can be examined using intravenous urography. The patient is given an injection of a contrast agent, then an x-ray of the abdominal cavity is taken. - Endoscopic examination
. Lower urinary tract endoscopy is also not a routine test. The test involves inserting a small device with a small camera at the end through the urethra and into the bladder. The image transmitted by the camera appears on the screen, allowing the doctor to assess the condition of the lower urinary tract. The method is also suitable for histological sampling if a malignant process is suspected.
Operations
Urologists at the Yusupov Hospital masterfully perform classical and minimally invasive surgical interventions and use innovative methods of surgical treatment of prostate adenoma.
Each patient is selected for the operation that suits him best. The generally accepted standard in the surgical treatment of prostate adenoma is transurethral resection of the prostate. The operation is highly effective. After the intervention, patients get rid of bladder outlet obstruction (narrowing of the urethra) and associated symptoms. The rehabilitation period is short. During or after surgery, bleeding and “water intoxication” syndrome may develop in the body.
Alternative methods of treating prostate adenoma include the following surgical interventions:
- Stenting;
- Balloon dilatation;
- Hyperthermia;
- Thermotherapy;
- Ultrasound, laser and needle ablation;
- Interstitial coagulation.
After them, complications occur less frequently, but these techniques are inferior to transurethral resection in terms of effectiveness, both clinically and economically.
Laparoscopic removal of prostate adenoma is used when the tumor has grown significantly, and removing it using transurethral resection is problematic. This operation is more complicated and is performed under anesthesia. Through small incisions, the surgeon inserts special instruments into the body cavity, which are used to remove the prostate adenoma. The operation is carried out using images from video cameras, which are displayed on the screen. The main advantages of the intervention are minimal blood loss and low likelihood of complications. After the operation, the patient does not need long-term rehabilitation.
When there are signs of prostate adenoma in men, doctors use a high-tech method of treating adenoma - laser enucleation. The intervention is carried out when the tumor is large. Excess tissue is removed using a laser. The operation is performed through the urethra. The tumor is separated, divided into small parts, and then removed. The method is considered minimally invasive. It has a number of significant advantages: it does not violate the integrity of cavities and does not cause unnecessary damage.
Laser vaporization involves destroying the adenoma by laser evaporation. The urologist inserts a special device through the urethra, brings it to the tumor and precisely targets it with a strong green laser. The depth of penetration of the laser and the accuracy of its impact make it possible to avoid damage to neighboring areas. The method is minimally invasive, bloodless, fast and effective. Its only drawback is the inability to take tumor tissue for histological examination.
In some situations, the inevitable method of treating prostate adenoma is abdominal surgery - adenomectomy. It is performed when other methods cannot help the patient. During surgery, the surgeon uses a scalpel to access the prostate gland and manually, using surgical instruments, removes the adenoma. As a result of the operation, significant blood loss and complications may develop. After surgery, the patient needs long-term rehabilitation.
Removal of prostate adenoma using transvesical (transvesical) adenomectomy involves radical excision of hyperplastic prostate tissue through a longitudinal incision in the anterior abdominal wall and bladder. The operation is performed in advanced stages of the disease, when the tumor reaches a large size, the bladder is overstretched due to its overflow with accumulated urine, and renal failure develops.
The bladder is pre-catheterized and filled with a sterile solution of furatsilin or another substance. Then it is isolated and taken in two places on special holders, for which the wall of the organ is lifted. The surgeon cuts through the resulting fold and opens the bladder.
Along the inner end of the installed urinary catheter, the area of the bladder neck is determined and around the urethral opening that appears in the field of view, stepping back from it by 0.5-1 cm, an incision is made in the mucous membrane. After this, the operating urologist penetrates the thickness of the prostate with his finger, enters it between the tumor capsule and adenomatous nodes, and removes the latter. At the same time, with the finger of the other hand, which is first inserted into the patient’s rectum, the doctor moves the gland towards the anterior abdominal wall. It becomes more accessible to manipulation. Thanks to this technique, the operation time is reduced and blood loss is reduced.
Then the surgeon performs hemostasis (stopping bleeding) of the bed of the removed adenoma and suturing the bladder, leaving a thin drainage in the wound. It is designed to wash its cavity from formed blood clots. The urinary catheter inserted before the operation is not removed for 7-10 days. A new section of the urethra is formed around it instead of the prostatic part of the urethra excised during the operation.
Transvesical adenomectomy is one of the most traumatic of all techniques used for prostate adenoma. It is accompanied by the risk of developing the following complications:
- Bleeding from the tumor bed;
- Congestive pneumonia;
- Violation of the motor-evacuation function of the intestines, manifested by constipation.
To avoid complications, after surgery at the Yusupov Hospital, the patient undergoes early activation. The following undesirable consequences of surgery to remove prostate adenoma may occur:
- Insufficient drainage of the bladder;
- Narrowing of his neck;
- Urinary infiltration of peri-vesical tissue;
- Formation of a “pre-bladder” (residual cavity in the place where the prostate adenoma was removed);
- Formation of narrowing of the lumen of the urethra;
- Urinary incontinence.
This negatively affects the quality of life of patients and prolongs the time required to restore adequate urination.
The consequences of the operation are less pronounced when the intervention is performed using a laparoscope. Laparoscopic surgery to remove prostate adenoma is one of the less invasive options for surgical interventions on the prostate gland. Urologists at the Yusupov Hospital use this technique if the patient has a sufficiently large prostate adenoma.
If the size of the prostate gland of a patient with adenoma does not exceed 120 cm3, transurethral resection of the prostate adenoma is recommended. But for 10% of patients who need surgical intervention, this option is not suitable, since the gland reaches a size of more than 120 cm3. Laparoscopic surgery to remove prostate adenoma is not performed for urolithiasis, inguinal hernia, bladder diverticula, or ankylosis of the joints of the lower extremities. In this case, the decision on the possibility of performing an operation is made collectively by a urologist, andrologist, abdominal surgeon and other specialists at the Yusupov Hospital.
With laparoscopic access, general anesthesia is used. Laparoscopic removal of prostate adenoma is carried out using specialized equipment. The surgeon uses trocars through which he passes laparoscopic instruments to the prostate gland. The trocar is equipped with a small video camera that transmits the image to the screen. This way, surgeons have the opportunity to perform all actions as accurately as possible.
Laparoscopic surgery to remove prostate adenoma has the following advantages over open adenomectomy:
- During the operation, bleeding and complications occur much less frequently;
- The pain syndrome is less pronounced, the patient does not need a large amount of analgesics;
- Bladder catheterization does not last long;
- Physical activity is restored faster, the next day after the operation the patient can walk without difficulty.
- Hospitalization after laparoscopic adenomectomy takes much less time. The patient quickly returns to normal life. He has no cosmetic problems. The length of scars after surgery does not exceed one centimeter.
After laparoscopic removal of prostate adenoma, the need for repeated surgery is minimized, since a significant part of the prostate tissue is removed.
Embolization of prostate arteries is one of the most modern methods of treating adenoma. It is used more often abroad. The operation involves blocking the blood vessels supplying the prostate adenoma. An endovascular surgeon for large blood vessels brings a microcatheter to the source of blood supply to the tumor and injects a special composition that blocks the blood flow. As a result, the tumor does not receive oxygen and nutrients, and it decreases in size. Contraindications to the use of this method are malignant tumors, allergies to contrast and embolic agents, cardiovascular pathology, some chronic diseases of internal organs, and acute diseases.
Transurethral resection of the prostate (TURP) is a method of removing prostate adenoma without external incisions. The intervention is performed using a special instrument (resectoscope). The urologist inserts it into the patient’s bladder through the urethra. After examining the urethra, bladder and the actual area where the prostate adenoma is located (the border of the urethra and bladder), the surgeon removes the prostate adenoma using a special device - a loop. Transurethral resection of the prostate requires good visibility. It is ensured by a constant flow of fluid through one of the resectoscope channels and outflow through the other channel. Visibility may be impaired due to bleeding from blood vessels. During the operation, the surgeon stops the bleeding in order not to lose orientation in the tissues.
Transurethral resection of the prostate is used if the size of the prostate gland does not exceed 80 cm3. The adenoma is removed until the tissue of the gland itself is visible. After the prostate adenoma is removed, the tissue is washed from the bladder using a special instrument, and a control examination of the surgical site and the bladder is carried out. If necessary, additionally stop bleeding from blood vessels. After this, the surgeon removes the operating instrument (resectoscope). A special Foley catheter is passed through the urethra into the bladder. An inflating balloon is located at the bladder end of the catheter. After the catheter is inserted into the bladder, the balloon is filled with fluid. It takes the place of the removed adenoma, which helps stop bleeding from small vessels and prevents the catheter from falling out of the bladder. In this case, minimal consequences are observed after removal of the prostate adenoma. Patient reviews of the operation are excellent. Recovery after removal of prostate adenoma occurs quickly.
Transurethral resection of the prostate is one of the most complex and precious operations in the entire spectrum of endoscopic urological surgery. Urologists at the Yusupov Hospital have undergone special training. Surgeons are fluent in the technique of this surgical intervention.
Transurethral electrovaporization combines the advantages of standard transurethral resection (the possibility of immediate removal of tumor tissue, optical control of the intervention, clinical and economic efficiency) with a significant reduction in blood loss during and after surgery, preventing “water intoxication” of the body. Electrovaporization of the prostate also has disadvantages. “Roller vaporization” is technically simple, there is good endoscopic visibility, there is no bleeding, but, compared to monopolar transurethral resection, it has a lesser ability to remove hyperplastic tissue. Roller vaporization is used as monotherapy for prostate adenoma with a volume of no more than 40 cm3. Vaporizing resection is not inferior in efficiency and speed to standard transurethral resection. It is just as difficult to master, since the hemostatic effect of the vaporizing loop is not as pronounced as the “roller vaportrode”, and the technique of cutting and removing prostate adenoma requires considerable experience of the surgeon.
New methods of transurethral endoscopic treatment of prostate adenoma include rotoresection. The technique combines electrovaporization, coagulation and mechanical removal of the prostate tumor with a rotating electrode. Due to sufficient depth of coagulation, good bleeding control is ensured during surgery, and the simultaneous mechanical removal of dehydrated and carbonized tissue with a rapidly rotating rotoelectrode allows the urologist to continue effective ablation by evaporation. Patients of the Yusupov Hospital have the opportunity to receive all complex methods of treating prostate adenoma at partner clinics.
Treatment of mild forms of BPH
In many cases, benign prostatic hypertrophy does not require treatment at all, or treatment is not very difficult.
Your doctor plans treatment for BPH depending on the severity of your complaints, test results, and the patient’s general condition. Treatment may be surgery or medication, including other complementary methods.
In some cases, the wait-and-see approach can be used because immediate intervention is not always required. If symptoms are mild and tests rule out complications or other abnormalities, there is a high probability that the condition will not worsen. In such cases, follow-up examinations are carried out at regular intervals. It is very important that the patient understands the importance of follow-up tests. Therefore, this path is only possible for conscious patients.
Will herbs help with hyperplasia?
Some natural drugs have good activity in the mildest forms of BPH, but their mechanism of action is not well understood and is unpredictable. Their use can reduce irritating symptoms and increase urine flow. Some compounds also have weak antiandrogenic, antiestrogenic, anti-inflammatory, analgesic and diuretic effects.
Most of these formulations have been shown to work well, but their use may pose risks. Therefore, you can drink herbal infusions only as prescribed by a urologist.
When purchasing over-the-counter medications, the patient feels “safe”, believing that they have solved the problem. But such treatment ends with the patient seeing a doctor only after the complaints become painful, when secondary disorders or complications may develop. The situation can be even more serious if the complaints are not caused by BPH, but by prostate cancer, in which early diagnosis can decide the fate.
Medicines to treat prostate problems
In drug therapy for BPH (conservative treatment), there are two main groups of active ingredients: alpha blockers and reductase inhibitors.
Alpha blockers have a therapeutic muscle relaxant effect on smooth muscles. By relaxing the smooth muscle cells present in the prostate and bladder, the pressure decreases and symptoms improve significantly. Improvement in urinary symptoms begins within a few days.
Reductase inhibitors suppress the formation of the active form of testosterone. This process occurs in the cells of the prostate gland. When the 5-alpha reductase enzyme is blocked, testosterone is unable to convert into its active form and therefore has no effect on prostate cells.
The use of a reductase inhibitor in patients with higher grades of BPH is advisable because treatment may result in a reduction in prostate size. The results of therapy begin to appear after about three months.
Prostate hyperplasia: scalpel or pills?
Modern drug therapy for benign prostatic hyperplasia L.M. Gorilovsky, MD, professor, D.A. Lakhno, PhD, Research Institute of Urology, Moscow Journal "Medical Council" No. 7-8 (2010) Published on the Remedium website
One of the most common urological diseases in older men is benign prostatic hyperplasia (BPH). According to epidemiological data, the prevalence of BPH in most countries reaches 20% in 50-year-old men, 50% in 60-year-old men, 57% in 70-year-old men and 80% in 80-year-old men. The average attendance for BPH in Russia, according to N.A. Lopatkin et al., in 2000 was 113–125 per 100,000 male population. The likelihood of undergoing surgical treatment in a man over 60 years of age with prostatic hyperplasia and lower urinary tract symptoms (LUTS), according to some researchers, reaches 39% [1].
Thus, BPH is one of the most common diseases leading to surgical intervention. Increasing life expectancy leads to an increase in the number of men suffering from BPH, and the improvement in their quality of life reduces tolerance to the disease, preventing them from continuing an active lifestyle.
Demographic studies from the World Health Organization, indicating a significant increase in the population over the age of 60, emphasize the socio-economic significance and relevance of this problem. The growth rate of this disease significantly exceeds the growth of the planet's population as a whole. It should be noted that the elderly population has great vital, productive and intellectual potential, which should be fully used by society.
The progression of BPH consists of worsening clinical indicators, including an increase in the volume of the prostate gland, worsening LUTS and a decrease in the maximum volumetric flow rate of urination (Qmax), an increased risk of developing acute urinary retention (AUR) and the need for surgical treatment of BPH, as well as a decrease in the quality of life associated with BPH [2].
Due to the fact that frequent urination, sluggish urine stream, stranguria, nocturnal pollakiuria, which are the main symptoms of BPH, significantly worsen the quality of life, the main task of the urologist is to timely diagnose these diseases and carry out early treatment measures aimed at improving the quality of life (Gorilovsky L.M., 2004).
According to modern concepts, the diagnostic complex when examining a patient with BPH includes: collecting anamnesis, quantitative assessment of symptoms and “quality of life” using the International Prostate Symptom Score - IPSS (the table is given in the article “Prostate adenoma: know your maneuver” - VM); study of the level of prostate specific antigen (PSA), urea and serum creatinine; analysis of urine and prostate secretions; digital rectal examination; transabdominal ultrasound examination of the kidneys and bladder with determination of the amount of urine; transrectal ultrasonography, uroflowmetry. In some cases, urodynamic studies may be necessary.
Until recently, a urologist and a patient diagnosed with BPH were faced with a choice: either undergo surgical treatment or wait and observe. Surgical treatment included transvesical or retropubic prostatectomy or transurethral resection of the prostate with its modifications. Recently, along with the increase in the incidence of BPH, the number of treatment methods for these patients has significantly increased. First of all, medications have appeared with which you can achieve a good effect, especially in the initial stages of the disease.
Advances in understanding the pathogenesis of prostatic hyperplasia and the creation of medications with a pathogenetically targeted mechanism of action have led to the fact that drug therapy for certain categories of patients has become truly effective. Modern pharmacotherapy allows many patients to avoid unwanted surgical treatment and associated dangerous complications, such as irreversible urinary incontinence and loss of sexual function with subsequent impairment of quality of life [3].
And although drug treatment does not relieve the patient of prostatic hyperplasia, it makes it possible to significantly reduce complaints, improve impaired urination and normalize the quality of life. Drug therapy for lower urinary tract symptoms has been actively used for 15 years in BPH. In the early 1990s, long-acting selective α-blockers terazosin and doxazosin appeared, and a few years later the first 5α-reductase inhibitors appeared on the pharmaceutical market. These two groups of drugs have become the mainstay for the treatment of BPH, sharply reducing the number of transurethral resections of the prostate. For example, in the United States, the number of transurethral and open adenomectomies decreased from 250,000 in 1987 to 88,000 in 2000 [4].
When choosing a treatment method, the doctor must evaluate the data from instrumental research methods and the patient’s problems, reflected in the IPSS questionnaire. As part of the standard examination of such patients, it is recommended to assess the subjective perception of the severity of BPH symptoms and the effectiveness of its treatment. This is due to the fact that the most common symptoms are often not the most troubling for patients [5].
The diagnostic criteria for prescribing conservative therapy when diagnosing BPH are: total IPSS score greater than 7 and less than 19; maximum urine flow rate (Qmax) more than 5 ml/s; the volume of residual urine is not more than 150 ml; the presence of contraindications to surgical treatment due to concomitant diseases; patient's refusal to undergo surgery. According to the 4th International Consultation on BPH (1997), the absolute indications for surgical treatment are: urinary retention; recurrent gross hematuria caused by benign enlargement of the prostate gland; large bladder diverticula; renal failure, bladder stones or recurrent genitourinary tract infections due to bladder outlet obstruction [6].
The group of choice for the symptomatic treatment of obstructive symptoms of BPH are α-adrenergic receptor blockers, the effects of which are aimed at elements of the autonomic nervous system, which are components of the dynamic component of bladder outlet obstruction in BPH. Alpha-blockers reduce symptoms and improve urodynamic parameters, but their effect in stopping the progression of BPH and reducing the risk of the need for surgical treatment of BPH has not currently been demonstrated.
Tamsulosin (omnic (Astellas Pharma); tulosin (Egis)) is the most effective α-blocker used for the drug treatment of BPH. Its unique features of use (efficacy without side effects, no need for dose titration, no effect on blood pressure) may be due to both the relatively low therapeutic dosage of 0.4 mg with the greatest α-blocking effect, and selectivity to the subtype (α1a- adrenoreceptors). Tamsulosin selectively and competitively blocks postsynaptic α1A-adrenergic receptors located in the smooth muscles of the prostate gland, bladder neck and prostatic urethra. This leads to a decrease in the tone of the smooth muscles of the prostate gland, bladder neck and prostatic urethra, improving the outflow of urine. At the same time, the symptoms of obstruction and irritation associated with benign prostatic hyperplasia are reduced.
The ability of tamsulosin to act on α1A-adrenergic receptors is 20 times greater than its ability to interact with α1B-adrenergic receptors located in vascular smooth muscle. Due to its high selectivity, the drug does not cause any clinically significant decrease in systemic blood pressure both in patients with hypertension and in patients with normal initial blood pressure. The bioavailability of tamsulosin is about 90%, and stable concentrations in the blood when taken daily are achieved on average within 5 days. The main site of tamsulosin metabolism is the liver, and enzymes from the cytochrome group play an important role in this process. The most common side effects of tamsulosin are nasal congestion, headaches and impaired ejaculation. The pharmacological characteristics of tamsulosin are of great clinical importance. The absence of a significant effect on the cardiovascular system allows one to avoid titrating the dose of tamsulosin. Thus, the maximum clinical effect of its use is achieved quite quickly. The clinical efficacy of tamsulosin at a standard dose (0.4 mg once daily) has been extensively studied in several multicenter, randomized, placebo-controlled, double-blind studies conducted in Europe and North America, involving more than 1300 patients. These studies confirmed the long-term effectiveness and safety of tamsulosin as a drug for the pharmacotherapy of benign prostatic hyperplasia [7].
Omnic Ocas is a controlled-release tablet based on a matrix using a non-ionic gel that provides long-lasting, slow release of tamsulosin and gives sufficient exposure with low fluctuations over 24 hours. This provides around-the-clock effective control of lower urinary tract symptoms.
Data from several international studies of the effectiveness of the use of α-blockers indicate that many patients, along with a decrease in the severity of LUTS, note an improvement in sexual function. It is believed that the reason for this effect is the polyvalent mechanism of action of α-adrenergic blockers, which improves blood circulation in the pelvic organs and generally improves the patient’s quality of life [8].
As noted above, for all their advantages, α-blockers are not able to influence the progression of the disease. In case of a high risk of disease progression (prostate volume exceeds 50–60 cm3), it is recommended to introduce 5α-reductase inhibitors into therapy. It is known that 5α-reductase inhibitors are able to inhibit the progression of the disease as a result of inhibiting the conversion of testosterone to dihydrotestosterone, an androgen, which is considered the main factor influencing the hyperplastic growth of prostate tissue. 5α-reductase inhibitors not only inhibit further growth of BPH, but also reduce the size of the prostate if it is enlarged [9,10]. Of the drugs used for the conservative treatment of men suffering from BPH, only 5α-reductase inhibitors are able to influence the pathophysiological mechanisms underlying the disease. There are two isoforms of 5α-reductase (type 1 and type 2). Today, two drugs from the group of 5α-reductase inhibitors are available in Russia, which significantly reduce the volume of the prostate gland - finasteride and dutasteride. Finasteride, which blocks type 2 5α-reductase, has been known for a long time, and the effect of its administration becomes obvious, on average, after six months of treatment. Dutasteride is a 45 times more potent type 1 5α-R inhibitor than finasteride and a 2.5 times more potent type 2 5α-R inhibitor. It provides greater suppression of serum DHT (α93% vs. 70%). These characteristics determine an earlier onset of the effect: a decrease in prostate size and an increase in Qmax. In Western countries, dutasteride under the commercial name Avodart was registered and approved for clinical use in 2002, in Russia - in 2005. The effectiveness and safety of dutasteride was assessed in a pooled analysis that included 3 placebo-controlled, two-year, double-blind studies.
Already 2 weeks after the start of treatment with dutasteride, there was a decrease in serum dihydrotestosterone levels by more than 90%, and this decrease was maintained until the end of the study. Over 2 years, prostate volume decreased by 25.7%. In addition, during treatment with dutasteride, there was a persistent decrease in the severity of symptoms of the disease, an increase in Qmax and a decrease in the risk of developing AUR by 57% and the need for surgical treatment by 48% [11]. For adult men, including elderly patients, the recommended oral dose is 500 mcg (1 capsule) once a day.
The most significant side effects with dutasteride monotherapy are: impotence, changes (decreased) libido, ejaculation disorders, gynecomastia. Analysis of data obtained from the above-mentioned placebo-controlled studies showed that adverse events that occurred were usually mild or moderate in severity and most often related to sexual dysfunction. Moreover, both in the avodart group and in the placebo group, the vast majority of patients (89 and 94%, respectively) did not have sexual function disorders. It should be noted that in terms of the frequency of recorded adverse events associated with taking the drugs, statistically significant differences between the dutasteride and placebo groups were, as a rule, observed only during the first 6 months of therapy. During further treatment, differences between groups in the most common adverse events disappeared.
The different pharmacological characteristics and mechanism of action of α1-blockers and 5α-reductase inhibitors provide the basis for the development and use of rational combination therapy. The combination of Avodart (dutasteride) and tamsulosin was studied in a 4-year, multicenter, randomized, blinded CombAT trial. The study involved parallel groups of 4844 men (mean age 50 years) with a clinical diagnosis of BPH. The indicator on the international scale of manifestations of prostate diseases was more than 12, prostate volume - more than 30 cmα, PSA level - 1.5-10 mg/ml, maximum urinary flow rate (Qmax) - more than 5-15 ml/s, minimum volume of urine excreted - 125 mg. They took tamsulosin 0.4 g orally daily; dutasteride 0.5 mg or their combination. The primary endpoint of 4-year follow-up was the occurrence of acute urinary retention or surgery for benign prostatic hyperplasia. Secondary endpoints of the study included analysis of clinical progression of BPH, symptoms, Qmax, prostate volume, safety and tolerability. The results of combination therapy were far superior to tamsulosin monotherapy but not to dutasteride monotherapy. Combination therapy showed not only a reduction in the relative risk of acute urinary retention or surgery for BPH, but also significantly better results than both monotherapies in reducing the risk of clinical progression of BPH. Data from the 4-year ComBat study support the use of combination therapy with tamsulosin and dutasteride in men with moderate to severe LUTS secondary to BPH [12]. Literature
1. Arrighi HM, Metter EJ, Guess HA, Fozard JL Natural history of benign prostatic hyperplasia and risk of prostatectomy. The Baltimore Longitudinal Study of Aging. // Urology 1991; 38(Suppl. 1): 4-8. 2. Emberton M., Andriole GL, de la Rosette J., et al. BPH. A progressive disease of the aging male. // Urology 2003; 61: 267-73. 3. Chapple CR: Medical therapy and quality of life. // Eur Urol 1998; 34(suppl 2): 10-17. 4. EAU Recommendations on Benign Prostatic Hyperplasia. Update March 2004. (Eds. J. de la Rosette., et al.). 5. Eckhardt MD, van Venrooij GE, van Melick HH, Boon TA. Prevalence and bothersomeness of lower urinary tract symptoms in benign prostatic hyperplasia and their impact on well-being. // J Urol 2001; 166:563-8. 6. Proceedings of the 4th International Consultation on BPH. Plymouth, Plymbridge Distributors Ltd, 1998, pp.669-684. 7. Djavan B., Marberger M. A meta-analysis on the efficacy and tolerability of alpha1-adrenoceptor antagonists in patients with lower urinary tract symptoms suggestive of benign prostatic obstruction. // Eur Urol 1999; 36:1–13. 8. Kumar R., Nehra A., Jacobson DJ, McGree ME, Gades NM, Lieber MM, Jacobsen SJ, St. Sauver JL Alpha-blocker use is associated with decreased risk of sexual dysfunction. // J Urol 2009 Jul;74(1):82-7. 9. McConnell JD, Bruskewitz R, Walsh PC, et al. The effect of finasteride on the risk of acute urinary retention and the need for surgical treatment among men with benignprostatic hyperplasia. //NEngl J Med 1998; 338:557-63. 10. Roehrborn CG, Boyle P., Nickel JC, Hoefner K., Andriole G. Efficacy and safety of a dual inhibitor of 5α-reductase types 1 and 2 (dutasteride) in men with benign prostatic hyperplasia. // Urology 2002; 60: 434-41. 11. Debruyne F., Barkin J., van Erps P., et al. ARIA3001, ARIA3002, ARIB3001 study investigators. Efficacy and safety of long term treatment with the dual 5-(-reductase inhibitor dutasteride in men with symptomatic benign prostatic hyperplasia. // Eur Urol. 2004, 46:488-494. 12. Roehrborn CG, Siami P., Barkin J. , Dami?o R., Major-Walker K., Nandy I., Morrill BB, Gagnier RP, Montorsi F., Comb AT Study Group. The effects of combination therapy with dutasteride and tamsulosin on clinical outcomes in men with symptomatic benign prostatic disease hyperplasia: 4-year results from the CombAT study. // Eur Urol (European urology) 2010 Jan;57(1):123-31.
Portal “Eternal Youth” https://vechnayamolodost.ru 12/28/2010
What happens during prostate surgery?
The most common type of prostate enlargement surgery is the so-called transurethral resection of the prostate (TUR). One of the most important arguments in favor of TURBT is the low incidence of complications and the avoidance of a surgical incision. The patient needs to spend no more than 3-5 days in the hospital.
The operation is performed using a device called a resectoscope. The device is inserted through the urethra to the prostate gland. The prostate gland is “cut” and removed.
During an open prostatectomy, an incision is made in the abdominal wall to access the prostate through the bladder. The advantage of this method is that it is possible to remove a large prostate. The disadvantage of this method is a higher number of possible complications, longer recovery and hospital stay.
After surgery, a histological examination of surgically obtained prostate tissue is always performed. If malignant prostate cancer is detected, it can be effectively treated if detected at an early stage.
How to treat this disease?
Treatment of prostate adenoma is divided into two large groups - surgical and conservative (with medications).
Regardless of the size of the adenoma, if there are good results (small volume of residual urine, high rate of urination, absence of complaints about urination), long-term drug therapy is possible.
Drug treatment
The main medications prescribed for the treatment of prostate adenoma include:
- Alpha-blockers - by relaxing the muscle component of the prostate and urethra, they reduce symptoms, but do not affect the volume of the prostate. However, these drugs can lower blood pressure and cause retrograde ejaculation (“dry orgasm”).
- 5 alpha-reductase inhibitors - by blocking this enzyme, they prevent the transition of testosterone to its more active form (dehydrotestosterone), which affects the growth of adenoma. This drug is used for prostate volume from 40 to 80 cm3. However, this group of drugs reduces libido (sex drive).
- The most commonly prescribed combination therapy is alpha-blockers + 5 alpha-reductase inhibitors.
- Herbal preparations, most often derivatives of plants from the Palm family. The mechanism of these drugs is similar to the group of 5 alpha-reductase inhibitors.
Surgery
It is carried out when conservative therapy is ineffective or intolerant.
Indications for surgical treatment are:
- Acute or chronic urinary retention;
- Hematuria (blood in the urine);
- Bladder stones;
- Hydronephrotic transformation of the kidneys (with a large amount of residual urine and impaired outflow of urine from the kidneys);
- Large bladder diverticulum;
- Progressive renal failure.
Currently, the gold standard for the treatment of prostate adenoma is endoscopic treatment methods:
- Transurethral resection of the prostate (TURP) . Unlike endoscopic enucleation, this operation is indicated for prostate volumes up to 80 cm3.
- Transurethral endoscopic enucleation of prostatic hyperplasia . This operation can be performed using thulium, holmium lasers (laser vaporization of prostate adenoma), bipolar electricity. Endoscopic enucleation is possible for any size of the prostate. Simultaneous cystolithotripsy (crushing stones in the bladder) is also possible. The entire period of hospitalization takes on average 3 days.
- For large prostate adenomas, open/laparoscopic adenomectomy . However, these operations, although they have good postoperative results, are inferior to endoscopic methods in the speed of postoperative rehabilitation.
Alternative methods of surgical treatment of prostate adenoma
Various alternative minimal intervention techniques have evolved significantly in recent years. This group includes various laser, ultrasound, and thermal methods.
These procedures result in significantly less stress on the patient, less hospital stay, and less risk of complications.
Their disadvantages are their higher cost and the small amount of prostate tissue that can be obtained for histological analysis.
Patients who do not respond to medications and surgery is contraindicated, for example due to a general condition or some other factor, require an indwelling catheter to allow urine to pass. For such cases, there are so-called prostate stents, which can be used temporarily or permanently.
Prevention
Methods and medications for the prevention of BPH are not yet well known. If you have BPH symptoms, it may be worth incorporating some lifestyle changes, such as avoiding drinking liquids in the evening, to reduce the frequency of nighttime urination.
The symptoms of prostatic hyperplasia are unpleasant and the quality of life of patients, commensurate with the severity of their complaints, certainly worsens. However, benign dysplasia is a very manageable condition.
Considering that the symptoms can also be associated with a more serious disease, for example, prostate cancer, with any signs of pathology, even if they are still tolerable, you should definitely seek medical help from a good urologist.
ONLINE REGISTRATION at the DIANA clinic
You can sign up by calling the toll-free phone number 8-800-707-15-60 or filling out the contact form. In this case, we will contact you ourselves.
If you find an error, please select a piece of text and press Ctrl+Enter
Vitamin E 400
Tocopherol acetate or vitamin E is often included in the complex treatment of prostate adenoma as an antioxidant, radioprotective agent and an indispensable link in reproductive processes.
Vitamin E in a dosage of 400 mg is prescribed by urologists to patients with disorders of erectile function and spermatogenesis associated with prostate adenoma. Treatment of such a serious chronic disease as prostate adenoma should be prescribed and monitored by a urologist. Taking certain medications on your own, without prior consultation with your doctor, is strictly prohibited, since self-medication in this case may not only be ineffective, but also dangerous for men’s health. Only a qualified specialist can tell you which tablets for prostate adenoma are the most effective in each specific case, and which of them can cause negative consequences.