Abdominal aortic aneurysm
An abdominal aortic aneurysm is an enlarged section of the lower aorta, the main blood vessel that carries blood throughout the body. The diameter of the aorta is about 2-3 cm, it passes through the center of the chest and abdomen. Because the aorta is the body's main blood supply, a ruptured aortic aneurysm can cause life-threatening bleeding.
Depending on the size and rate at which the aneurysm is growing, treatment can range from observation to emergency surgery. Once an abdominal aortic aneurysm is detected, your doctor will monitor its condition so that surgery can be planned if it is needed. Emergency surgery for a ruptured aortic aneurysm is very dangerous.
Symptoms
Abdominal aortic aneurysms often grow slowly and are usually asymptomatic, making them difficult to identify. Some aneurysms may never rupture. Many start out small in size and remain that way, although many expand over time. Others are expanding quickly. It is difficult to predict how quickly an abdominal aortic aneurysm will grow.
As the aneurysm gets larger, some people may notice:
- feeling of pulsation near the navel;
- deep, constant pain in the abdomen or side of the abdomen;
- lower back pain.
Causes
Most aortic aneurysms appear in the part of the aorta that belongs to the abdominal cavity. Although the exact cause of abdominal aortic aneurysms is unknown, many factors may play a role, including:
- Smoking tobacco.
Cigarette smoking and other forms of tobacco use increase the risk of aortic aneurysms. In addition to the harmful effects that smoking has directly on the arteries, smoking contributes to the accumulation of lipid plaques in the arteries (atherosclerosis) and high blood pressure. Smoking can also cause rapid growth of the aneurysm and subsequent damage to the aorta. - Hardening of the arteries (atherosclerosis).
Atherosclerosis occurs when lipids and other substances deposit on the inner wall of a blood vessel, increasing the risk of an aneurysm. - Infection of the aorta (vasculitis).
In rare cases, an abdominal aortic aneurysm may be caused by an infection or inflammation that weakens part of the aortic wall. - Aneurysms can develop anywhere along the aorta, but when they form in the upper part of the aorta, they are called thoracic aortic aneurysms. Most often, aneurysms form in the lower part of the aorta and are called abdominal aortic aneurysms.
Risk factors
Risk factors for abdominal aneurysm include:
- Age.
Abdominal aortic aneurysms occur most often in people over 65 years of age. - Smoking tobacco.
Tobacco smoking is a significant risk factor for the development of abdominal aortic aneurysm. The longer you smoked or chewed tobacco, the more likely you were to develop an aneurysm. - Atherosclerosis.
Atherosclerosis, the deposition of lipids and other substances that can damage the inner wall of a blood vessel, increases the likelihood of an aneurysm. - Male gender.
Men develop abdominal aortic aneurysms much more often than women. - Family history.
People who have a family history of abdominal aortic aneurysm are at increased risk. People who have a family history of aneurysms tend to develop aneurysms at a younger age and are at increased risk of aneurysm rupture.
Complications
Dissecting aneurysm - rupture of the aortic wall (dissection) is the main complication of an abdominal aortic aneurysm.
A ruptured aortic aneurysm can lead to life-threatening internal bleeding. In general, the larger the aneurysm, the greater the risk of rupture.
Signs and symptoms indicating a ruptured aneurysm:
- sudden intense and constant pain in the abdominal cavity or lower back;
- pain that radiates to the back or legs;
- sweating;
- sticky sweat;
- dizziness;
- nausea;
- vomit;
- low pressure;
- rapid pulse;
- loss of consciousness;
- dyspnea.
Another complication of aortic aneurysms is the risk of blood clots. Small blood clots may develop in the area of the aortic aneurysm. If a clot breaks away from the inside wall of the aneurysm and closes a blood vessel elsewhere in your body, it can cause pain or block blood flow to the legs, toes, kidneys, or abdominal organs.
Clinical manifestations
Many variants of localization and extent of dissection, the possibility of occlusion of various branches of the aorta give such a variety of clinical manifestations that they make their systematization quite difficult. The most typical symptoms are:
• sharp pain, most intense at the moment of occurrence, more often - behind the sternum, in the heart area, less often - in the interscapular region, epigastrium, lower back;
• motor excitement;
• shortness of breath;
• pale or bluish skin;
• increased blood pressure (higher values are typical for a low location of the dissection);
• hypotension (often the result of cardiac tamponade and aortic valve insufficiency);
• loss of consciousness;
• arrhythmia;
• pulse asymmetry;
• transient disturbances of sensitivity and movements in the limbs;
• visual and speech disorders.
Modern approaches to the treatment of abdominal aortic aneurysm
- Abdominal aortic aneurysm is detected annually in approximately 12 to 15 people out of 100,000, and due to the potential for rupture, increases mortality;
- Ultrasound or CT screening is recommended for men over 65 years of age who smoke, and for men over 50 years of age and women over 60 years of age whose parents or siblings have had an aortic aneurysm;
- It is recommended to operate on aneurysms with a diameter greater than 5 cm in women and 5.5 cm in men, or if the aneurysm has increased by 5 mm (or more) in less than 6 months;
- Endovascular surgery for abdominal aortic aneurysm is the treatment of choice in patients over 65 years of age, at high risk due to other diseases, and with previous aortic surgery.
In the hands of experienced surgeons, open aortic aneurysm surgery is safe and long-lasting in most cases, and is well suited for younger patients. During this operation, the aorta is clamped above and below the aneurysm, and the damaged area is replaced with a polyester patch.
Perioperative complications (including cardiac and pulmonary complications, incisional hernias, sexual dysfunction, paraplegia, and death) and recovery time when choosing traditional open surgery may have a poorer outcome in patients who are elderly or at high surgical risk.
Endovascular treatment of aortic aneurysm using an implantable stent is a safer alternative to open surgery. This procedure produces excellent results in patients with suitable anatomy.
Treatment technologies at the Innovative Vascular Center
Vascular surgeons at our clinic have significant experience in open operations for abdominal aortic aneurysms. They have performed more than 150 operations for this pathology with success in 95% of patients. The approach of our clinic is to thoroughly prepare a patient with an aneurysm to exclude pathology of the heart and carotid arteries, which may affect the outcome of the operation. To prevent renal complications, we use prolonged hemofiltration in the postoperative period. To reduce blood loss, hemodilution (blood dilution) and blood return equipment are used. In order to prevent complications in the postoperative period, we practice early getting patients out of bed and active rehabilitation. In recent years, we have been gradually moving away from open operations for aneurysms in favor of less traumatic endovascular endoprosthetics operations.
Control and treatment
- aneurysms are often asymptomatic;
- Abdominal aortic aneurysms are often discovered by chance during examination of the abdomen during radiography, computed tomography, ultrasound, performed for another purpose;
- if the aneurysm is small (4.5 cm in diameter) and there are no symptoms, annual duplex ultrasound examination is recommended;
- quitting smoking and controlling hypertension is the optimal prevention of the appearance and growth of aneurysms;
- It is recommended to operate on aneurysms with a diameter greater than 5 cm in women and 5.5 cm in men, or if the aneurysm has increased by 5 mm (or more) in less than 6 months.
The procedure is performed through small incisions in the femoral arteries. After puncture of the femoral artery, the guidewire is passed through the dilated part of the aorta, then the stent is advanced along the guidewire. Once the stent is positioned correctly, the balloon expands and the stent pushes the vessel wall apart to prevent the aneurysm from spreading below the renal arteries.
To ensure proper sealing between the implanted stent and the aorta, most currently available stents require that the aneurysm have a proximal isthmus at least 1.0 to 1.5 cm below the renal arteries. However, surgery can be done in patients with aneurysms whose aneurysm isthmuses are shorter or absent altogether, by implanting a stent with multiple holes and branches into the arteries of the kidneys or intestines.
Suitable iliac artery conditions are required for guidewire placement, but the potential placement of a stent through a small retroperitoneal incision has increased the number of candidates for endovascular surgery
Compared to traditional open surgery, endovascular surgery has several advantages:
- reduction of operation time;
- reducing blood loss and the need for infusions;
- reducing the time of treatment in the intensive care unit and hospital stay;
- reduced risk of complications;
- Less contrast is used and often less than 60 ml of contrast is required during the procedure;
- intraoperative and early (up to 30 days) mortality are also lower for endovascular operations than for open ones.
The average stay after open surgery is approximately 3 days in the intensive care unit, followed by 7-10 days in the ward, with recovery taking 8-12 weeks.
Most patients undergoing endovascular surgery do not require hospitalization in the IT department and can be sent home the next day after surgery. A larger percentage of patients who have undergone endovascular surgery are sent straight home rather than to rehabilitation sanatoriums. These patients return to normal levels of physical activity more quickly; the rehabilitation period is 1-2 weeks.
In patients with minor comorbidities who are candidates for endovascular intervention, some complications specific to this method may also occur. It is extremely rare to switch to open surgery. Problems associated with stent placement occur in 5-10% of patients and require CT or ultrasound monitoring
Displacement of the stent is rarely possible, because Newer generation stents have hooks and deploy above the level of the renal arteries for better fixation. “Leaks”—when blood leaks between the stent and the aortic wall—occur in 5-10% of cases. Most of them are type II “leaks” - blood continues to accumulate in the aneurysm from the lumbar artery. If there is growth of the aneurysm, patients are not considered cured; in this case, under local anesthesia, the lumbar arteries are closed by embolization on an outpatient basis.
With proper monitoring, the risk of subsequent rupture is extremely low. Therefore, patients should be prepared to undergo further evaluation, which includes computed tomography of the endovascular stent 4 to 6 months after surgery and annually thereafter. Other less common complications are stent failure or infection.
The current prognosis for healthy patients who undergo aneurysm surgery is excellent. Endovascular surgery is a remarkable advance in the treatment of patients with suitable anatomy and is the preferred treatment option for high-risk and elderly patients.
Postoperative period
After surgery, the recovery period takes 3-4 weeks. The patient undergoes regular examinations; cardiologists monitor the functioning of the heart and aorta. Depending on the technique of the intervention performed and the size of the aortic aneurysms, clinical recommendations suggest minimal physical activity only under medical supervision.
Physical therapy with the use of special simulators is indicated so that the heart and blood vessels learn to work in new conditions (with a stent or shunt). After a month, if there are no complications after surgery, the patient can return to the pre-operative lifestyle. It is recommended to reduce physical activity and the amount of fatty foods in the diet so as not to provoke the development of atherosclerosis.
Treatment and drugs
Here are the general guidelines for treating abdominal aortic aneurysms.
Small aneurysm
If you have a small abdominal aortic aneurysm—about 4 cm in diameter or smaller—and you have no symptoms, your doctor may suggest observation rather than surgery. In general, small aneurysms do not require surgery because the risk of surgery may outweigh the risk of rupture.
If you choose this approach, your doctor will monitor your aneurysm with periodic ultrasounds, usually every 6-12 months; You should report immediately if you experience abdominal tenderness or lower back pain—potential signs of rupture.
Average aneurysm
The average aneurysm measures between 4 and 5.3 cm. It is impossible to say for sure in the case of a medium-sized abdominal aortic aneurysm the risk ratio between rupture and surgery. You will need to discuss the pros and cons and make a decision with your doctor. If you choose surveillance, you will need to have ultrasound scans every 6 to 12 months to monitor your aneurysm.
A large, fast-growing, or “leaky” aneurysm. If you have an aneurysm that is large (greater than 5.6 cm) or rapidly growing (growing more than 0.5 cm in six months), then you will likely need surgery. In addition, a “leaking”, thinned or painful aneurysm requires treatment. There are two types of surgery for abdominal aortic aneurysms.
Open abdominal surgery for an abdominal aortic aneurysm involves removing the damaged section of the aorta and replacing it with a synthetic tube (prosthesis) that replaces the damaged section through an open approach to the abdominal cavity. With this type of intervention, you will likely need a month or more to recover.
Endovascular surgery is a less invasive procedure and can be used to repair an aneurysm in some cases. The doctor uses a synthetic implant, which, with the help of a guide (catheter), is passed through an artery in the thigh into the aorta. The implant—a fabric tube covered with a metal support mesh—is placed at the site of the aneurysm and secured with small hooks. The tissue implant strengthens the weakened part of the aorta and prevents rupture of the aneurysm.
Recovery time for people who undergo endovascular surgery is shorter than for people who have open abdominal surgery. However, more frequent examinations will be required in the future because an endovascularly placed implant may leak. Follow-up ultrasounds should be performed every six months for the first year, and then once a year thereafter. Long-term survival rates are similar for both endovascular surgery and open surgery.
Treatment options for your aneurysm will depend on many factors, including the location of the aneurysm, your age, kidney function, and other conditions that may increase your risk of endovascular or open surgery.
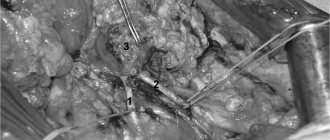
Progress of the aortic aneurysm resection operation
- Surgical approach
During the preoperative examination, a decision is made regarding the surgical approach. Most often, three accesses are performed. Two of them are in the groin area on the thigh, to isolate the common femoral arteries, one access is a median laparotomy (an incision in the middle of the abdomen) or an access on the left side. For tall aneurysms, the superior approach can be extended into the chest. This intervention is thoracophrenolumbotomy.
- The meaning of the operation
After isolating the aneurysmal sac, the abdominal aorta is clamped. The time for blocking blood flow must be reduced. To do this, before installing the clamp on the aorta, a good isolation of the aneurysm and all arterial branches up to the bifurcation of the aorta into the iliac arteries is performed. When vascular clamps are applied, the lumen of the aneurysm is opened, thrombotic clots are removed from the aneurysm cavity and bleeding from the branches flowing into the aneurysm is stopped.
Open intervention consists of replacing the enlarged section of the aorta with a synthetic vascular prosthesis. The latter is sewn into the upper section of the aorta (above the aneurysm), then the branches of the prosthesis are carried to the femoral arteries and sewn to them. After this, the prosthesis is covered with the walls of the aneurysmal sac. The main problem is the identification of the aneurysmal sac and the branches emanating from it. This must be done quickly enough if these branches are passable, since prolonged compression can cause disruption of the nutrition of the intestine or spinal cord.
After connecting the aorta to the femoral arteries, it is necessary to decide on the need for transplantation of the inferior mesenteric artery. This artery supplies blood to the colon, and sometimes ligating it can lead to disruption of the intestinal blood supply. To make a decision, it is necessary to evaluate the blood flow through this artery. If, after removing the clamp, there is good reverse blood flow, then the artery does not need to be sutured to the vascular prosthesis; if it is passable, but the blood flow is very weak, then the bypass paths are undeveloped and the arteries need to be replanted into the vascular prosthesis.
After completion of the vascular stage of the operation, tubular drains are installed in the retroperitoneal space and in the access area on the thighs, and the wounds are sutured layer by layer.
The average duration of surgery for an aortic aneurysm is 3 hours. The average volume of blood loss is about one liter. Blood loss is replenished with donor blood, plasma and saline solutions.
Lifestyle and Home Remedies
The best way to prevent an aortic aneurysm is to keep your blood vessels as healthy as possible. To do this, you can take the following steps:
- quit smoking;
- keep your blood pressure under control;
- get checked regularly;
- reduce the amount of cholesterol and fat in your diet.
If you think you may have an abdominal aortic aneurysm, or are concerned about your risk of an aneurysm due to a family history, see your doctor. If an aneurysm is detected early, treatment may be easier and more effective.