Every adult has encountered the diagnosis of “otitis media”: if he was not sick himself, then he treated his child for the disease.
“Otitis” is a collective concept that characterizes the course of the inflammatory process in the ear.
Any of its parts can become inflamed. The structure of our ear is not as simple as it seems. This is a complex mechanism that performs an important function. It consists of three parts: the outer ear, the middle and the inner.
The outer is the visible part of the ear. We most often think of the auricle when we mean the ear. Although its role in the complex process of sound perception is minimal. It only picks up sound waves and transmits them further to the middle section. The outer ear is separated from the middle ear in adults and children by the eardrum.
The middle section is responsible for sound transmission. The eardrum transmits sound vibrations into the tympanic cavity, where they are amplified. The auditory ossicles are located here: the malleus, the incus and the stapes. The malleus is connected to the eardrum. The sound wave bends the eardrum, and this vibration is transmitted to the hammer, and from it, further along the chain from one auditory ossicle to another, the signal is transmitted to the internal part of the hearing organ.
The inner ear is located in the temporal bone and is a collection of canals. Due to its similarities, it is also called a labyrinth. Hair cells are located in these channels. Each specific cell perceives a certain frequency of sound. Hair cells pick up sound vibrations and convert them into nerve impulses. The impulse is sent directly to the brain.
Inflammation can affect each of the three parts of the ear; accordingly, there are three types of otitis media: external, middle or internal.
Adults and children, for the most part, have to deal with otitis media.
Make an appointment right now!
Call us by phone or use the feedback form
Sign up
Types of otitis media
Inflammation of the middle ear in adult patients and in childhood can occur in acute and chronic forms. Acute otitis media begins, as a rule, suddenly: with unpleasant sensations in the ear, which increase over a short period of time, the pain becomes more intense. An adult patient describes his condition as follows: “There’s a shooting in the ear!” If the disease begins in a child, the baby begins to scream furiously and fiddle with his ear. Pus accumulates in the ear. Only when the eardrum ruptures and purulent contents exit the middle ear cavity does relief occur.
With chronic otitis media, the signs of the disease are less pronounced. Chronic otitis media is more sluggish. The diagnosis is made when the disease lasts from six to ten weeks in an adult or child or exacerbations recur more than four times a year.
Otitis media usually manifests itself as a complication of other infectious diseases.
Chronization begins mainly in cases where treatment of the middle ear for acute otitis was untimely or was carried out with incorrectly selected medications.
Another mistake in the treatment of acute otitis is the incorrect use of drugs, when adult patients, having felt relief, stop taking medications. And an incomplete course of taking medications is a direct path to chronicity of the inflammatory process. Therefore, the disease should be treated fully by contacting an ENT doctor in time.
Causes of chronic otitis media.
Catalysts for exacerbation of a chronic disease can be:
- infectious diseases;
- chronic diseases of the ENT organs (rhinitis, sinusitis);
- prolonged nasal congestion;
- adenoids;
- damage and trauma to the ear;
- eustachitis;
- enlarged nasal turbinates;
- weak immunity;
- lack of vitamins;
- hypothermia;
- improper ear hygiene.
It is much easier for children to get sick - the Eustachian tube connecting the nasopharynx to the ear is very short, so the infection easily penetrates from the nasal cavity to the ear cavity.
Provoking factors can be improper blowing of the nose or rinsing the nose at home, for example, with sinusitis, when, due to inept actions, the infection penetrates into the ear, causing inflammation there.
To prevent exacerbation of chronic otitis, it is necessary to contact an otolaryngologist in time and treat the cause of the disease.
Signs and symptoms of chronic suppurative otitis media
Typically, patients with chronic suppurative otitis media or chronic otitis media present the following complaints:
- periodic or constant suppuration from the ear,
- hearing loss,
- recurrent ear pain,
- a feeling of noise in the ear,
- dizziness.
However, in some cases, these symptoms may be absent or mild. The causes of exacerbation of the process may be a cold, water getting into the ear, a common runny nose, diseases of the nose and nasopharynx. With exacerbation of the disease, suppuration intensifies, body temperature may rise, noise intensifies or appears, and mild pain in the ear.
Symptoms
Due to the sluggish course of the disease, adult patients do not always realize that they have problems until they notice problems with hearing or the exacerbation phase begins. Symptoms in the chronic form:
- pain in the affected ear, worsening at night;
- hearing loss;
- elevated body temperature in the absence of other cold symptoms;
- purulent discharge from the ear canal in a purulent form, sometimes the discharge produces a foul odor;
- noise in ears;
- headache;
- If purulent otitis media has developed, the adult patient is haunted by the feeling that fluid is overflowing in the ear.
Chronic disease occurs in waves: periods of exacerbation are followed by periods of rest (remission).
During an exacerbation, children become lethargic, capricious, and their performance at school decreases.
During remission, symptoms subside. The patient may note that his hearing has decreased. But a person quickly gets used to this state.
If the disease is not treated at this stage, the consequences can become much more serious. Inflammation can affect the labyrinth of the ear. If the purulent process spreads to areas of the brain, meningitis may develop.
If left untreated, the disease gradually destroys the auditory ossicles and, as a result, leads to severe hearing loss. It will be impossible to completely restore your hearing.
Friends! Timely and correct treatment will ensure you a speedy recovery!
Causes
The most common causative agents of otitis media are staphylococci, streptococci, and Haemophilus influenzae; other bacteria, as well as viruses and fungi, are somewhat less common.
The occurrence of CHSO occurs, as a rule, after insufficient treatment of acute otitis of any localization
. In most cases, this is facilitated by injury or rupture of the eardrum, which leads to massive infection from the outer ear. Chronicity of the inflammatory process is often observed in immunodeficiency states, in the presence of pathology of the nasal mucosa, paranasal sinuses and nasopharynx, in the case of long-term treatment that suppresses the immune system (large doses of glucocorticosteroids, antiallergic, cytostatic therapy).
Types of chronic otitis
There are two types of chronic otitis: mesotympanitis and epitympanitis.
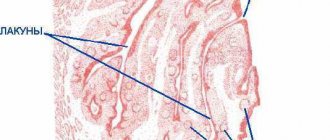
In the first case, the inflammatory process covers the mucous membrane of the middle ear and the eardrum. Perforation in the tympanic membrane occurs approximately in its center. The membrane itself thickens and becomes covered with pus. Purulent processes do not subside. Polyps form on the mucous membrane, which periodically bleed. The tympanic cavity gradually fills with pus, which provokes the destruction of the auditory ossicles and a gradual decrease in hearing.
Epitympanitis is a more severe manifestation of chronic inflammation. It affects not only the mucous membrane, but also bone tissue. The perforation in the eardrum is located close to its edge. Benign tumor-like formations are formed - choleastomas. Choleastomas and polyps block the tympanic cavity. The release of pus becomes difficult. As they grow, choleastomas begin to grow into the bone tissue, gradually destroying them. This type of inflammation affects the cranial bones, labyrinth of the ear and brain.
The consequences of this condition are quite serious, so there should not even be any doubt about whether to treat or not treat this disease.
Causes of chronic suppurative otitis media (CSOM)
Chronic purulent otitis media is the result of an advanced form of acute otitis media or its insufficient treatment, in which the formed post-inflammatory changes in the mucous membrane and structures of the middle ear contribute to the chronicity of the process. Persistent damage to the integrity of the eardrum can be caused by a number of other external factors, including chemical exposure or mechanical damage due to injury.
The development of CHSO is caused by various factors, including a decrease in the general immune status of the body, the presence of concomitant diseases of the body, virulent strains of pathogens resistant to antibacterial drugs, disruption of reparative processes, dysfunction of the auditory tube, etc. The development and maintenance of CHSO can also be facilitated by a deviated nasal septum, the presence adenoid vegetations.
Diagnostics
Timely diagnosis will help prevent the development of complications and start treatment of chronic otitis in a timely manner. If signs of the disease occur, you should make an appointment with an otolaryngologist for diagnosis and effective treatment.
To make a diagnosis, the following is carried out:
- otoscopy (standard examination of the hearing organ);
- blood analysis;
- if necessary, radiography or computed tomography;
- culture of discharge from the ear canal;
- audiometric study to determine the degree of hearing loss.
In the diagnostic process, it is necessary to differentiate mesotympanitis from epitympanitis. This is important when prescribing competent treatment.
Complications and consequences
- Mastoiditis (inflammation of the mastoid process of the temporal bone) - characterized by swelling, swelling of the post-auricular area.
- Intracranial complications (meningitis - inflammation of the dura mater, encephalitis - inflammation of the brain substance, brain abscess - a localized abscess in the brain) are characterized by a severe general condition, severe headache, and the appearance of brain symptoms (neck tension, vomiting, confusion, etc.).
- Thrombosis of the sinuses (cavities in the dura mater in which venous blood collects). In this case, there is a severe headache, exophthalmos (bulging eyes), convulsions, coma (lack of consciousness) and other severe disorders of the nervous system.
- Neuritis of the facial nerve (inflammation of the facial nerve) – manifested by facial asymmetry, impaired mobility of half the face;
- Otogenic sepsis is a generalized infection spread to various organs and tissues through the bloodstream;
- Cholesteatoma is a formation consisting of cells of the upper layer of the skin of the external auditory canal, which grow into the tympanic cavity through a perforation (defect) of the eardrum. May destroy surrounding tissue, including bone.
- Irreversible hearing loss;
- Risk of death.
How to treat the disease?
Chronic otitis media is treated conservatively or surgically, depending on the type of inflammation.
Conservative treatment includes the use of medications, rinsing the ear from purulent accumulations and physiotherapeutic procedures.
Treatment is carried out on an outpatient basis except in clinical cases when there are life-threatening complications or the patient is young (up to 2 years). Indications for the need to treat otitis in a hospital are meningitis, facial paralysis, and brain abscess. If otitis media is not treated, the following may develop: thrombosis, sepsis, mastoiditis. You can also permanently lose your hearing.
Drugs for the treatment of otitis, as well as a complete treatment regimen, are prescribed by an otolaryngologist based on their clinical picture, because mesotympanitis and epitympanitis are treated differently.
Treatment of mesotympanitis
Mesotympanitis is the mildest form of chronic inflammation. Therefore, therapy for this diagnosis is conservative - the disease is treated with medications.
The first stage of therapy is to stop the discharge of purulent masses. For this purpose, the ear cavity is washed. Before rinsing the ear with medications, the ENT doctor cleans the auricle, then cleans the ear canal with a probe, and cleans the middle ear. At the end of all these manipulations, medications are injected into the ear. Antibacterial, anti-inflammatory, and antihistamine drugs are injected into the washed ear.
To restore the integrity of the tympanic membrane, physiotherapeutic procedures are carried out. The complex of physical procedures includes ultraviolet irradiation, laser therapy, ultrasound and photodynamic therapy sessions. To restore hearing, treatment is carried out using electrical pulses in combination with infrared laser radiation using the Audioton apparatus.
In combination with drug therapy, physiotherapy relieves inflammation and the symptoms of the disease disappear.
In those rare cases when conservative therapy does not help, it is necessary to open the tympanic cavity surgically and then perform plastic surgery of the tympanic membrane.
GBOU "NIKIO im. L.I. Sverzhevsky" of the Moscow Department of Health
Chronic suppurative otitis media means chronic inflammation of the middle ear. Chronic inflammation is a consequence of acute inflammation; Many factors contribute to the transition of acute or subacute inflammation to chronic, such as, for example, a decrease in the general resistance of the body, the presence of chronic tonsillitis (and in children, adenoiditis), chronic inflammation of the paranasal sinuses (sinusitis), chronic catarrhal or vasomotor rhinitis, nasal dysfunction breathing and patency of the auditory tube, etc. To cure a patient from chronic inflammation of the ear, it is necessary first of all to sanitize the nose and pharynx and restore nasal breathing.
In its course, it is always accompanied by discharge from the ear and hearing loss, and sometimes by severe intracranial and labyrinthine complications. For a long time, without affecting hearing, chronic otitis media does not cause concern in patients and reduces their alertness to the need for early elimination of a purulent focus of infection in the middle ear. That is why broader public information about the characteristics of chronic inflammation of the middle ear is needed. To understand them, you need to have some understanding of the structure (anatomy) of the middle ear.
The middle ear, which has the shape of an irregular tetrahedral prism filled with air, is located in the temporal bone and communicates with the air of the nasopharynx through the auditory tube. The eardrum separates the middle ear from the external auditory canal. For the most part it is stretched like a drum; only a small upper part of it is relaxed. The central part of the middle ear is the tympanic cavity; An auditory tube is located in front of us, and a cave (antrum) is located behind us. The cave is a large air cell in the temporal bone, communicating with the tympanic cavity. In a healthy ear, in the temporal bone, in addition to the cave, there are many other small air cells (cells), which all communicate with the cave. If otitis media (acute and, especially, chronic) develops in early childhood, then these small air cells, except for the cave, do not develop. An important structure of the middle ear is the 3 auditory ossicles, connected by small joints. The first bone - the malleus - is tightly fused with the eardrum, and the third - the stapes - with the inner ear (labyrinth) through the oval window, with the walls of which the stapes is connected by a thin ligament along the entire perimeter of its base. The inner ear has another window - a round one, closed by a durable membrane that separates the inner ear from the middle ear. Both windows are close to the nerve cells, the sound-receiving cells of the cochlea. All formations of the middle ear are covered with a mucous membrane that extends, as it were, from the nasopharynx into the middle ear. One of the features of the anatomical structure of the middle ear is the presence of small narrow spaces, especially in the upper and posterior parts of the tympanic cavity, formed by the auditory ossicles, ligaments and folds of the mucous membrane. With inflammatory swelling of the mucous membrane, these spaces are early isolated from the general tympanic cavity and become inaccessible for drug treatment. Another feature of the middle ear is the close proximity of the inner ear, which favors the penetration of toxic inflammatory products (and some toxic drugs, such as streptomycin, neomycin) into it and damage to auditory nerve cells. And finally, the third feature is the close location of the cranial cavity with all its structures, which are separated from the middle ear by a thin layer of bone tissue. This facilitates the penetration of infection into the brain tissue during purulent destruction of the dividing bone.
Chronic suppurative otitis media is characterized by discharge from the ear of a purulent, mucous or mucopurulent nature, which can be abundant or scanty, constant or periodic, with long or short intervals. The eardrum is always destroyed - partially or completely. Depending on the location of the membrane defect, it is customary to distinguish between mesotympanitis, epitympanitis and meso-epitympanitis. Mesotympanitis is characterized by perforation in the tense part of the eardrum and predominant inflammation of the mucous membrane; in this case, discharge from the ear can be abundant (less often scanty) and mucous, viscous in appearance. Sometimes polyps of the mucous membrane grow. With epitympanitis, the upper loose part of the membrane is destroyed; discharge from the ear is usually purulent (profuse during exacerbation), with an unpleasant odor; in this case, bone tissue is quickly destroyed and cholesteatoma develops from the skin epidermis of the auditory canal. Once a cholesteatoma appears, it does not stop growing. The skin epidermis seems to grow into the cavity of the middle ear and continues to grow constantly, regardless of whether there is an exacerbation of inflammation or not, however, during exacerbations, the growth of cholesteatoma is more rapid and granulations are always formed, which serve as an indicator of the destruction of bone tissue. This cholesteatoma-granulation process can lead to meningitis, brain abscess or vestibular vertigo. Mesoepitympanitis has all the signs of mesotympanitis and epitympanitis; They are characterized by a very long course of otitis media (tens of years).
The main difference between mesotympanitis and epitympanitis is that the former are characterized by intense inflammation of the mucous membrane, and the latter are characterized by damage to bone tissue and the growth of cholesteatoma.
With mesotympanitis, the auditory ossicles can be preserved and mobile for a long time, and therefore hearing remains almost normal for a long time; Only after many years (sometimes 10-15) the connection between the bones can be disrupted, which leads to a sharp deterioration in hearing. Slower development of hearing loss may be a consequence of gradually developing immobility of one bone (usually the stapes) or all bones. The degree of hearing loss in different patients with mesotympanitis is not the same, which depends on many reasons: on the location and size of the perforation of the eardrum, on the degree of mobility of the auditory ossicles, their preservation, etc. This hearing loss, caused by a violation of the sound conduction path, is called conductive, i.e. conductive. At the same time, with prolonged inflammation of the mucous membrane in the tympanic cavity, the products of the inflammation itself and the vital activity of microbes, as well as some medications, can penetrate into the inner ear and lead to toxic damage to the auditory nerve cells, i.e., cochlear neuritis. The layering of nervous hearing loss on conductive hearing loss is expressed by a high degree of hearing loss. In these cases, there is very little chance not only of successful hearing-improving surgery, but also of good hearing protection with the help of a hearing aid.
Anyone who uses a cotton swab soaked in petroleum jelly to improve their hearing often asks: “Why can’t I have hearing-improving surgery if such a swab improves my hearing?” The very fact of improved hearing in such cases suggests that the structures of both windows of the inner ear are mobile; and this fact in itself serves as an indication for hearing-improving surgery. However, in the middle ear there may be such large irreversible changes in the mucous membrane and auditory tube, large destruction of the eardrum, that it is impossible to create a new tympanic cavity, which must be isolated from the auditory canal and must be connected through a functioning auditory tube to the nasopharynx. But even if a hearing-improving operation cannot be performed, it is necessary to sanitize the middle ear and eliminate inflammation so that sensorineural hearing loss does not develop further.
In patients with epitympanitis, hearing can also remain normal for a long time, since the upper part of the eardrum, which is destroyed in this case, takes a small part in conducting sound. And only in cases where cholesteatoma spreads to the auditory ossicles and destroys them, hearing decreases sharply. Usually only in this case, patients are concerned about the condition of their ear and persistently look for ways to improve their hearing. Meanwhile, as with mesotympanitis, hearing-improving surgery sometimes becomes impossible. And since cholesteatoma in its aggressive growth poses a danger to life, the patient is offered only
sanitizing operation due to the failure of non-surgical, conservative treatment.
Lack of awareness of patients about chronic suppurative otitis media is often the reason for late seeking medical help. Patients themselves often put various drops into the ear only because a neighbor or someone else has used them successfully. But they may be indicated for some, and contraindicated for others. Self-medication is unacceptable, because it is often incorrect and can even lead to deafness. It should be remembered that conservative treatment can reduce the exacerbation of chronic inflammation, but it very rarely eliminates it completely. Drugs cannot penetrate isolated small areas of inflammation; In addition, with long-term inflammation, irreversible changes occur in the tissues of the middle ear. Long-term conservative treatment may be justified only in patients with no prospects for hearing loss.
improving surgery, and the inflammatory process in the middle ear does not threaten life or the development of sensorineural hearing loss. One can only regret that so many patients
it is necessary to refuse hearing-improving surgery due to late presentation and limit oneself to a sanitizing operation.
For any inflammation of the middle ear, the patient should consult a doctor for help. Active and proper treatment of acute inflammation of the middle ear ensures that it does not become chronic. And with chronic inflammation, surgical sanitation of the ear is necessary as early as possible if conservative treatment is completely unsuccessful or leads only to temporary improvement. The earlier the sanitizing operation is performed, the smaller it is in volume and the greater the chances of its success. And the later it is performed, the larger it is in volume and the less chance there is of a complete cessation of discharge and the possibility of then performing a hearing-improving operation.
Treatment of epitympanitis
This form of the disease initially requires surgical intervention. The presence of choleastomas and affected bone tissue is a direct indication for surgical intervention. The intervention is contraindicated for elderly people and patients with heart pathologies and kidney diseases.
The operation is performed under general anesthesia through an incision behind the ear. During the operation, purulent accumulations, affected areas of bone tissue, polyps and choleastomas are removed from the tympanic cavity. If the malleus, incus and stapes are partially destroyed during the course of the disease, prosthetics are performed.
Postoperative rehabilitation therapy does not require a long hospital stay. Dressing changes and restorative procedures can be performed on an outpatient basis in an ENT clinic.