Everyone is familiar with the unpleasant condition of a cold, when the nose is constantly stuffy. According to statistics, an ordinary person gets a runny nose more than 100 times from birth to old age. It is interesting that of all the diseases in Russia, every third is a respiratory disease, and every seventh is a cold (rhinitis, sinusitis, etc.).
Runny nose (rhinitis) is a common disease of the upper respiratory tract, transmitted by airborne droplets. One of the main factors in the development of rhinitis is hypothermia, it reduces the body's defenses, provokes the proliferation of microbes in the nose and nasopharynx and leads to nasal congestion.
Another factor related to rhinitis is a decrease in immunity after suffering from chronic diseases.
1 Diagnostics of rhinitis in MedicCity
2 Endoscopy of the nasal cavity in MedicCity
3 Diagnostics of rhinitis in MedicCity
Clinical picture of rhinitis
Rhinitis can be part of an acute respiratory infection and the beginning of an allergic reaction.
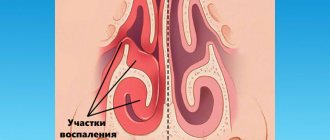
The disease begins with a deterioration in the general condition of the body, headache, weakened sense of smell, and it becomes difficult for a person to breathe through the nose. The nose may also be stuffy, pathogenic microflora begins to develop in it, and first clear, then green and brown nasal discharge appears.
If you have a fever and a stuffy nose, it could be rhinitis!
Symptoms of rhinitis:
- severely stuffy nose;
- nasal discharge (watery, mucous or mucopurulent);
- mucus running down the back of the throat;
- sleep disturbance;
- snore;
- headache.
A lot can be said about rhinitis, but the primary task of treating chronic rhinitis is to eliminate the causes that support the chronic inflammatory process of the nasal mucosa.
Why does my nose get stuffy? Causes:
- chronic inflammation of the paranasal sinuses;
- deviated nasal septum;
- anomalies in the structure of the nasal concha;
- adenoid vegetations, etc.
In such cases, normal air circulation is disrupted, pathological discharge flows into the nasal cavity, irritates the mucous membrane and maintains a chronic runny nose.
Ozena
Ozena is a chronic atrophic fetid runny nose, which differs from a simple atrophic runny nose by deep atrophy of the entire mucous membrane, bone walls of the nasal cavity and nasal turbinates. Ozena is characterized by the secretion of a thick secretion that dries into foul-smelling crusts.
Despite the fact that the disease has been known since ancient times, the etiology and pathogenesis of ozena continue to remain insufficiently understood to this day. It is now recognized that in the pathogenesis of ozena, a significant role is played by hereditary-constitutional characteristics, transmitted by inheritance as a recessive trait, as well as environmental conditions, incl. nutritional and vegetative insufficiency. As a result, a patient with ozena develops various neuroendocrine, neurovegetative and neurotrophic disorders. The central links that form these disorders probably involve the hypothalamic-pituitary department of the central nervous system.
Clinic and symptoms of ozena
The disease usually begins at a young age, women are more often affected. After the onset of menopause, many clinical manifestations of ozena decrease, which is the basis for considering this disease as being associated with dysfunction of the endocrine glands.
Patients with ozena are characterized by severe atrophy of the nasal mucosa and a decrease in the size of the nasal turbinates, especially the lower ones. Sometimes the lower shells atrophy faster than the middle ones, and therefore the latter appear unusually large against the background of the small atrophied lower ones. As a result of atrophy of the mucous membrane and nasal turbinates, the nasal cavity becomes wide. Often during ozena, the entire nasal cavity is filled with crusts. They usually have a yellowish-greenish, brownish or dirty color and are easily removed in the form of casts. At the same time, the outer surface of the crusts is dry, and the lower surface is viscous, thick, and an extremely unpleasant fetid odor emanates from it, which is a mixture of indole, skatole, phenol, hydrogen sulfide and volatile fatty acids. Actually, of all the objective signs of ozena, stench (kakosmiaobjectiva) should be placed in first place, as the constant and most significant objective symptom. However, patients suffering from anosmia do not feel this smell. It is the stench emanating from ozena patients that makes it impossible for them to communicate closely with other people, determines the tragedy of their situation and puts ozena patients in the position of outcasts of society. All this allows us to consider ozena as a disease of social significance.
Atrophic phenomena during ozena affect not only the nasal cavity, but also the paranasal sinuses and underlying respiratory tract. The crusts filling the nasal cavity spread posteriorly into the nasopharynx and pharynx, closing the mouths of the auditory tubes. Unfavorable conditions are created for ventilation of the tympanic cavity, which contributes to its involvement in the inflammatory process. This is the reason for the often observed damage to the hearing aid in patients with ozena.
Treatment of ozena
Treatment of ozena, as well as other degenerative processes of the nose, is one of the most difficult problems of rhinology. In recent years, however, pathogenetically based conservative and surgical treatment methods have appeared, combined with the use of etiotropic drugs that directly affect Klebsiella ozena. However, symptomatic treatment methods aimed at removing fetid crusts and deodorizing the nasal cavity have not lost their importance and continue to remain in the arsenal of modern rhinologists.
Based on the infectious hypothesis of the etiology of ozena, antibiotics active against Klebsiella ozena are used in treatment. However, these treatment methods do not allow obtaining lasting clinical results.
In the treatment of ozena, surgical methods are mainly used. Thus, based on the idea that dystrophic (atrophic) processes in the nasal cavity develop as a result of a violation of the trophic function of the autonomic nervous system, a synthetic implant (polyurethane, ivalon, etc.) is implanted in the area where the diffuse autonomic ganglion of the nasal septum is located. Inserting a graft into the area of the autonomic ganglion aims to have a positive effect on the trophism of the nasal mucosa. The described surgical method allows for clinical recovery (i.e., cessation of drying of foul-smelling crusts and revitalization of the mucous membrane) in 75% of cases.
Also, at the discretion of the doctor, a conservative method can be used, based on the use of cholinomimetics, anticholinesterase drugs, vitamins E and D, long-acting nitrites, stimulants of tissue regeneration, in particular, metacil. This treatment is carried out for 1 month in a hospital setting.
Acute rhinitis
Acute rhinitis is one of the most common diseases in childhood. Every mother is familiar with its symptoms: the child’s nose is stuffy, runny nose, etc.
Acute rhinitis has an infectious form, caused by viruses or bacteria. The disease can manifest itself as a separate disease of a viral or bacterial nature or be a component of infectious diseases such as influenza, ARVI, scarlet fever, meningitis, diphtheria, etc.
Provoking factors for acute rhinitis are hypothermia, polluted air, decreased human immunity, allergies, adenoids, and hypertrophic rhinitis. Therefore, if the nose is constantly stuffy, the child clearly has weak immunity, and it needs to be improved!
Symptoms of acute rhinitis:
The disease occurs in 3 stages:
- discomfort in the nose, itching, sneezing, tears, headache, malaise, fever (within 1-2 days);
- the nose is stuffy, it becomes difficult for the patient to breathe, hoarse voice, watery discharge from the nose, decreased sense of smell;
- The nasal discharge becomes thick and purulent, and the patient is bothered by severe nasal congestion.
1 Consultation with an otolaryngologist in MedicCity
2 Consultation with an otolaryngologist in MedicCity
3 Consultation with an otolaryngologist in MedicCity
Methods for getting rid of rhinitis
Treatment should begin only after studying the symptoms of a chronic disease, conducting a full diagnosis and establishing the form of the disease. Such precaution is really necessary, because for different types of rhinitis, different treatment techniques are used.
Therapy for catarrhal rhinitis
If such a form of the disease is detected, symptomatic and pathogenetic treatment is carried out. The first is to alleviate the patient's condition with the help of individual drugs. Doctors prescribe vasoconstrictors to relieve congestion. However, their use is limited to 3–5 days due to the risk of provoking the development of drug-induced rhinitis. Therefore, at the same time, it is important to carry out pathogenetic therapy aimed at getting rid of the disease.
Complex treatment involves taking the following medications:
- Antibiotics. The most effective drugs for chronic rhinitis are the cephalosporins and tetracyclines.
- Antiallergic drugs.
- Glucocorticoids.
- Various reparants and regenerators.
The selection of medications, calculation of dosage and duration of treatment is carried out by the doctor. At the same time, the specialist monitors the disease over time, adjusting the regimen of anti-rhinitis medications if necessary.
Treatment of chronic hypertrophic rhinitis
In cases where the disease is not complicated, conservative treatment can be used. The patient is prescribed medications that simultaneously alleviate rhinitis and help reduce inflammation of the mucous membrane.
The main elements of therapy are:
- Nasal formulations with an anti-inflammatory effect.
- Vasoconstrictor drops based on active ingredients such as phenylephrine, naphazoline, xylometazoline or oxymetazoline. However, their use is justified only with partial and minor changes in the epithelium.
A drug such as hydrocortisone has proven itself to be excellent in the treatment of chronic hypertrophic rhinitis. It is recommended to inject it directly into areas where thickening of the mucosa is observed. The product helps reduce the degree of hypertrophy of the mucous membrane, relieve inflammation and remove congestion. However, doctors use hydrocortisone exclusively in the treatment of the hypertrophic form of the disease in adults, since it is a hormonal type of drug.
If, with hypertrophic rhinitis, a significant part of the mucous membrane hypertrophies, conservative treatment is not advisable. Only surgical intervention can help the patient. The type of operation depends directly on the extent of the lesion, as well as its location. To eliminate rhinitis, the following is carried out:
- osteoconchotomy, if the disease has affected bone tissue;
- conchotomy, or removal of the mucous layer;
- galvanocaustics - cauterization of mucous membranes.
Folk remedies help only in the initial stages. If the chronic form develops, the patient must receive more serious treatment.
Vasomotor chronic rhinitis: how to treat
For rhinitis of this type, treatment is based on the following scheme:
- Rinse the nose with sea water or saline. The liquid allows you to get rid of mucus, as well as reduce its production by affecting goblet cells.
- Use of glucocorticosteroids. Hormonal medications gradually relieve swelling and make breathing easier. They are an excellent replacement for vasoconstrictor drugs, which, although they quickly eliminate unpleasant symptoms, do not help get rid of the causes of the disease. Treatment with glucocorticosteroids gives a lasting effect. They are prescribed mainly to adults.
- Physiotherapy, massage of facial points.
If there is no visible effect from the treatment, then the surgeon will deal with the elimination of rhinitis. Patients are shown ultrasonic disintegration, radio wave surgery, laser destruction, lateropexy with vasotomy.
Actions upon detection of atrophic and subatrophic rhinitis
Patients with a similar diagnosis will have to use three types of therapy in combination during treatment:
- Etiotropic, that is, to eliminate the cause of the disease. Doctors usually recommend the use of antibiotics. The most suitable remedy is selected depending on the specific type of bacteria that caused rhinitis. Bacterial culture, carried out at the stage of diagnosing the disease, helps determine their type.
- Pathogenetic, the purpose of which is to improve the condition of the mucous membranes that are damaged during atrophic rhinitis. Moisturizers based on sea water in the form of aerosols or drops are recommended. Antiseptic drugs that can eliminate purulent inflammation and healing ointments are also prescribed.
- Symptomatic, aimed at alleviating the patient’s condition. Mucolytics are often used to help thin the mucus.
The course of treatment can last quite a long time. When remission occurs, it is recommended not to forget about caring for the mucous membranes and take measures to prevent the emergence of a new exacerbation of rhinitis.
Is allergic rhinitis curable?
The main reason for the appearance of this type of rhinitis is exposure to certain irritating substances, therefore, at the first stage of solving the problem, it is necessary to exclude or at least minimize contact with the allergen, if it is impossible to completely protect the patient from it.
Doctors most often insist on drug treatment, which recommends:
- Immunotherapy. Patients are given small doses of the allergen so that the immune system “gets used to it” and stops reacting to its arrival.
- Taking hormonal drugs. They are designed to reduce or completely eliminate symptoms. The products reduce nasal congestion due to the removal of swelling, and also help reduce sensitivity to the allergen.
- Inhalations. Promote the formation of a protective film on the mucous membranes, which prevents the penetration of the allergen.
Surgery for this type of rhinitis is indicated only if various pathologies are detected, for example, a deviated septum in the nose. The disease cannot be cured by surgery.
Getting rid of medicinal rhinitis
The first step towards a cure is to completely stop using the medications that caused the disease. If this cannot be done immediately, the practice is to gradually reduce the dosage or replace it with less concentrated analogues.
Patients are advised to spend more time in the fresh air, moisturize the mucous membranes and rinse the nose with saline solutions, and do breathing exercises. The effectiveness of physiotherapeutic procedures such as electrophoresis, inhalations, laser and ultrasound therapy has been proven. Breathing returns to normal 1–3 weeks after stopping the drug that caused rhinitis.
Chronic rhinitis
Chronic rhinitis is a long-term, chronic inflammation of the nasal mucosa, which appears as a result of the negative influence of microbes, as well as some environmental factors (dust, air pollution) on the nasal mucosa.
Types of chronic rhinitis
- allergic (seasonal, allergies to plants and products);
- infectious (occurred as a result of infectious diseases);
- non-allergic, non-infectious rhinitis (medicinal rhinitis, hormonal rhinitis, rhinitis of the elderly).
Reasons for appearance
The reasons that contribute to an imbalance in the structure of the inferior turbinate can be physiological, psychological, environmental and pharmacological.
| External factors: | Internal factors: |
|
|
Symptoms of the disease can appear during age-related changes in the body (female, male menopause), bearing a child and breastfeeding. Regular use of medications can also lead to rhinitis:
- antidepressants,
- tranquilizers,
- alpha blockers,
- contraceptives,
- non-steroidal drugs.
In a child, rhinitis may be a consequence of teething. Also, the reason may lie in primary pathologies: tonsillitis, pharyngitis, deviated septum, etc.
Allergic rhinitis
Allergic rhinitis is an inflammation of the mucous membranes of the nose, which is based on an allergic reaction of the body to any allergen.
Possible allergens:
- household or book dust;
- dust mite;
- insect bites;
- plants;
- Food;
- medications;
- molds and yeasts.
You can read more detailed information about allergic rhinitis here.
Diagnostics
Before starting treatment for vasomotor rhinitis, the disease should be diagnosed.
| The criteria that the doctor uses when interviewing: | Characteristic signs of the patient's condition: |
|
|
The doctor evaluates the medical history to determine the cause and history of rhinitis. At this stage, the presence of other diseases of the nasal cavity should be excluded.
Patient examination
Determining the clinical picture involves an objective examination of the patient. Before determining how to treat chronic vasomotor rhinitis, the otolaryngologist must determine whether:
- difficulty contracting the walls during breathing;
- an increase in the size of the walls of the nasal cavity;
- mucous or watery discharge;
- disturbance of a person’s well-being (weakness, fatigue).
If necessary, an allergist and neurologist are involved in making a diagnosis. At this stage, symptoms of VSD are revealed:
- lowering blood pressure,
- feeling of coldness in the extremities,
- joint and muscle pain,
- high sweating,
- anxious state.
After this, laboratory and clinical research methods are carried out.
Rhinoscopy
Rhinoscopy is an examination of the nasal cavity using auxiliary instruments: a funnel for children and a mirror for adults. In modern conditions, the procedure is carried out using a video camera. The result is displayed on the monitor, which makes it possible to analyze the disease over time.
During anterior rhinoscopy, a mirror is inserted into the hole to a depth of one to two centimeters, after which it opens in the anterior sections of the sinus. This allows you to evaluate the condition of the anterior part of the septum, as well as the overall nasal passage.
Average rhinoscopy involves inserting a speculum below the middle concha. The doctor can see the middle meatus.
During posterior rhinoscopy, the fiberscope is inserted through the oral cavity to the pharynx. This way you can assess the condition of the back of the shell. To prevent the gag reflex, treatment with an anesthetic occurs. Based on the results of rhinoscopy, it is determined how to treat vasomotor rhinitis without surgery.
Laboratory research methods
To know how to cure vasomotor rhinitis, you need to conduct laboratory diagnostics:
- A general and biochemical blood test allows you to see the number of eosinophils.
- Allergy tests:
- skin allergy tests - when the pathogen comes into contact with the skin, an allergic reaction occurs;
- assessment of immunoglobulin G to the pathogen involves a laboratory analysis of blood serum using a special tablet.
- An immunogram allows you to assess the quality of the immune system.
- Culture analysis of nasal discharge excludes the presence of an additional infection (rhinitis, sinusitis).
- An x-ray shows a change in the color of the maxillary sinuses and the presence of polyp formation.
The list of additional diagnostic methods includes an electrocardiogram and an electroencephalogram.
Vasomotor rhinitis
Vasomotor rhinitis refers to non-allergic, non-infectious rhinitis. There are medicinal, hormonal, reflex and idiopathic vasomotor rhinitis. It is characterized by impaired nasal breathing, nasal congestion and narrowing of the nasal cavity as a result of swelling and swelling of soft tissues.
Reasons for the development of vasomotor rhinitis:
- low air temperature;
- wet air;
- eating too hot or spicy food;
- frequent consumption of alcoholic beverages;
- experiencing emotional stress;
- inhalation of tobacco smoke;
- smog, air pollution;
- strong odors;
- hormonal changes in the body;
- long-term use of vasoconstrictor drugs;
- use of contraceptives or medications that lower blood pressure;
- thyroid disease, etc.
Clinical signs and symptoms of vasomotor rhinitis
The main symptoms of this form of rhinitis can be considered difficulty in nasal breathing and watery discharge from the nose. Sneezing attacks are less common.
Most often, vasomotor rhinitis is confused with atypical forms of allergic rhinitis. Therefore, a thorough examination is necessary.
1 Endoscopy of the nasal cavity in MedicCity
2 Endoscopy of the nasal cavity in MedicCity
3 Endoscopy of the nasal cavity in MedicCity
Possible complications and consequences of the disease
Neglect of treatment leads to the following negative consequences:
- chronic oxygen starvation of the body;
- persistent headaches;
- surges in blood pressure;
- noise in the head;
- impaired coordination of movements;
- apnea (stopping breathing);
- persistent impairment of ventilation in the nasal sinuses;
- sinusitis or tonsillitis in chronic form;
- allergic rhinitis;
- rhinitis of non-allergic origin and eosinophilic syndrome;
- occupational rhinitis with loss of ability to work, including disability.
Hypertrophic rhinitis
The disease hypertrophic rhinitis is characterized by an increase in the mucous membrane of the nasal turbinates, which entails difficulty breathing due to nasal congestion.
Factors contributing to the disease:
- hypothermia of the body;
- long-term use of vasoconstrictor drugs;
- infections in the nasopharynx;
- contaminated air;
- alcohol;
- smoking;
- presence of allergies.
Hypertrophic rhinitis can occur due to the following diseases:
- diseases of the endocrine system;
- diseases of the heart and blood vessels;
- congenital or acquired curvature of the nasal septum;
- pathology of the neuro-reflex function of the nose;
- untreated catarrhal, vasomotor and chronic rhinitis.
How does the disease manifest?
Hypertrophic rhinitis is characterized by a stuffy nose and difficulty breathing, and vasoconstrictor drops do not eliminate these symptoms. With hypertrophic rhinitis, the following symptoms appear:
- the nose does not breathe;
- mucous and purulent discharge from the nose;
- recurrent headaches;
- dry mouth and nasopharynx;
- disturbances of taste and smell.
Causes and classification of rhinitis
Risk factors for developing the disease include a decrease in general immunity, unfavorable living conditions (strong or prolonged exposure to irritants) and individual intolerance to certain allergens.
According to the course of the disease, they are distinguished:
- acute rhinitis (occurs after the initial exposure to a pathogen or allergen and lasts up to 3 days);
- chronic rhinitis (usually develops as a complication of an acute process and persists for several weeks and even years).
Depending on the cause, there are:
- allergic rhinitis, which develops when the nasal mucosa comes into contact with an allergen - pets, pollen, house dust, mite or yeast allergens. Symptoms can be seasonal (for example, with aggravation in spring, during the flowering period of plants) or year-round;
- non-allergic rhinitis is caused by hypothermia or sudden changes in humidity, viral infections, strong irritants (strong odors, smoke, dust), certain medications (including vasoconstrictor drops), food allergies, disruption of certain organs (thyroid diseases, gastroesophageal reflux), and rhinitis of pregnant women and senile rhinitis are also distinguished;
- Vasomotor rhinitis is not associated with either allergens or pathogens, and develops with hyperactivity and dilation of the blood vessels of the nasal cavity wall. The cause is considered to be an imbalance of the autonomic nervous system, which cannot cope with the function of “inhibiting” the reaction of the nasal mucosa to environmental conditions. The causes may be stress, physical activity, endocrine diseases, as well as hereditary predisposition. In a third of such patients, the disorder is chronic, and in half it manifests itself to a moderate or severe degree.
The causes of rhinitis in children are considered to be imperfect immunity and unfavorable environmental conditions. In addition, this disease in children can be caused by a deviated nasal septum, diathesis, adenoids and polyps, foreign bodies in the nose, sinuses, and long-term use of vasoconstrictor drops.
Chronic catarrhal rhinitis
Chronic catarrhal rhinitis is persistent inflammation in the epithelial tissues of the nose, which does not lead to changes in the structure of the nose.
Typically, chronic catarrhal rhinitis appears as a result of an untreated form of acute rhinitis or its advanced form. In the case of an advanced form, pathogenic organisms multiply in the nasal mucosa, causing catarrhal inflammation.
Symptoms of the disease:
- runny nose that appears in autumn and winter;
- mucous or purulent discharge;
- lack of sense of smell (no nose breathing at all);
- headache.
Diagnostics
During an examination, an ENT doctor may detect boils, cracks and eczema in the nasal cavity. During rhinoscopy, mucus in the nasal cavity in the form of a mesh can be noted.
Treatment of chronic atrophic rhinitis
Alkaline solutions are used in the form of drops, aerosols, irrigation with sodium bicarbonate solution, lubricating the nasal cavity with iodine glycerin (Lugol's solution) with a light massage of the nasal mucosa, which enhances the function of the mucous glands. Previously, we used 1–2% yellow and 5% white mercury ointment with the addition of 1 g of Shostakovsky balsam per 10 g of ointment, furatsilin ointment (at the rate of 1:5000), alkaline and oil inhalations, 2% solution of potassium iodide orally in solution (1 each /2 teaspoon 2 times a day), aloe extract up to 30 injections. It is necessary to humidify the air in the room.
When a hypertrophic process is combined with an atrophic one, treatment is carried out taking into account the predominance of one or another process, affecting areas of hypertrophy with one method, and atrophic areas with other methods.
Treatment of rhinitis
What to do when your nose is stuffy?
Everyone understands what inconvenience a stuffy nose can cause. Treatment must be comprehensive.
The treatment regimen for rhinitis includes the following measures:
- elimination of possible endo- and exogenous factors that cause and maintain rhinitis;
- drug therapy for each form of rhinitis;
- surgical intervention according to indications (for example, for a deviated nasal septum);
- physiotherapy and climate therapy.
Conservative treatment of rhinitis
Conservative therapy includes the following methods:
- Ultrasound and injection inhalation of medicinal substances into the nasal cavity.
- Rinsing the nose and nasopharynx with medicinal substances using a suction aspirator.
- Photodynamic therapy is a unique method of treating rhinitis, based on the use of a photosensitive drug, photoditazine, in the form of a gel, followed by its activation by laser irradiation of the nasal cavity. The drug accumulates in “sick” cells; after laser irradiation, a large amount of oxygen is released, which causes the death of damaged cells and has a powerful antiseptic and anti-inflammatory effect. The volume of the nasal turbinates decreases, nasal breathing improves, and discharge stops. As a result of therapy, you will finally be able to get rid of nasal congestion. The procedure is absolutely painless and takes 1.5-2 hours. Performance is not affected. A course usually requires 2-3 procedures.
- Applications of medications to the nasal mucosa.
1 Sinus Pari inhaler
2 Rinsing the nose and nasopharynx
3 Photodynamic therapy in MedicCity
Surgical treatment of rhinitis
Sometimes it is impossible to do without surgical treatment of rhinitis. In this case, the choice of rational surgical tactics is based on the degree of hypertrophy of the nasal turbinates and impaired nasal breathing. All methods used in our clinic are as gentle as possible.
Surgical treatment of rhinitis includes the following procedures:
- Radio wave coagulation of the inferior turbinates is the most gentle method of treating vasomotor and hypertrophic rhinitis. After anesthesia of the mucous membrane, an electrode with 2 thin needles is inserted into the nasal concha. Under the influence of radio waves, the nasal concha shrinks literally “before our eyes”; nasal breathing improves already at the moment of manipulation. The procedure takes about 15 minutes. and practically painless.
- Laser coagulation is a contact laser effect on the reflexogenic zones of the nasal mucosa or on the entire surface of the inferior turbinate. The procedure is effective, but it should be noted that there is a long recovery period (about 1-2 weeks), as well as greater damage to the mucous membrane than with radio wave treatment.
- Plastic surgery of the inferior turbinates.
If it is necessary to intervene on the nasal turbinates, many clinics still often perform such a destructive operation as conchotomy, which subsequently leads to gross anatomical and functional disorders. Plastic surgery of the inferior turbinate is an alternative to this mutilating operation. Very often, submucosal vasotomy is performed, in which the mucous membrane is detached with the destruction of the choroid plexus, which is the cause of nasal congestion. Sometimes the operation is supplemented by moving the concha to the side, which allows you to significantly expand the nasal passages and restore normal air flow in the nasal cavity. It is also possible to partially remove the posterior ends of the inferior turbinates, which is carried out with a special instrument - a nasal loop, or through bipolar coagulation and radio wave surgery, in which individual areas of the hypertrophied mucous membrane of the turbinates are reduced. The choice of a specific intervention method is individual and is carried out directly by the surgeon.
At the MedicCity multidisciplinary clinic, otorhinolaryngology is one of the priority areas of work! Our otolaryngologists are high-level specialists. General practitioners, immunologists and other specialists from more than 30 specialties will help you cope with your diseases!
Symptoms of the disease
The symptoms of bilateral hypertrophic rhinitis are in many ways similar to the symptoms of other types of runny nose.
The main symptom of the disease is constant nasal congestion. The patient tries to cope with this symptom on his own by actively using vasoconstrictor drugs, but the relief is temporary, and after some period the congestion returns.
Over time, even vasoconstrictor drops cease to cope with this sign of inflammation. Nasal breathing becomes very difficult, and the patient breathes mainly through the mouth. As a result, unpleasant symptoms appear in the pharynx: soreness, dryness, cough, sensation of the presence of a foreign body in the nasopharynx.
Symptoms of the disease also include mucous discharge from the nasal passages (the discharge may be purulent). With a long course, the disease progresses, and other signs of bilateral rhinitis appear:
- constant headaches;
- increased fatigue;
- sleep disturbance;
- decreased sense of smell;
- bleeding of the mucous membrane - this sign of the disease is a consequence of mechanical damage to the mucous membrane when the patient tries hard to clear the nasal passages and relieve congestion;
- snoring at night with cases of temporary cessation of breathing during sleep (apnea);
- nasal voice;
- noise and congestion in the ears.
Unpleasant signs of the disease affect the patient’s psycho-emotional state: he becomes more irritable, perceives new information worse, and gets tired faster. This is due to insufficient oxygen saturation of the brain.
It is impossible to establish a correct diagnosis based solely on symptoms alone. It is necessary to undergo a full examination by an otolaryngologist, who will carry out the necessary diagnostic measures.
Disease prevention
In order not to wonder in the future about how to cure chronic vasomotor rhinitis, you need to take care of measures to prevent it. To do this you need:
- monitor blood pressure levels;
- do not use harmful chemicals and cosmetics;
- eliminate anomalies in the structure of the nasal cavity;
- eliminate airway obstruction;
- review your diet in favor of healthy foods;
- enrich your menu with minerals, vitamins A and E;
- give up bad habits (alcohol, smoking, drugs);
- stabilize the psycho-emotional state;
- engage in moderate physical therapy;
- avoid infection with viral respiratory diseases;
- normalize the functioning of the immune system.
Regular medical examination helps prevent the development of allergic vasomotor rhinitis. Treatment of symptoms must be agreed with a specialist.