Dermatoses
(
dermatosis
, singular; Greek derma, dermat[os] skin + -osis; synonym:
skin diseases
, obsolete -
rashes, rashes
) - a collective term denoting various congenital and acquired pathological conditions of the skin and its appendages; This concept includes skin changes of various origins: dystrophic, inflammatory, infectious, hereditary, etc.
The term “dermatoses” includes both individual nosological forms and group concepts (for example, “dermatitis”, “mycoses”, “dermatozoonoses”, etc.). Temporary symptomatic changes in the skin that do not have an independent wedge, meaning and do not require independent treatment, observed in some infectious diseases (typhoid fever, scarlet fever, measles, jaundice, etc.), are not included in the concept of “dermatoses”.
In modern literature, approx. 2 thousand Dermatoses. At the same time, clinical variants of the same Dermatosis often have independent traditional names (for example, manifestations of infiltrative-suppurative trichophytosis - parasitic sycosis, kerion Celsi, etc.).
According to P.V. Kozhevnikov (1970), the diversity of dermatological pathology is due to the following factors. 1. The anatomical and physiological complexity of the skin, formed by a number of morphological structures (see Skin), although connected with each other, can have an independent patol, condition, in connection with which diseases of the sweat glands can be distinguished - anhidrosis (see), hidrocystoma (see), hyperhidrosis (see), dyshidrosis (see), prickly heat (see), etc.; diseases of the sebaceous glands - acne (see), tumors and nevi of the sebaceous glands; hair diseases - see Hair, table. Nail diseases - see Nails. 2. The ability to observe the dynamics of skin lesions with the naked eye and using a number of research methods, which facilitates the identification and description of wedges and variants. 3. Features of the structure and functional state of the skin in various parts of the human body, in connection with which it is possible to identify diseases characteristic of the folds of the skin, scalp, skin of the palms and soles, etc. 4. The variety and abundance of environmental factors affecting the skin.
general information
Dermatosis is the name of congenital and acquired skin diseases, manifested by rash, redness of the skin, burning and other symptoms.
In most cases, we are talking about inflammatory pathologies caused by allergic reactions or infections. Dermatoses can be associated with dangerous conditions of the nervous and endocrine systems. At the same time, nails and hair are also exposed to pathological effects. Almost every person has experienced at least one form of dermatosis during their lifetime. This may be a temporary irritation of the skin when exposed to an allergen or a severe chronic condition. Inflammatory skin diseases are more common among women. Some types of dermatosis, such as psoriasis, are difficult to treat, but modern means can successfully eliminate the most unpleasant symptoms of such ailments.
Classification
One of the first attempts to classify Dermatoses, which now has only historical significance, belongs to Alibert (JL Alibert, 1832), who divided all skin diseases into 12 groups (eczematous, exanthematous, carcinotic, scabious, etc.). Morfol, D.'s classification was proposed by R. Villan (1785) and then somewhat refined by Bateman (Th. Bateman, 1815). In this classification, all skin diseases were divided into 8 classes: papular, squamous, exanthematous, bullous, pustular, vesicular, tuberculous (tubercular), macular (spotty). Morphol, the classification is still used, in particular by R. Degos (1953).
F. Gebra (1845) developed a classification based on patol signs, but at the end of the 19th - beginning of the 20th century. the pathoanatomical classification could not satisfy dermatologists, because the causes of many D. became clear and there was an urgent need for etiol, classification.
The first attempt to classify D. according to etiol signs was A. Bazin’s identification of mechanical, traumatic and artificial D. Subsequently, numerous attempts were made to classify D.
The etiological-pathogenetic classification, which still retains its significance, was developed by A. M. Krichevsky in 1933-1935; it contains 17 classes.
A. Dermatoses, the etiology of which is known:
1. Traumatic dermatoses. 2. Dermatoses caused by radiant energy (actinodermatoses). 3. Chemical dermatoses. 4. Dermatozoonoses. 5. Dermatoprotozoonoses. 6. Dermatospirochetosis. 7. Dermatomycosis. 8. Dermatobacillosis. 9. Dermatococci. 10. Diseases caused by a filterable virus. 11. Infectious diseases caused by unknown pathogens.
B. Dermatoses, the etiology of which is unknown:
12. Dermatoses associated with suffering of the endocrine and autonomic nervous systems. 13. Dermatoses associated with disorders of interstitial metabolism. 14. Dermatoses associated with diseases of hematopoiesis. 15. Hereditary and congenital dermatoses. 16. Skin tumors. 17. Other skin diseases of unknown etiology.
More complete etiol. the classification is presented in the works of P.V. Kozhevnikov (1970). According to this classification, all skin diseases are divided into 12 groups.
1. Hereditary and congenital developmental anomalies: ichthyosis, keratoderma, epidermolysis, xeroderma, etc. 2. Parasitic and microbial dermatoses caused by animal and plant parasites, microbes, viruses. 3. Exogenous normergic dermatoses caused by mechanical, physical and chemical agents. 4. Angiogenic dermatoses: a) inflammatory - vasculitis, toxicerma, erythema nodosum, etc.; b) angioplastic - angiomas, telangiectasia, etc.; c) hemorrhagic non-inflammatory. 5. Histiohemodermatoses: lymphocytoma, mastocytosis, sarcoidosis, fungoid mycosis, other reticuloendotheliosis. 6. Alimentary dermatoses including hypovitaminosis. 7. Metabolic dermatoses. 8. Endocrine dermatoses. 9. Neurogenic dermatoses: a) psychogenic - dermatomania, dermalgia, pathomimia; b) aesthesiodermatoses - dermalgia, acroparesthesia, etc.; c) vegetative neuroses - livedo, acrocyanosis, seborrhea, psoriasis, urticaria, prurigo, neurodermatitis, dyschromia, etc.; d) allergic dermatoses - eczema, dermatitis herpetiformis; e) atrophy; f) others - pemphigus, lichen planus, etc. 10. Tissue growth disorders: a) non-tumor - part of the keratoses, keloid milium; b) benign tumors; c) malignant tumors. 11. Presumably infectious dermatoses: pityriasis rosea, acrodermatosis atrophy, Lipschitz's erythema migrans, etc. 12. Dermatoses of unknown origin.
In modern foreign manuals [for example, Gertler (W. Gertler, from 1970 to 1973) and others] highlight skin changes due to developmental defects, dyschromia, metabolic diseases, hron, connective tissue diseases, skin diseases caused by exposure to external irritants, circulatory disorders in the skin and hemorrhagic diathesis, neurovascular reactions of the skin, eczema, seborrhea, occupational D., chronic, idiopathic D., erythroderma, dermatohemoblastosis and reticulogranulomatosis of the skin, skin tumors, skin changes associated with the condition of internal organs and lack of nutrition , infectious, parasitic, phytogenic D.
Existing classifications cannot be considered perfect, since the basis for grouping D. (and this is inevitable until their essence is clarified) are very heterogeneous signs: etiology (infectious, parasitic D.), leading symptoms (blistering, itchy D., keratoses , dyschromia, erythroderma), systemic lesions (hemoderma, vasculitis, diffuse connective tissue diseases), etc. They do not fully meet modern requirements also due to the accumulation of new data on the etiology and pathogenesis of a number of D., for example, within the framework of the P. classification. V. Kozhevnikov does not include the group of skin vasculitis, systemic connective tissue diseases and a number of others.
Features of the organ
The skin is an integumentary organ that protects a person from a variety of external influences. Thanks to the skin, internal organs are protected from excessive exposure to heat, cold and ultraviolet radiation. It is also a kind of barrier that prevents the penetration of pathogenic microorganisms into tissues. The skin of different parts of the body may have different structures. Certain areas of the skin have hair. Sweat and sebaceous glands perform auxiliary functions.
Skin layers:
- The surface cover (epidermis), represented by five layers of cells. The outer layer consists of keratinized cells that protect the lower parts of the skin from physical, chemical and microbiological influences. Keratinized epithelial cells periodically exfoliate.
- The middle layer (dermis), which has a connective tissue structure. This area contains numerous blood vessels that supply the skin. The dermis also contains smooth muscles, elastic fibers, hair follicles, sweat and sebaceous glands.
- Subcutaneous fat tissue. This layer of skin contains a large amount of adipose tissue, which protects internal organs from physical impact. This section of the organ also contains blood vessels, nerves and other structures.
Additional functions of the skin include respiration, thermoregulation, immune defense, excretion and metabolism. The prevalence of dermatoses is not least due to the fact that the skin is constantly exposed to negative external factors.
Chronic inflammatory dermatoses of the palmoplantar localization
About the article
12214
0
Regular issues of "RMZh" No. 8 dated 04/09/2013 p. 393
Category: Dermatology
Authors: Belousova T.A. 1, Goryachkina M.V. 1 State Budgetary Educational Institution of Higher Professional Education “First Moscow State Medical University named after. THEM. Sechenov" Ministry of Health of the Russian Federation, Moscow
For quotation:
Belousova T.A., Goryachkina M.V. Chronic inflammatory dermatoses of the palmoplantar localization. RMJ. 2013;8:393.
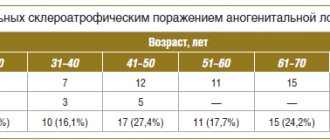
In clinical dermatological practice, dermatoses of the palmoplantar localization (DPPL) are usually called chronic inflammatory diseases, the favorite localization of which is the palms and soles. Damage to these areas of the skin can be caused by many reasons, including: and fungal infection. Among non-infectious dermatoses, damage to the skin of the palms and soles is caused by eczema, psoriasis, and various forms of congenital and acquired keratoderma. Congenital keratoderma is a rare genodermatosis, manifests itself in early childhood and is combined with other malformations of the skin, internal organs, nervous system and musculoskeletal system. The debut of most DLPLs, as a rule, occurs between 30 and 40 years, i.e. at the most active working age. The majority of patients are women, who suffer from this pathology 3 times more often than men. DPPL is characterized by a long chronic course with periods of exacerbations, severe or moderate inflammatory changes, accompanied by itching, burning and soreness of the skin. The particular torpidity of the course of DPPL is largely determined by the constant irritation and traumatization of the skin of the palms and soles by external environmental influences (frequent washing, use of cosmetics and detergents, wearing shoes) [1, 4].
Damage to the most “working”, constantly functionally loaded areas of the skin significantly limits the physical capabilities of patients. Disfiguring cosmetic defects in visible areas of the skin bring patients deep mental suffering. Due to worries about the disease, patients, most of whom are women, develop severe emotional disorders, which causes disharmony in interpersonal and family relationships and underlies low self-esteem. Patients experience great difficulties in performing household and professional duties, choosing a profession, and finding employment. All this leads to a significant decrease in the quality of life. The social significance of DPPL is determined by the fact that in 30% of patients, a progressive increase in the severity of the process and the lack of effect from treatment cause temporary or long-term loss of ability to work, which negatively affects a professional career, leads to a decrease in social status and a deterioration in financial situation [2]. The structure of DLPL in adults is dominated by various forms of eczema (dyshidrotic, tylotic), which account for more than half of all cases. Eczema of the palms and soles is a chronic, relapsing disease with many causes and contributing factors. Allergens are the cause of dermatosis in a quarter of patients. An immediate type I inflammatory reaction according to the classification of P. Gill and R. Coombs can occur to latex in rubber gloves or when hands come into contact with food. However, a delayed type IV reaction is more often formed. Causative allergens often include nickel, chemical ingredients in cosmetics and medications, dyes and materials from which shoes are made. Among the accompanying irritant factors are detergents, alkalis, solvents, disinfectants, prolonged contact with water, friction, cold, and low humidity. The disease may be a reaction to a fungal or bacterial infection. Dyshidrotic eczema manifests itself acutely in the form of development against the background of slight hyperemia of blisters the size of a small pea, sometimes larger and multi-chambered, in the area of the palms, soles and lateral surfaces of the fingers (Fig. 1). After opening the blisters, weeping erosions form, gradually drying into serous crusts, and when a bacterial infection is attached, into purulent ones. After a relapse, the skin of the palms and soles remains dry, peeling and cracked. The cracks can be deep and very painful. The process is persistent, accompanied by severe itching and burning of the skin. During the transition to the chronic stage, infiltration and lichenification increase, hyperemia becomes stagnant, cracks become permanent. Against this background, with exacerbations of the process, blisters appear again, hyperemia, swelling of the skin and itching intensify. A rare type of chronic eczema is horny eczema (eczema tyloticum) (Fig. 2). In this form, there are no symptoms of acute inflammation of the skin in the form of swelling, blistering rashes and itching. On the skin of the palms there are limited areas of hyperkeratosis in the central or marginal zones of the palms and more or less deep cracks. Patients' complaints boil down to roughness and stiffness of the skin of the palms and pain in the area of cracks. A special type of chronic eczema is eczema of the fingertips. The skin of the fingertips is pink-red, dry, flaky, cracked. Vesicles are not typical. Itching is minimal and often completely absent. Soreness and a burning sensation of the skin in the affected area are typical. The process is limited to the distal phalanx of one or more fingers. Atopy may be a predisposing factor; irritants (detergents, contact with water, friction), allergens (glue, medications, foods, plants) may play a role. It is often observed in people of certain professions: dentists, flower growers, office workers, hairdressers. The process tends to be protracted over a long period of time. In a number of patients, the process, starting at the fingertips, slowly spreads to all fingers and the palm and develops into exfoliative keratolysis. This chronic dermatosis is characterized by widespread symmetrical peeling of the skin of the palms. At the beginning, the peeling zones are small in size, up to 2–3 mm in diameter, and have a rounded outline. Gradually they increase in size due to peripheral growth, merge, forming large rounded areas. The central zone becomes hyperemic and painful [3]. The second position (approximately 20%) in this group is occupied by patients with menopausal palmoplantar keratoderma (Haxthousen syndrome). Dermatosis is an acquired form of diffuse keratoderma. The disease mainly affects women in the 5th decade of life. In men, the disease occurs less frequently and at a later age – between 50–60 years. The development of the disease is facilitated by estrogen deficiency and a decrease in the functional activity of the thyroid gland. Patients often have somatic diseases comorbid with dermatosis: obesity, hypertension, cardiovascular diseases, deforming arthritis. The skin of the palms and/or soles, starting from the central zone, is gradually covered with horny layers, the number of which slowly increases both in volume and area. The horny masses crack, pain appears in the area of the lesions, especially when walking, and mild itching. Hyperkeratotic layers can be diffuse or focal with increased horny layers along the edges of the palms and soles. Hyperkeratosis is especially pronounced in areas of pressure and friction. Some patients may have areas of keratosis, incl. with psoriasiform peeling and on other areas of the skin, primarily on the extensor surfaces of the extremities (elbows, knees) [5]. In 10% of patients, skin lesions on the palms and soles are caused by psoriasis (Fig. 3). Most often, this dermatosis occurs between the ages of 30 and 50 years, but can also appear at a later period. A predisposing factor is constant trauma to the skin of the palms during physical labor. The process is represented by infiltrated plaques with clear boundaries of scalloped burgundy-red outlines that protrude above the surface of the surrounding skin. Over time, the plaques, due to peripheral growth, merge into a continuous lesion that occupies the entire surface of the palms or soles. The plaques are covered over the entire surface with thick, firmly seated silvery-white scales, less often with yellowish-gray crusts, after exfoliation of which the bright red surface of the plaque is exposed. Often, with constant trauma, the surface of the rash cracks with the formation of painful, deep bleeding cracks [6]. Despite the fact that the dermatoses included in the group under consideration have their own individual etiopathogenetic mechanisms of development, their clinical symptoms are very similar. This is largely due to the peculiar structure of the skin of the palms and soles. It is known that the skin, depending on the thickness of the epidermis, is divided into two types: thick and thin. The skin of the palms and soles is classified as thick skin (the thickness of the epidermis is 5–8 mm), while in areas of thin skin its thickness does not exceed 1–2 mm. In thick skin, all 5 layers of the epidermis are present, with the spinous layer being 3 times thicker than in thin skin. Thick skin is distinguished by an extremely developed stratum corneum, consisting of 15–20 layers of keratinized cells (in thin skin there are 3–4 rows). At the same time, the thickness of the dermis is small, with well-defined papillae, which increases the area of the basal layer and the ability for a large number of keratinocytes to enter into differentiation. In this regard, DLPL are characterized not only by inflammatory infiltration of the dermis, but also by significant pathological changes in the epidermis. Disorders of keratinization processes are characterized by pronounced pathological changes in the proliferation and differentiation of keratinocytes (acanthosis, hyperkeratosis, parakeratosis). Clinically, this is manifested by intense peeling, focal or diffuse hyperkeratosis, dryness, superficial or deep cracks [7]. External therapy for DLPL is the leading component of the therapeutic complex. The morphological characteristics of the skin of the palms and soles largely determine the therapeutic effect of a particular externally applied drug. It is known that the absorption of external medications depends on the structure (thickness) of the skin. Comparative studies have revealed significant differences in the absorption of the same drug applied to different areas of the skin. This indicator in the forearm area was equal to 1.0; on the back -1.7; on the scalp – 3.5; on the skin of the face –13; on eyelids – 42; and on the palms - only 0.83, on the feet - only 0.14. Thus, even pathologically intact thick skin is capable of absorbing externally applied drugs only in small quantities. With inflammatory changes, impaired desquamation, and thickening of the stratum corneum, the absorption of drugs decreases to an even greater extent. Therefore, the area of the palms and soles is one of the “difficult” localizations for external treatment. According to the frequency of use of various external agents used in the treatment of DPPL, they can be ranked as follows: topical steroids, keratolytics, emollients and moisturizers (emollients), tar preparations and other reducing agents, topical retinoids, calcipotriol (a synthetic analogue of vitamin D3), hydroxyanthrones (ditranol, cignolin). The last three groups are mainly used in the treatment of psoriasis. As clinical practice shows, topical steroids in combination with keratolytics and emollients have an effective therapeutic effect in 75% of patients with DPPL. However, when choosing a specific external steroid, it is necessary to take into account a number of factors that influence their therapeutic effect, primarily the absorption of the steroid, which in less permeable thick skin will be significantly lower than in thin skin. Therefore, to obtain an effect in the first case, a longer duration of treatment and the use of a stronger steroid are necessary than in the second. The penetration of the steroid through the phospholipid layers of the epidermis into the dermis increases with the esterification of the steroid molecule and the lipophilicity of the drug base. An important pharmacodynamic characteristic of a topical steroid is the concentration gradient - the amount of drug transferred into the skin per unit time. Occlusion increases the absorption of the drug many times over. Ointment forms of topical steroids have the greatest penetrating ability. And, finally, the speed of onset of the effect and its duration depend on the rate of binding of the hormone to the cytosolic receptors of keratinocytes and the duration of the association of the steroid with a specific GCS receptor. Thus, the choice of a specific topical steroid for DPPL should be determined by several criteria. The steroid must have significant therapeutic potency (belong to the class of strong steroids) and be applied in the form of an ointment using occlusive dressings. This ensures rapid penetration of the drug through the thick and pathologically altered stratum corneum and the creation of the necessary therapeutic concentration in the focus of chronic inflammation. It is necessary to adhere to the daily frequency of use of a specific steroid, which contributes to the active accumulation and maintenance of the therapeutic concentration of the drug in the pathologically altered skin during the course of therapy. The correct tactics of using a steroid ensures active suppression of inflammation and itching, rapid achievement of a clinical effect with minimal risk of side effects [8]. In the treatment of squamous-hyperkeratotic conditions, keratolytics are actively used, and primarily ointments containing salicylic acid in a concentration of 2–10%. Salicylic acid, by dissolving the intercellular binding substance of epidermocytes, promotes exfoliation of dead horn cells, active rejection of scales and removal of crusts. Possessing hygroscopicity, it attracts water from the subepidermal layers, providing a moisturizing and macerating effect on the epidermis, which also significantly increases its permeability to other medicinal effects. Being a strong b-hydroxy acid, it helps restore the natural acid reaction of the skin, preventing the development of bacterial and mycotic flora, thereby reducing the risk of developing unwanted infectious complications. The use of a combination of topical steroids with 2–10% salicylic acid in the form of an ointment significantly increases the possibility of active penetration of the steroid into the skin [9]. The basic means of external therapy for chronic squamous-hyperkeratotic diseases of the palms and soles, accompanied by severe dryness, peeling, and cracking of the skin, are emollients (from the French molle - soft). In modern dermatological practice, emollients are recognized as highly effective agents, indispensable in the management of patients with dry skin prone to hyperkeratosis and desquamation. These drugs have the ability to moisturize, soften, saturate the skin with fatty components, and restore its aesthetic appearance. They reduce transepidermal water loss and replenish layers of intercorneocytic lipids. The action of emollients is partly due to the effect of filling gaps between exfoliating keratinocytes, but their most important therapeutic effect is to increase the water content in the stratum corneum. Restoring hydration has a beneficial effect not only on the mechanical properties of the stratum corneum, improving the extensibility and flexibility of the skin, but also actively contributes to the normalization of skin desquamation processes. An increase in the concentration of free water molecules in the skin increases the activity of proteolytic enzymes and accelerates the process of destruction of corneodesmosomes, which leads to a more complete and uniform separation of horny scales from the surface of the skin. The use of emollients as part of complex dermatological treatment helps to increase the activity of therapy, reduce the duration of treatment, lengthen periods of remission, improve the prognosis of the disease in general, and therefore improve the patient’s quality of life [10–12]. Thus, the modern arsenal of external therapeutic agents makes it possible to create a program for effective external treatment of a patient with DPPL, taking into account the characteristics of the clinical picture of the disease, the individual and age-related characteristics of the patient’s skin.
Literature 1. Raznatovsky K.I. The role of socio-psychological and emotional stress factors in the development of hemodynamic, microcirculatory and hormonal disorders in dermatoses of the palmoplantar localization: abstract of thesis. dis. doc. honey. Sci. – St. Petersburg, 1997. 22 p. 2. Belousova T.A. Experience of using Elokom S in the treatment of inflammatory dermatoses of the palmoplantar localization // Breast cancer. 2006. No. 5. pp. 357–360. 3. Thomas P. Habiff. Skin diseases. Diagnosis and treatment. – M.: MEDpress-inform, 2006. P. 32–41. 4. Akimov. V.G. Palmoplantar keratoderma of hereditary and acquired nature // Consilium Medicum (add. “Dermatology”). 2011. No. 3. P. 6–10. 5. Albanova V.I. Dermatoses of menopause. //Rus. magazine leather and veins bol. 2002. No. 2. P. 38–42. 6. Wolfe K., Johnson R., Surmond D. Fitzpatrick Dermatology; lane from English; 2nd ed. 2007. pp. 98–117. 7. Myadelets O.D., Adaskevich V.P. Functional morphology and general pathology of the skin. – Vitebsk: Publishing House of the Vitebsk Medical Institute, 1997. 269 p. 8. Fitzpatrick D.E., Eling D.L. Secrets of dermatology. – M.: Binom, 1999. P. 55–63. 9. Kruglova L.S. Modern possibilities of external therapy for psoriasis. 10. Loden M. The clinical benefit of moisturizers // JEADV. 2005. Vol. 19. P. 672–688. 11. Marks R. Actions and effects of emollients // Sophisticated Emollients. – Stuttgart, New York: Georg Thieme Verlag, 2002. P. 12–23. 12. Trapp M. Is there room for improvement in the emollients for adjuvant therapy? // JEADV. 2007. Vol. 21(2). P. 14–18.
Content is licensed under a Creative Commons Attribution 4.0 International License.
Share the article on social networks
Recommend the article to your colleagues
Common types
Dermatoses may differ in their causes, symptoms and possible complications. Dermatologists encounter certain diseases more often in their practice.
Known diseases:
- A group of inflammatory skin diseases (dermatitis). Many people get allergic dermatitis because the immune system reacts to certain substances (allergens). Dermatitis can also be caused by infections, exposure to chemical irritants, endocrine diseases and other pathological conditions.
- Psoriasis is a chronic inflammatory pathology of the skin of a non-infectious nature. For many years, doctors did not know the cause of psoriasis, but new research has linked the etiology of this disease with dysfunction of the immune system. The disease manifests itself as numerous skin rashes in the form of papules and plaques. The first symptoms usually occur in adult patients.
- Eczema is an inflammation of the skin, characterized by the appearance of various rashes. Eczema often occurs against the background of pathologies of internal organs. External chemical influences can also cause an inflammatory response.
- Scabies is a parasitic infection that occurs when the scabies mite penetrates the surface layers of the skin. The disease is manifested by itching, the appearance of rashes and ulcers.
Many dermatoses have similar symptoms, so only a doctor can clarify the diagnosis with the help of special examinations.
What happens to the human body before skin symptoms appear?
Allergic skin diseases are based on changes in the reactions of the immune and nervous systems. After initial contact with an allergen, the immune system remembers information about it, i.e. the body enters a state of heightened readiness to quickly react to the re-entry of the same antigen (sensitization). During this time, the person is not bothered by any symptoms. And when this allergen is reintroduced, a pathological immune process begins with damage to the skin and sometimes other organs.
Causes
Dermatoses can occur due to the influence of external and internal factors. External influences are most often represented by chemical irritants that affect the condition of the skin. Diseases of internal organs can also affect the condition of the skin. An important role in the etiology is played by hereditary factors that cause increased sensitivity of tissues to certain influences. The reasons for the development of some forms of dermatosis still remain poorly understood.
Possible reasons:
- Features of the immune system. Normally, immunity protects the body from the effects of pathogens. Immune system cells are present in the skin because this is the anatomical region that first encounters pathogens. In some cases, the immune system is hypersensitive to certain substances, such as pollen, dust or animal hair. Skin contact with such substances leads to an allergic reaction. The inflamed epidermis begins to itch.
- Autoimmune pathologies. When the immune system malfunctions, cells begin to attack healthy tissue. The patient experiences an inflammatory reaction, accompanied by redness and swelling of the skin. A typical example of autoimmune dermatosis is psoriasis.
- Hormonal imbalance. Normally, endocrine factors control the development of the skin. A deficiency or excess of certain hormones can lead to dermatosis. Thus, in adolescents during puberty, hormonal levels change, which often results in skin rashes.
- Metabolic disease. The structure of the skin depends on the constant supply of important components to the cells. A lack of certain vitamins or minerals can cause brittle nails or peeling skin.
- Exposure to pathogenic microorganisms. Bacteria, fungi, viruses and protozoa can attack the skin and cause infectious dermatosis.
- Uncontrolled use of medications. Thus, the use of antibiotics increases the skin's sensitivity to sunlight. Some painkillers also have a negative effect on the skin.
Clarifying the cause of dermatosis is important for selecting effective therapy.
Risk factors
In addition to the direct causes of pathology, doctors take into account the influence of additional factors related to heredity, lifestyle and the patient’s individual history.
Possible risk factors:
- Excessive ultraviolet exposure.
- Using personal hygiene products that are harmful to the skin.
- Insufficient skin hygiene.
- Genetic disorders (eg, epidermolysis bullosa.)
- Allergic history. If a person suffers from allergies, the risk of dermatosis increases.
- Diseases associated with a high risk of skin pathology: bronchial asthma, congestive heart failure, HIV infection.
- Professional activity that requires constant contact with chemicals and other irritants.
- Age. Inflammatory dermatoses occur more often in children and young patients.
- Hormonal changes in adolescents, pregnant women and other categories of patients.
Considering risk factors helps dermatologists prescribe preventative measures.
Symptoms
The manifestations of dermatoses are varied and contradictory. The most characteristic symptom of skin pathology is an itchy rash. The patient may develop small red spots, blisters, papules, warts, small tumors and other abnormal skin structures. The nature of the rash helps doctors determine the cause of the disease.
Other possible symptoms:
- Redness and swelling of the skin.
- The appearance of ulcers.
- Blister formations.
- Severe peeling of the skin.
- Brittle nails and hair loss.
- Excessive dry skin.
- The appearance of a crust.
- Constant fatigue.
- Decreased performance.
- Sleep disturbance.
Cosmetic defects that occur with dermatitis negatively affect a person’s mental state. Some diseases that manifest as profuse acne are difficult to treat, so patients are forced to adapt to their appearance.
Diagnostics
If symptoms of a skin disease appear, you should make an appointment with a dermatologist. During the consultation, the doctor will ask the patient about complaints and collect medical history information to identify risk factors for dermatosis. Then a general examination of the skin is performed to identify characteristic clinical signs of pathology. To clarify the diagnosis, the dermatologist needs the results of instrumental and laboratory tests.
Additional diagnostics:
- Laboratory blood tests. In the treatment room, a nurse collects venous blood and sends the material to the laboratory. Specialists evaluate the ratio and quantity of formed components, and also study the biochemical parameters of the blood. A blood test can detect signs of infection, autoimmune inflammation or other pathology.
- Dermatoscopy. Using a special device, the doctor takes an enlarged photo of the affected area of skin and studies the features of the rash. Dermatoscopy is important for differential diagnosis and exclusion of dangerous diseases such as melanoma.
- Laboratory examination of exudate. The specialist collects secretions from ulcers or other skin formations. The resulting material is studied in the laboratory to detect pathogenic microorganisms or signs of inflammation.
- Histological examination of the skin. A biopsy is performed if it is necessary to exclude oncology.
- Carrying out allergy tests. The doctor places microscopic particles of the irritant on the skin and monitors the condition of the tissue. This study is necessary to find the source of the allergy.
If necessary, the dermatologist may prescribe additional tests, including a general urine test. A timely appointment with a doctor helps to quickly clarify the cause of the rash and select effective treatment.
results
After therapy, all patients showed positive results, however, the dynamics of itching and signs of inflammation when using combination and monotherapy had statistical differences.
Thus, on lesions where combination therapy was used ( Neotanin
+ Akriderm), the intensity of itching by the 3rd day of the study decreased by 60% (from 10 points to 4), with monotherapy with Akriderm - only by 22% (from 9 points to 7;
p
= 0.02) (Fig. 1).
Rice.
1. Intensity of itching (on a 10-point scale). According to the daily diaries of patients, in areas of the body where Neotanin
, the itching stopped much faster: after 8-15 minutes - compared to monotherapy with Akriderm, in which the cessation of itching was observed on average only after 60 minutes (
p
<0.01) (Fig. 2).
Rice. 2. Time to relieve itching after applying the drug, min. The duration of antipruritic action after application of Neotanin
+ Akriderm was on average 2-3 hours, Akriderm - only 30 minutes (
p
<0.01) (Fig. 3).
Rice.
3. Duration of antipruritic action after application, min. Thus, the duration of antipruritic action (time for resolution of clinical manifestations) with combination therapy of Neotanin
with a topical glucocorticosteroid is 4 times higher compared to monotherapy with a topical glucocorticoid (Fig. 4).
Rice. 4. Terms of resolution of clinical manifestations when using combination therapy compared to monotherapy with a topical glucocorticosteroid: a) in a 35-year-old woman with moderate atopic dermatitis (exacerbation); b) a 35-year-old woman with acute eczema of the hands.
Rice. 4. Terms of resolution of clinical manifestations when using combination therapy compared to monotherapy with a topical glucocorticosteroid: c) in a 25-year-old woman with mild atopic dermatitis (exacerbation).
Frequency of itching on the half of the body to which Neotanin
+ Akriderm, by the end of the 1st week decreased by 75% - from the indicator “very frequent itching” to the indicator “rare itching”;
in the area of application of Akriderm by 25% - from the indicator “very frequent itching” to the indicator “frequent itching” ( p
<0.01).
The severity of itching was assessed on a scale from 0 to 4 points, where 0 points means no itching, 4 means severe itching. At the 1st visit, the average score was 4 on each side. By the end of the 1st week, on the areas of the body where Neotanin
+ Akriderm, severity of itching decreased to 2 points (mild itching);
Akriderm - up to 3 points (moderate itching) ( p
<0.02).
Each of the signs of inflammation (erythema, edema, oozing, excoriation, lichenification and dryness) was assessed on a scale from 0 to 3 points, where 0 points means no symptom, 3 means a pronounced symptom. The intensity of inflammation was determined by the sum of scores of all signs. The intensity of skin inflammation on the 7th day of treatment decreased by 50% on skin areas after application of Neotanin
+ Akriderm, by 22% - in areas with monotherapy with glucocorticosteroids (
p
<0.01).
In addition, during monotherapy with Akriderm, in 3 patients an exacerbation of the skin process was recorded on the 5th-7th day of therapy, in 1 patient a bacterial infection was noted on the skin area.
In general, during treatment, an increase in the quality of life was found in almost all patients included in the study.
On areas of the body where Neotanin
+ Akri-derm, the effectiveness of therapy on the 4th visit (10th day) was assessed by the doctor in 37 (92.5%) patients as a marked improvement, in 3 (7.5%) - as an improvement. After using Akriderm, the indicators were as follows: in 7 (17.5%) patients there was a marked improvement, in 27 (67.5%) there was an improvement, in 5 (12.5%) there was no change, in 1 (2.5%) %) - deterioration.
DIQL was measured at the beginning and at the end of treatment: a decrease was noted from 21 points (the disease has an extremely strong impact on the patient’s life) to 9 (the disease has a moderate impact on the patient’s life).
Treatment methods
Polymorphic skin formations, characteristic of certain types of dermatosis, arise for various reasons, so treatment is selected after diagnosis. Most often, a dermatologist prescribes drug therapy. The dermatologist takes into account possible contraindications before selecting therapy.
Frequently prescribed drugs:
- Corticosteroids are medications that ease the inflammatory response.
- Antibiotics are drugs that destroy pathogenic microorganisms.
- Antiseptics for external use.
- Antihistamines are medications that prevent the development of an allergic reaction and skin lesions.
- Various immunosuppressants that suppress autoimmune reactions.
The listed medications can be prescribed in the form of ointments, gels, tablets or solutions for intravenous administration. Local use of corticosteroids can reduce the risk of side effects. Additional treatment options include surgery and physical therapy. In most cases, the dermatologist prescribes a hypoallergenic diet and vitamin supplements to the patient. Compliance with the doctor’s recommendations helps prevent the development of relapse.