Exudative erythema multiforme (EEM) - symptoms and treatment
Infectious-allergic MEE, including herpes-associated[13], is characterized by an acute onset of the disease. It can be manifested by fever, general weakness, body aches, headache, sore throat and other symptoms.
Often, a few days before an exacerbation of MEE, a herpes infection is activated in patients - herpes appears on the lips or a relapse of genital herpes occurs[8].
Rashes characteristic of MEE usually begin to appear 1-2 days after the onset of prodromal phenomena. In this case, general symptoms usually subside.
The localization of the rash is very diverse. It can appear on both the skin and mucous membranes.
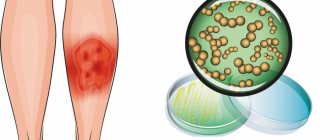
Skin manifestations
The skin is usually marked by clearly defined rounded red-pink spots and flat, edematous papules, which increase in size from 2-3 mm to 3 cm in diameter. In the infectious-allergic form, the spots are usually somewhat smaller and do not tend to merge. They can cause itching and burning.
The predominant localization of rashes is on the extensor side of the arms and legs, the back of the feet and hands, on the face and in the genital area. Basically, they are located symmetrically on the body, often in groups in the form of arcs or garlands.
As the papule grows, its center begins to sink and change color to a more bluish color; a red-pink rim remains along the periphery - thus, the elements of the rash acquire the characteristic appearance of a “target” (sometimes they are compared to a “bull’s eye” or “cockade”) [4] .
Afterwards, bubbles form in their center - vesicles and bullous elements. They contain serous or bloody exudate. When they burst, the blisters form yellowish or brown-brown crusts and eroded surfaces.
As a result, elements of varying degrees of development are simultaneously present on the patient’s body - spots, papules and blisters, turning into crusts and erosions. That is why erythema is called multiforme.
At intervals of several days, new groups of rashes may form. This may delay the process. But usually final regression occurs within about two weeks.
The frequency of exacerbations can vary from 1-2 to 5-12 times a year. In rare severe cases, one exacerbation can turn into another, with virtually no clear interval. During this time, previous rashes do not completely resolve.
Rashes on mucous membranes
Single elements may appear on the oral mucosa, which do not cause much concern. In more severe cases, the lesions are so extensive and painful. They make it difficult to speak and eat even homogeneous and liquid food[12][13].
The resulting blisters burst quite quickly, so the patient does not have time to notice them - usually erosions are already detected, on which filmy fibrinous deposits of a light or brown hue can sometimes be seen.
In the area of the red border of the lips, very painful, cracking, bloody crusts may appear, which do not allow the patient to fully open his mouth.
Less commonly, rashes are found on the mucous membranes of the eyes and genitals. In complicated cases, secondary infection may occur, scarring and synechiae (adhesions) may form.
Symptoms
Before the appearance of rashes and during the course of the disease, there is a deterioration in the general condition, malaise, increased body temperature, fatigue, pain in the joints, burning and soreness in the mouth, and difficulty eating.
Edema spots, papules, vesicles, and blisters appear. Polymorphism of elements is primary. Very rarely there is a monomorphic blistering rash. Characteristic plaques spread along the periphery like a roller (cockade) and sink in the center (cockade-shaped rashes). In the center of the plaque is violet-bluish in color, and along the periphery - pink-red.
Bubbles and vesicles with serous, less often hemorrhagic contents are surrounded by an inflammatory rim. Blisters and vesicles open, serous whitish or grayish-yellow, as well as hemorrhagic crusts form on the surface of the erosions. Scraps of blisters and vesicles appear along the edges of the erosions; Nikolsky's symptom is negative. Rashes in the mouth are painful.
The location of the rashes is characteristic on the back of the hands, feet, extensor surfaces of the limbs, palms and soles. Often the elements of the rash are arranged in the form of garlands, arcs, and rings.
Erythema nodosum
Hepatitis
Arthritis
Colitis
Allergy
17476 08 February
IMPORTANT!
The information in this section cannot be used for self-diagnosis and self-treatment.
In case of pain or other exacerbation of the disease, diagnostic tests should be prescribed only by the attending physician. To make a diagnosis and properly prescribe treatment, you should contact your doctor. Erythema nodosum: causes, symptoms, diagnosis and treatment methods.
Definition
Human skin consists of epidermis and dermis. The epidermis serves to protect the underlying tissues from mechanical, chemical, thermal damage, as well as from the penetration of infectious agents. The dermis is a layer of skin that includes a network of blood vessels, subcutaneous fatty tissue (SAT), connective tissue fibers, hair follicles, sweat and sebaceous glands.
Erythema nodosum is an inflammatory lesion of small vessels of the skin and subcutaneous fatty tissue, which is a type of panniculitis (inflammation of fatty tissue that develops against the background of other diseases or is idiopathic in nature).
Causes of erythema nodosum
Unfortunately, it is not always possible to establish for certain what led to the appearance of erythema nodosum. This poses difficulties in determining treatment tactics for such a condition. Most often, erythema nodosum is found in adults of reproductive age. In children and adolescents, it can develop against the background of a previous streptococcal infection.
The cause of the inflammatory process, which results in erythema nodosum, can be infectious agents, autoimmune diseases, allergic reactions, taking medications (sulfonamides, penicillin antibiotics, oral contraceptives, bromides, etc.). Pregnancy can also provoke the appearance of erythema nodosum.
Under the influence of these factors, lymphocytes are activated, the immune system begins to produce specific antibodies and inflammation develops. However, such a response of the body is not detected in every person, which suggests a special predisposition to such an immune response, and the predisposition can be either hereditary or acquired.
Erythema nodosum usually develops in the presence of two conditions: specific abnormal activity of the immune system and a provoking factor (trigger).
Among infectious diseases, such triggers are often streptococcal infection, tuberculosis, chlamydia, hepatitis B and C, etc.
The incidence of erythema nodosum in autoimmune diseases is high. This is a group of diseases that are based on a violation of the immune system’s recognition of “self” and “foreign” cells. As a result, immune cells begin to show aggression against cells of their own body, just as they would be activated when meeting infectious agents or cancer cells.
Erythema nodosum is common in sarcoidosis. One form of sarcoidosis (Löfgren's syndrome) is a combination of bilateral damage to the lymph nodes located in the roots of the lungs, joints, fever and erythema nodosum.
Other autoimmune diseases associated with the development of erythema nodosum include:
- systemic lupus erythematosus;
- rheumatoid arthritis;
- Behçet's disease (a disease based on vascular inflammation);
- Sjögren's disease (a disease that primarily affects the salivary and lacrimal glands);
- nonspecific ulcerative colitis (severe inflammatory damage to the colon), etc.
Sometimes erythema nodosum develops against the background of various malignant neoplasms, which include leukemia, lymphoma, pancreatic cancer, etc.
Classification of erythema nodosum
Erythema nodosum can be either an independent disease of unknown etiology (
primary or idiopathic erythema nodosum
) or develop as part of other diseases (
secondary erythema nodosum
). This classification is extremely important for determining the patient’s treatment tactics, because the treatment of secondary erythema nodosum is based on the effect on the underlying disease.
Erythema nodosum may have an acute
,
migratory
or
chronic course
.
Symptoms of erythema nodosum
The clinical features of erythema nodosum depend on the etiological factors and the nature of the process.
Primary (idiopathic) erythema nodosum manifests itself acutely - bright red painful confluent nodes form on the legs against the background of swelling of the legs and feet.
In acute cases, the nodes develop rapidly. Characterized by a concomitant increase in temperature to 38-39°C, weakness, headache, arthralgia. The disease is preceded by viral infections or tonsillitis. The nodes usually disappear without a trace after 3-4 weeks without ulceration, relapses are rare.
Migratory erythema nodosum is characterized by an acute course with an asymmetric inflammatory component. The main node is dense, bluish-red in color, delimited from the surrounding tissues. As a result of peripheral growth due to the migration of the inflammatory infiltrate, a ring-shaped plaque is formed with a sunken pale center and a wide, more saturated peripheral zone. Single small nodules may appear, including on the opposite shin. The duration of the disease is up to several months. During the formation of nodes, concomitant general disorders in the form of chills, weakness, arthralgia, and low-grade fever may be observed.
Chronic erythema nodosum usually occurs in middle-aged and elderly women, often against the background of vascular, allergic, inflammatory, infectious or tumor diseases. Exacerbation occurs more often in spring and autumn. Nodes with moderate pain and the size of a walnut are localized on the legs (on the anterolateral surface), swelling of the legs and feet is observed. Relapses can last for months.
Diagnosis of erythema nodosum
The diagnosis of erythema nodosum is made based on the clinical picture. This suggests that the data obtained during the conversation with the patient and examination is sufficient. However, to select treatment, it is necessary to establish causative and concomitant diseases. For this purpose, the patient may be prescribed the following studies:
- A clinical blood test with a leukocyte count, which will allow you to assess the intensity of inflammatory processes in the body, suspect the cause, and identify changes characteristic of leukemia and lymphoma.