It is necessary to distinguish physiological anovulation from pathological.
- Physiological is considered a violation of the maturation and release of the egg from the follicle during puberty, during pregnancy, lactation and menopause. In addition, ovulation does not occur 1-2 cycles a year, since the ovaries need rest.
- Pathological anovulation occurs with various diseases and hormonal disorders. The dominant follicle does not develop or burst, as it should normally, but regresses and turns into a cyst. The egg does not enter the abdominal cavity, therefore, fertilization and pregnancy are impossible.
Typical pathogenesis of the anovulatory cycle
In the ovaries, during the anovulatory cycle, periods of development and degradation of the follicle vary in duration and characteristics. The anovulatory cycle is characterized by an oversaturation of the action of estrogen, which must fall under the influence of the gestagenic hormone progesterone, which does not happen during the anovulatory cycle. In very rare situations, the anovulatory cycle is comparable to hypoestrogenism.
The development of the level of estrogenic influence affects the endometrium of various types.
Atresia of the follicle becomes the cause of hormonal imbalance, and this already becomes the reason for the development of the anovulatory cycle and the cause of such menstrual bleeding. During each anovulatory cycle, the endometrium begins to exhibit functional failures, and the anovulatory cycle will therefore be accompanied by hemorrhages, extravasations, and necrosis. The uppermost layers of the endometrium are quite unstable and often disintegrate, which causes bleeding, but in the absence of independent endometrial rejection, the development of bleeding is accompanied by diapedesis of red blood cells. At times, hyperestrogenism does not decrease and the excretion of estrogen in the urine remains quite stable throughout the current anovulatory cycle.
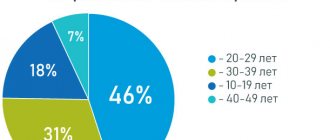
When menstrual function matures in puberty, the cause of the anovulatory cycle may be the lack of the required ratio of luteinizing and luteotropic hormones, the synthesizing reactions of which become most active by the age of 16.
The gynecology of the female body develops in inverse proportion during menopause:
- cyclic secretion is disrupted;
- there is an increase in gonadotropic influence.
Such unsystematic alternations of full menstrual and anovulatory cycles with fading reproductive function are accompanied by changes in the nature of menstruation and the duration of the cycle itself.
What is the manifestation of the anovulatory cycle?
In medicine, the anovulatory cycle manifests itself in several ways. Through ordinary observation, it is almost impossible to determine the anovulatory cycle, the signs of which are invisible to the naked eye. Menstrual-like bleeding very often may not differ at all in the regularity of occurrence and volume of discharge from anovulatory bleeding.
During hyperestherogenia, bleeding is accompanied by heavy and prolonged bleeding similar to menorrhagia. In this case, violations of the standard size of the uterus are observed, it increases significantly, changes its density, the cervix softens and becomes covered with the internal os. As a result, excessive bleeding causes anemia.
Hypoestrogenia, on the contrary, is characterized by scanty bleeding. A gynecological examination reveals a uterus of reduced size, with a long conical neck, the internal os remains closed, and the vaginal passages are narrower.
During the anovulatory cycle during menopause, a woman does not have the opportunity to become pregnant. The cause is hormonal imbalance, in medicine this condition is called hormonal infertility.
middle line
This line is drawn over 6 temperature values in the first phase of the cycle preceding ovulation.
This does not take into account the first 5 days of the cycle, as well as days on which the temperature could be affected by various negative factors (see rules for measuring temperature). This line does not allow any conclusions to be drawn from the graph and is for illustrative purposes only.
Causes of anovulatory cycle
In average healthy women, anovulatory cycles are practically not observed during reproductive age. In rare cases, anovulatory cycles alternate with menstrual cycles, but are not systematic. In such women, the anovulatory cycle can be caused once by a sudden change in climate or a change in geographical zone.
The most common reasons for the development of an anovulatory cycle of physiological origin include age-related changes in the female body, such as:
- puberty;
- pregnancy, breastfeeding;
- menopause
In nature, the anovulatory cycle and pregnancy, as well as postpartum recovery of the female body, are closely related. As soon as the woman in labor restores her menstrual cycle, in 50% of women who breastfeed, this cycle remains single-phase anovulatory.
The reasons for the development of a pathological anovulatory cycle include:
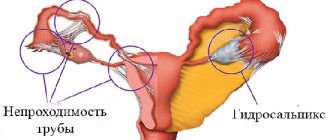
- ovarian dysfunction;
- hypothalamic-pituitary regulation of the menstrual cycle.
Ovarian dysfunction has a direct impact on the development of the anovulatory cycle. Firstly, the anovulatory cycle is greatly influenced by inflammatory processes in the ovaries or appendages. Secondly, abnormal internal secretion of the ovaries can also lead to menstrual irregularities. Thirdly, impaired functioning of the thyroid gland becomes the first cause of single-phase anovulatory cycles.
In case of erroneous processes of hypothalamic-pituitary regulation, the following is observed:
- insufficient production of FSH, which prevents full maturation of the follicle, thereby depriving the follicle of the ability to ovulate;
- LH deficiency;
- hormonal instability;
- excessive prolactin production.
Very often, the development of anovulatory cycles is influenced by congenital defects of the reproductive system, delayed sexual development, and genetic pathologies.
How does ovulation occur?
This process is part of the so-called reproductive or menstrual cycle, which is present in any healthy woman of reproductive age (18-35 years) and affects the functioning of her entire reproductive system (namely the ovaries and uterus). It is divided into the following stages:
- Follicular (1-13 days). The pituitary gland in the brain produces gonadotropin-releasing hormone (GnRH), which, together with follicle-stimulating [FSH] and luteinizing [LH] hormones, accelerates the development of 10-20 eggs in the follicles (egg vesicles) of one of the ovaries. In parallel with this, the old endometrium (mucous membrane) is rejected in the uterus, which, together with blood, exits the genital tract in the form of menstrual bleeding. Towards the end of this phase, a new endometrium forms and quickly thickens.
- Ovulatory phase (14-17 days). Approximately on the 14th day of the cycle, the pituitary gland releases luteinizing hormone, under the influence of which the most mature follicle opens and releases the egg into the fallopian tube, which connects the ovary to the uterine cavity. The remaining, less developed follicles gradually decrease in size, returning to their original state. The endometrium in this phase is already of sufficient thickness.
- Luteal phase (13-14 days). The follicle, after releasing the egg, transforms into the corpus luteum, which produces the hormones estradiol, progesterones and androgens. Under their influence, the thickened endometrium of the uterus is modified, the number of blood vessels and secretory glands in it increases, preparing it for embryo implantation. When pregnancy occurs, the corpus luteum continues to produce progesterone until the developing placenta begins to synthesize it itself. If pregnancy does not occur, then the synthesis of estradiol and progesterone is reduced, the endometrium becomes thinner and begins to die.
It is obvious that ovulation is closely interrelated with other processes of the menstrual cycle. Therefore, its disorders are most likely associated with the work of all organs and systems involved in the reproductive function of a woman.
Take the first step
make an appointment with a doctor!
Diagnosis of anovulatory cycle
Approach 1.
The simplest and most common method for diagnosing an anovulatory cycle is determining basal temperature. A full menstrual cycle is accompanied by an increase in basal temperature during the activation of the progesterone phase. During the anovulatory cycle, a single-phase temperature remains.
Approach 2.
Active estrogenic influence during the anovulatory cycle is detected on the basis of functional tests (the “pupil” symptom during a single-phase cycle, positive fern phenomenon), colpocytological data.
Approach 3.
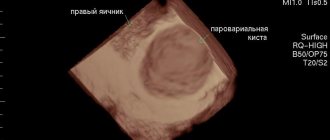
The main signs of the anovulation cycle include the absence of a dominant follicle, which can easily be determined using dynamic ultrasound radiation when examining the ovaries.
Approach 4.
One of the decisive approaches to diagnosing the anovulatory cycle is gynecological curettage of the uterine cavity before the so-called menstruation. Afterwards, a histological examination of the scraping is required. Confirmation of the absence of secretory changes in the endometrium in the analysis indicates a disruption of the menstrual cycle and the active development of the anovulatory cycle.
Approach 5.
Determining the etiological reasons for the development of the anovulatory cycle is carried out by studying the state of the thyroid gland, the hypothalamic-pituitary hormonal system, and the adrenal cortex. All kinds of inflammatory processes in a woman’s genitals must be diagnosed.
But since the menstrual and anovulatory processes can alternate irregularly, only six-month dynamic monitoring of the state of follicle development can make the diagnosis accurate.
Treatment of anovulatory cycle
Firstly, it is important to understand that treatment of the anovulatory cycle is possible only if the patient wishes. Secondly, an endocrinologist is a specialist in this disease. Thirdly, one should not delay if there is a suspicion of illness. If you detect at least some symptoms, it is important to immediately consult a doctor. A prolonged painful condition of the female genital organs threatens the development of infertility and obvious changes in the endometrium. Deviations noticed by a doctor in time can be stimulated by artificially induced ovulation and suppression of excessive proliferation.
Hormonal treatment of anovulatory cycles is carried out intermittently, referring to the degree of estrogen saturation.
To stimulate the resumption of stage-by-stage full menstruation, drugs with gonadotropic effects are prescribed, but only after the preliminary curettage procedure.
With physiological anovulation during puberty or at the end of reproductive age, lactation, treatment is not required.
Hyperstimulation and its consequences
Abuse of stimulant drugs is fraught with the development of hyperstimulation syndrome. This pathology is characterized by the formation of functional cysts on the genitals. Overstimulation can be mild or severe. Symptoms of mild pathology:
- pain in the ovarian region;
- bloating;
- nausea and vomiting;
- slight weight gain.
The severe form of hyperstimulation syndrome is characterized by the following symptoms:
- sudden weight gain (up to 10 kg per week);
- constant nausea, vomiting;
- swollen and hard belly;
- severe pain in the lower abdomen;
- formation of blood clots in the veins of the legs;
- respiratory dysfunction.
If mild symptoms go away on their own, then severe hyperstimulation requires close medical supervision and drug treatment. Ignoring severe symptoms of hyperstimulation can lead to irreversible consequences - miscarriage, cyst formation, bleeding, kidney failure and even death.
Gynecologists at the Raduga clinic will help you find the cause of the lack of ovulation and restore the normal functioning of the female body.
What can be the prognosis after treatment of anovulatory cycles?
It is very important to correctly develop a course of treatment for anovulatory cycles. After completing it fully, about 40% of women suffering from the disease can successfully conceive, bear and give birth to a child.
A woman should be very careful and careful about her health. Self-care should be accompanied by good nutrition, rational distribution of working time and rest periods. Every woman should make regular visits to a gynecologist to check the health of her genitals, take care of protection from fungi, and avoid infection with toxins.