Somatoform disorders are a group of diseases of a psychogenic nature, the peculiarity of which is the presence of somatic complaints in the absence of pathological changes in internal organs that could explain the cause of the complaints. People often visit various doctors, undergo examinations for the presence of physical diseases and undergo treatment. Somatoform disorders (F45) according to ICD-10 belong to the group of neurotic, stress-related and somatoform disorders (F40-48).
With somatoform disorder, a person cannot recognize the psychosomatic onset of the disease, even if there are symptoms of anxiety and depression. Disorders affect a person’s ability to work and quality of life. A specific manifestation of the disease should be considered the patient’s conviction that he has somatic diseases, which decreases after research and health assessment by a specialist.
There are five types of somatoform disorders: hypochondriacal, somatization, chronic somatoform pain disorder, undifferentiated somatoform disorder and somatoform dysfunction of the autonomic nervous system.
The main reasons for the development of the disorder are stress, indifference of loved ones, the presence of other mental illnesses and personality traits.
In patients, the results of medical examinations will be within normal limits or with minor deviations, but will not explain the symptoms that occur. Symptoms of the disorder cause a person to experience excessive worry and anxiety, which interferes with everyday life, and the person constantly seeks medical help.
In the presence of a somatoform disorder, the clinical picture may include any symptoms, most often pain of various types, vegetative and somatic manifestations. The presence of symptoms is not associated with a physical illness. Normal sensations are perceived by the patient as abnormal. A person focuses all his attention on internal sensations, as a result of which somatoform disorders are often accompanied by anxiety and symptoms of depression.
There are five types of somatoform disorders:
Hypochondriacal disorder. The patient has numerous concerns about the presence of a serious incurable disease, which, in his opinion, may cause death. Fears are accompanied by affective disorders - anxiety, hopelessness, despondency. There is instability in ideas about the presence of a specific disease and its severity; the “diagnosis” depends on somatic manifestations and can change; the level of fear for one’s health also changes. Hypochondriacal depression often develops against the background of affective disorders.
Somatization disorder. With this form of the disorder, the patient's internal mental conflicts are expressed in the form of somatic symptoms. The person is convinced that the symptoms are caused by a physical illness. Complaints are varied, constant, atypical for a somatic disease. Examination is carried out for timely diagnosis of the disease and prompt treatment. He does not express concern about the severity and curability of his “illness,” unlike people with hypochondriacal disorder. They deny that they have a psychological problem as the cause of their symptoms. Somatization disorder is accompanied by a persistent low mood, and the development of depressive and anxiety disorders is possible.
Somatoform dysfunction of the autonomic nervous system. Accompanied by vegetative symptoms. The reason lies in the disruption of the functional state of organs controlled by the autonomic nervous system. Complaints are nonspecific, changeable, symptoms can be observed in various conditions and diseases (sweating, shortness of breath, tachycardia, slight increase in body temperature, change in blood pressure). The patient is convinced of the presence of a somatic illness, does not recognize the psychological nature of the disorder, but conflict is not clearly expressed. With this form of the disorder, da Costa syndrome, irritable bowel syndrome, etc. can be observed. Symptoms may be similar to the clinical picture of damage to a specific organ controlled by the autonomic nervous system.
Chronic somatoform pain disorder. The patient suffers from constant pain. The pain is localized in the same place, is debilitating, painful, and the nature and location do not change over time. There are no neurological or autonomic disorders.
Undifferentiated somatoform disorder. There are numerous complaints characteristic of the group of somatoform disorders, but they cannot be assigned to a specific form of the disorder. Complaints are numerous and variable, vegetative symptoms are subtle.
A person with somatoform disorder experiences emotional and physical torment, which only treatment from a specialist can cope with.
Painful and undifferentiated disorders often initiate in childhood and early adolescence. Pain disorder in girls manifests itself between 11 and 19 years of age, and in boys up to 13 years of age. Abdominal symptoms (nausea, abdominal pain, etc.) are more common in adolescence, as are headaches. Somatoform disorders are more common among girls than boys.
At the beginning of the disease, bodily sensations differ from normal ones only by a slight increase in the intensity of the manifestation. Close attention to “new” sensations in the body develops gradually as they are repeated. Over time, the sensations begin to cause an alarming reaction.
The further course of the disorder depends on the personality-neurotic characteristics (the greater the tendency to long-term experiences, the more likely it is to increase anxiety and a more acute reaction to symptoms). A long-term state of anxiety is always accompanied by autonomic disorders, which manifest themselves as functional disturbances in the functioning of various organs. Unlike the initial symptoms of the disease, disorders at a later stage can be confirmed by instrumental examination methods.
SDVNS in children
Often, somatoform autonomic disorder appears in children at puberty, that is, during the period of maturation. This is due to a hormonal surge and intensive growth of the body.
The following factors can provoke the process:
- heredity;
- stress;
- mental, physical stress;
- infections;
- bad habits;
- surgical interventions;
- large body weight;
- sedentary lifestyle;
- staying at the computer for a long time.
The appearance of teenagers is typical. If sympathy predominates, then the skin of such children is moist and oily, with acne. She alternately turns red and pale. A bluish tint appears. Cold, with a marbled pattern called a vascular necklace. When pressed with a finger, the skin turns pale and red dermographism is observed.
When parasympathetics dominate, the skin is dry, with pink or white dermographism. These children have an increased appetite, but they do not gain weight.
The disorder is accompanied by a sudden rise in temperature under the influence of stress. A typical occurrence is fainting.
All characteristic changes in internal organs are present.
The psycho-emotional sphere is also undergoing changes. Such a child becomes distracted and nervous. He quickly gets tired, drowsiness and apathy appear, and his memory deteriorates.
In most cases, the course of the disease is stable. But periodically panic attacks and crises occur:
- sympatho-adrenal - accompanied by tachycardia, elevated blood pressure, headaches, thirst, chills and hyperthermia. Anxiety and feelings of fear develop;
- vagoinsular – migraine-like attacks, nausea, vomiting, pain in the abdominal area. Hyperhidrosis, decreased blood pressure and fainting, slow heart rate, increased urine output, breathing disorders;
- mixed.
The attack can last up to several hours.
Causes of somatoform disorder
Somatoform disorder is a disorder in the somatosensory system, which is responsible for the perception of impulses coming from the body. Disturbances can occur in peripheral receptors and central sections, mutually reinforcing each other. Primary dystrophic changes in receptors occur for various reasons. Altered erroneous pain signals activate central pain maintenance mechanisms. Their hyperactivity increases the excitation of peripheral receptors, which leads to sensitization to pain.
Against the background of stress, a primary tension of the central regulatory mechanisms occurs, the threshold for the perception of physical discomfort decreases, which leads to the subsequent transmission of pathological excitation to the peripheral receptors of the somatosensory system. Normal tension or discomfort is perceived by the patient as pain and other symptoms of his “disease.” Over time, this perception of discomfort is reinforced by internal beliefs, so any unpleasant sensations begin to be regarded as pain. Somatic symptoms are very common among children and adolescents, who often have difficulty expressing their feelings and emotions through language.
There are three groups of factors that can provoke the development of somatoform disorders.
Heredity and personality traits. People with character traits such as asthenia, hysteria, dysphoria, and impressionability are at increased risk of developing somatoform disorders. Persons with a history of anxiety and emotional lability, genetically determined by the level of reactivity of the nervous system. Patients with somatoform disorders are often sensitive, pessimistic, demonstrative, and quickly become mentally exhausted.
Psycho-emotional factors. The presence of traumatic events, the characteristics of upbringing, the family situation, the nature of professional stress - all this can become a provoking factor in the development of the disorder. Psychogenic factors shape behavior patterns and ideas about the world around us.
The reason for the occurrence of somatoform disorders can be situations of loss of social status, unsuccessful attempts to realize themselves professionally. Chronic psychological trauma appears as a result of constant emotional and physical overstrain, demandingness, mismatch between needs and external conditions, situations of deprivation in childhood or, conversely, being the center of attention in the family circle.
The child’s symptoms may be a mirror manifestation of the illness of one of his loved ones. If a family member has physical health problems, somatic disorders, behavior with excessive concern about one's health or frequent visits to medical institutions, this can model similar behavior in the child.
Organic factors. These include previous injuries and illnesses, usually severe or with a long course, they can leave behind exhaustion of the body or psychological trauma.
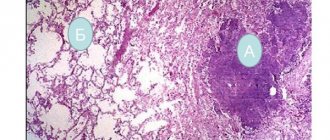
Atherosclerosis
When schizophrenia is combined with a cardiovascular disease such as atherosclerosis, a continuous type of mental illness predominates. Against the background of atherosclerosis, there is an introduction of age-related themes of delirium, a kind of poverty of the delusional system. Perception disorders become less legible, their individual identity is lost, and the phenomena of mental automatism become simplified.
The influence of the vascular factor is reflected in an increase in excitability, irritability, and a tendency to affective outbursts. Low mood is accompanied by weakness, tearfulness, dull headaches, and superficiality due to rapid exhaustion. The instability of emotions is combined with impulsiveness. Symptoms of the defect appear against an asthenic background; there is a surprising combination of inactivity with the inability to mobilize and fussy hyperactivity. Cynicism and emotional coldness are combined with the appearance of exaggerated politeness and condescension (Valeeva A.M., 2000).
The most pronounced influence of vascular pathology is noticeable in periodically relapsing schizophrenia.
Signs of vascular disease manifest themselves more clearly during attacks of psychosis than during remission. Memory impairment and short-term episodes of delirium are detected. With the addition of vascular pathology, attacks of schizophrenia become protracted, and the quality of remissions worsens. In paranoid schizophrenia, symptoms of vascular disorders can be interpreted in a delusional manner. Patients claim that dizziness, headaches, and heart pain occur as a result of exposure (Morozova V.D., 2000).
Diagnosis of somatoform disorder
The disease may remain undiagnosed for a long time due to the variety of symptoms, especially with somatization and undifferentiated somatoform disorders. The basis for the diagnosis of somatoform disorders is the collection of anamnesis and analysis of behavioral reactions. The presence of a disorder may be indicated by an improvement in condition after diagnostic examinations, ineffectiveness of treatment for a suspected somatic disease, uncertainty of complaints, or their dramatic change over time. The disorder may be accompanied by somatic illnesses, anxiety and depressive disorders.
It is important to pay attention to the presence of these clinical manifestations:
- Specific emotionally charged complaints about somatic malaise, autonomic dysfunctions, functional disorders (pain, cramps, muscle tremors, sleep disorders, appetite disorders, etc.) A person is fixated on any confirmation of his “diagnosis” and requires the appointment of examinations.
- The presence of manifestations of a mental disorder of the neurotic range (anxiety, fussiness, mood swings, irritability, short temper, apathy, fatigue, etc.)
- The presence of disorders of the somatosensory system. Sensopathy often manifests itself in the form of paresthesia (sensations of burning, burning, drilling, tingling, etc.). With paresthesia, the patient clearly points to the organ that is bothering him, describes the sensations clearly and emotionally. If discomfort is interpreted by the patient as pain, this is senestalgia. Senestalgia is distinguished by the location of pain and has its own name. With senestopathy, it is difficult for a person to describe what he feels; as a rule, the discomfort does not have a clear localization.
In the presence of pronounced somatic symptoms for two or more years, with social maladjustment and a persistent change in the emotional background, a diagnosis of somatization disorder is possible. If the disease lasts for at least six months and the clinical picture is atypical, an undifferentiated somatoform disorder is diagnosed. If a person experiences persistent anxiety about his health and fear of the “incurability of the disease,” a diagnosis of hypochondriacal disorder is made.
Differential diagnosis is carried out with the initial stages of somatic diseases, depression, hypochondriacal delirium and other mental disorders.
Hypertonic disease
According to Canadian scientists, the proportion of people with hypertension in schizophrenia is 13.7%; largely similar data were obtained from an epidemiological study of patients in the general medical network conducted by domestic researchers (Kozyrev V.N., 2002; Smulevich A.B. et al., 2005).
Other studies found that 34.1% of patients with schizophrenia were diagnosed with hypertension (Dixon L. et al., 1999). However, earlier M.D. Pyatov (1966) in his study showed that the combination of schizophrenia with hypertension is rare and amounts to only 2.65%. A similar point of view is shared by H. Schwalb (1975) and T. Steinert et al. (1996), who believe that cases of vascular hypertension in schizophrenia are relatively rare. According to some authors, hypotension in schizophrenia is due to the effect of antipsychotics, many of which affect alpha and muscarinic receptors.
Probably, such a scatter of statistical data reflects the same old question about the boundaries of schizophrenia and its diagnostic criteria. According to A.B. Smulevich et al. (2005), the difference in data regarding the prevalence of arterial hypertension is due to the population that falls into the field of view of researchers.
It should be borne in mind that such well-known risk factors for cardiovascular diseases as smoking, diabetes, a sedentary lifestyle, and lipid metabolism disorders occur quite often in patients with schizophrenia, which undoubtedly contributes to the development of this pathology.
In patients with schizophrenia who are treated in psychiatric hospitals, arterial hypertension is more malignant, and in outpatient settings its course is milder.
We support the point of view of those authors who consider the combination of hypertension with schizophrenia to be a relatively rare phenomenon. In our opinion, this is to some extent due to the psychosomatic nature of hypertension, which, for reasons that are not entirely clear, is not so typical for schizophrenia, either in terms of hereditary predisposition or in terms of the pathogenesis of the disease. However, in this case we again turn to the topic of the boundaries of schizophrenia and its differences from affective disorders.
If there is a combination of schizophrenia and hypertension, then the dynamics of the schizophrenic process, the course of hypertension and the expected outcome of the disease are often unpredictable.
According to some authors, the schizophrenic process takes on a clearly more favorable course here, with a softening of the main psychopathological symptoms, with the possibility of long-term remissions, especially in those cases where hypertension joins a long-standing process. A different picture is observed when schizophrenia and hypertension began almost simultaneously or when the latter preceded the former. Here the course of schizophrenia takes on a noticeably accelerated course, and its symptoms become pronounced. (Banshchikov V.M., Nevzorova T.A., 1962).
According to American authors, patients with schizophrenia with comorbid arterial hypertension today in almost 88% of cases do not receive drugs that stabilize blood pressure (Nasrallab H. et al., 2006).
Treatment of somatoform disorder
Treatment of somatoform disorder is long-term and carried out comprehensively, combining drug treatment and psychotherapy. Psychotherapy helps the patient reconsider his beliefs and physical sensations, and learn to cope with stress and anxiety. Pharmacotherapy eliminates anxiety and corrects mood. Drugs are selected according to the clinical picture.
At the Alter Mental Health Center, the method of psychotherapy is selected taking into account the form and severity of the somatoform disorder. Often used in treatment are cognitive-behavioral and dynamic therapy, training in relaxation skills, and group classes to improve communication and social skills.
Lack of timely treatment can lead to loss of performance, problems in social relationships, and the risk of developing concomitant mental disorders increases.
If you notice signs of somatoform disorder in yourself or your family, we will provide you with qualified assistance, of high quality and at an affordable price. Our clinic is located in the center of Moscow, on Vsevolozhsky Lane, next to the Kropotkinskaya metro station. The specialists at the Alter Mental Health Center are interested in your speedy recovery.