- Affective respiratory syndrome
Mental disorders accompanied by a sharp change in a person’s emotional state are classified as affective disorders. They can be characterized by a sharp change in dynamics, disturbances in the manifestations of standard human emotions. Treatment of affective disorder in a specialized clinic in most situations can give a favorable prognosis for improving well-being and self-perception.
Affective disorder syndromes
Depending on the prevailing symptoms, various syndromes of affective disorders are distinguished:
- Depression associated with metabolic disorders of brain tissue. Manifestations of depression are associated with the patient experiencing a state of extreme despondency and hopelessness. This syndrome is characterized by suicidal thoughts, often leading to attempts to end one’s existence. Without the necessary therapy, the syndrome can last for a long period.
- Dysthymia differs from depression in its milder form. The patient becomes depressed during the day, anxiety increases, and mood worsens.
- In bipolar disorder, the patient experiences alternating phases of depressed mood and euphoria. Previously, this disease was called “manic-depressive psychosis.” In a depressed state, the patient's mood is depressed. Moving into the manic stage, the patient becomes cheerful, often excessively active, aggression, delusional ideas and irritability appear. In the case of the maximum stage of manifestation of changes in states, bipolar disorder is called cyclomia.
- In the case of depressive disorders, the patient suffers from increased anxiety, fear, and internal restlessness. The patient constantly expects the onset of tragedy, impending disaster. In severe cases, movement disorder and panic attacks are possible.
- Cotard's syndrome is accompanied by nihilistic-hypochondriacal delusions, accompanied by ideas of enormity. Occurs in involutional melancholia and recurrent depression.
- Manic syndrome (mania) is accompanied by a high level of joyful mood. The patient suffers from an increased desire for constant activity, there is an increased level of optimism, cheerfulness, and inadequate joy. Attention is distracted, superficiality of judgments is visible, verbosity, hypermnesia, thoughts are not completed, fatigue is absent, the attitude towards oneself is idealized. There is a mild manic state (hypomania).
Affective disorders require immediate consultation with a specialist. They often become the debut of various mental disorders. They are capable of persisting throughout the entire period of subsequent mental illness.
Treatment
- Antipsychotics (eg, lithium, some anticonvulsants) and second-generation antipsychotics, or a combination of both
- Supportive treatment and psychotherapy
Treatment for bipolar disorder consists of three stages:
- Impact Treatment: Stabilization and Symptom Control
- Ongoing treatment: Achieving complete remission
- Maintenance treatment or prevention: Maintaining remission
Although most patients with hypomania can be treated on an outpatient basis, severe mania, like depression, often requires hospitalization.
Drug therapy for bipolar disorder
Medicines to treat bipolar disorder include:
- Mood stabilizers: lithium and some anticonvulsants, in particular valproate, carbamazepine and lamotrigine
- 2nd generation antipsychotics: Aripiprazole, Lurasidone, Olanzapine, Quetiapine, Risperidone and Ziprasidone
These drugs are prescribed either individually or in combination at all stages of treatment, although in different dosages.
Choosing drug treatment for bipolar disorder can be difficult because all medications have significant side effects, frequent drug interactions, and no one drug is universally effective. The choice should be based on what has previously been effective and well tolerated in a given patient. If the patient has not previously been prescribed medications for bipolar disorder (or the drug history is unknown), the choice depends on the patient's medical history (depending on the adverse effects of the specific mood stabilizer) and the severity of symptoms.
Some specific antidepressants (eg, SSRIs) are also prescribed to treat severe forms of depression, but their effectiveness is controversial; they are not recommended as the sole treatment for depressive episodes.
Other Treatment Options
Phototherapy is useful for the treatment of seasonal bipolar disorders type I or II (autumn-winter depression and spring-summer hypomania). This method is especially effective as an adjuvant treatment.
Education and psychotherapy
By enlisting the support of loved ones, the doctor can prevent the development of major episodes of mood disorders.
Group therapy is often recommended for patients . In these classes, they will learn about bipolar disorder, its consequences, and the important role of mood stabilizers in the treatment of this disorder.
Individual psychotherapy can help patients cope with life's difficulties and embark on a new path of self-awareness.
Patients, especially those with bipolar II disorder, have poor adherence to the prescribed regimen because they believe that these drugs make them less alert and creative. The doctor can explain that a decrease in creative abilities is relatively rare, because mood stabilizers help achieve harmony in the interpersonal, scholastic, professional and creative aspects of life.
Patients should be warned to avoid stimulant medications and alcohol to minimize sleep disturbances and to identify early signs of relapse.
If the patient is prone to squandering, then control of the family budget should be transferred to family members. Patients with sexual hyperactivity should be told about the consequences of this behavior for the family (eg, divorce) and the risk of contracting infectious diseases such as AIDS.
Support groups (for example, the Depression and Bipolar Disorder Support Network) can help patients by providing an opportunity to share experiences and feelings with other patients.
Treatment of mood disorders
In medical practice, treatment for affective disorders is developed individually for each patient. It is necessary to take into account the present symptoms and the presence of additional diseases. When developing a program, procedures are carried out to:
- stop the active stage of the disease, if present;
- eliminate the cause of the pathology;
- carry out psychotherapeutic work;
- with the help of social work, increase adaptive abilities.
The composition of an integrated approach to the treatment of all types of syndromes includes:
- use of drug treatment;
- psychotherapy;
- social rehabilitation.
In case of acute exacerbation, suicidal thoughts, hospitalization is recommended. Each type of disease requires separate approaches when developing a course.
Affective mood disorder
Almost everyone has experienced mood swings, often without specific reasons. In some cases, such changes, caused by fatigue or based on pleasant occasions, cease to be only one of the manifestations of the norm. In this situation, they require diagnostics and development of a treatment program.
The cause may be genetic predisposition or external factors. For example, a strong shock caused by the death of a loved one. The reason is joy.
To correct the condition, a personal conversation between a specialist and a doctor is required to establish an accurate diagnosis. Elimination of provoking factors allows the state of affect to be relieved. Treatment uses sedatives and antidepressants.
Affective mental disorder
In such a situation, the patient’s condition becomes pathological and interferes with his normal life activities. Therapy is often lengthy. Requires the use of pharmacological drugs.
As in other situations with this disease, first of all the patient is removed from the acute attack stage. Identification of causes that can become a provoking factor is carried out in consultation with a psychologist. The pathology is characterized by alternating periods of exacerbations and remissions. Supervision by a specialist at any stage and attendance at preventive examinations are required.
Affective spectrum disorders
In most cases, doctors try to eliminate manifestations of affective spectrum disorders in restrictive conditions. Hospitalization is required for acute manifestations. At the initial stage of confronting the pathology, relief drugs are used with combinations of neuroleptics and antipsychotics. The use of anticonvulsants of the Valproate group may be required.
In the presence of psychosomatic symptoms, second-generation antipsychotics are used. Such as Serdolex, Clopixol Acufaz. The second generation of these drugs has fewer side effects. Drug resistance after 4 weeks of use becomes a recommendation for the use of anticonvulsants. Lithium salt is prescribed.
Depressive affective disorder
Directly translated in Latin, depression is called “dejection.” This condition cannot be completely cured today, but it can be corrected and stopped. Therapy helps improve the psychological and physiological state of the patient. Using a combination of psychological and biological treatment. In addition to medicinal drugs, folk recipes are distinguished by a high degree of effectiveness. First of all, herbal soothing teas, yoga. Patients are shown psychotraining courses and soothing baths. Following the rules of a healthy diet and avoiding alcohol plays a positive role.
Organic affective disorder
Antidepressants are used in treatment. They improve emotional well-being and reduce anxiety levels. It is necessary to remove the factors that provoked the condition.
An organic affective state is caused by physiological factors. Such as a long-term illness, withdrawal of certain medications, consequences of traumatic brain injury, postoperative condition.
The prescription of medications is carried out taking into account the medications that the patient is forced to take in accordance with the main diagnosis. In most situations, doctors prefer to focus on the use of psychotherapy, soothing infusions and teas, and physiotherapeutic procedures.
Manic affective disorder
The problem for conducting a successful course is often the patient's rejection of the diagnosis. A full examination is carried out to exclude concomitant dementia or schizophrenia. During therapy, sessions with a psychotherapist and prescription of medications are used. Anticonvulsant therapy is recommended.
In case of severe cases, compulsory hospitalization is required. In such a situation, doctors need the support of the patient's relatives.
Emotionally affective disorders
With such a lesion, a maximum change in the perception of the surrounding world occurs. The reaction to the provoking factor becomes excessive. There is a loss of understanding of the surrounding situation, and at the same time the understanding of a person’s actions in the current situation decreases.
The provocateur is prolonged exposure to traumatic events, leading to a pathological reaction of the brain. The patient loses control and does not adequately evaluate the actions taking place. Among the provocateurs are the death of a loved one, a sharp decline in social status and material level, and the occurrence of hormonal imbalance. The therapy uses tricyclic antidepressants, antipsychotics, mood stabilizers, tranquilizers, and mood stabilizers.
In the absence of positive dynamics, anticonvulsant therapy is prescribed. Psychotherapy sessions are conducted both with the patient himself and with his environment.
Bipolar disorder treatment
Courses of mood stabilizers are used for therapy. Such as Carbamazepine, lithium therapy, valproic acid. Treatment is divided into the stage of removing the patient from the acute stage and further preventive therapy, which can be carried out for life. At this stage, the use of a lithium solution is recommended. When you stop taking it, about half of patients relapse within a few weeks. Complete withdrawal within 5 years leads to relapse in 94% of patients.
This remedy shows a positive effect in 60% of patients with short cycles and up to 20% of patients with long cycles. Additional medications are prescribed. With the high potency of lithium, its positive effect occurs approximately 5 days after the start of treatment. During this period, other medications are used. Constant monitoring of the effect of the drug on the body is required. Treatment should be discontinued if dysarthria, widespread tremor and ataxia appear. Most often, negative symptoms are observed in the elderly and patients with poor health.
Causes
As already mentioned, the main “culprit” of organic mood disorder is a physiological factor. The most common reasons:
- Brain damage – tumor, traumatic brain injury affecting the frontal lobes.
- Diseases of the endocrine system - Itsenko-Cushing's disease, thyrotoxicosis, consequences of partial or complete removal of the thyroid gland, premenstrual and menopausal syndrome.
- Long-term use of hormonal drugs or their withdrawal. Those who suffer from autoimmune diseases and are forced to take glucocorticosteroids are especially at risk.
- Overdose of antihypertensive drugs, rarely - antibiotics, sedatives, antitumor drugs, narcotic analgesics.
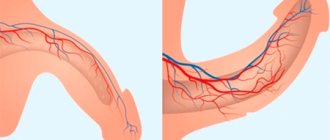
The above-mentioned circumstances negatively affect the state of neurotransmitters responsible for transmitting impulses between nerve cells, and from them to the glands and muscle tissue. An imbalance of these biologically active substances disrupts this process, and the parts of the brain responsible for instinctive behavior, feelings and emotions end up working incorrectly.
Excess serotonin and norepinephrine speed up neurotransmission, making receptors more sensitive. This contributes to a manic state. A deficiency of these hormones provokes depression.
Bipolar affective disorder symptoms
This disease leads to a person’s complete loss of orientation in the world around him. Suicidal thoughts arise, careers end, and interpersonal relationships are destroyed. The disorder provokes life-threatening antisocial behavior.
The main symptom is a sudden change in mood. Depression gives way to euphoria. The change of cycles is chaotic. The duration of the phases cannot be determined. Sometimes the phases last for years. In the interval between attacks, there are no outward manifestations of the diagnosis and the patient feels completely healthy.
During depression, irritability, unmotivated anger, hopelessness and embarrassment are noted. In the euphoric stage, the patient may be prone to excessive spending or uncontrolled sexual relations.
The physiological state changes during different phases. During the manic stage, the patient feels a surge of strength, he is overly active, mobile, laughs often, speech becomes loud, and movements are impulsive.
The depressive stage is characterized by a sharp loss of strength. It becomes difficult for a person not only to move, but also to think. The duration of the depressive state is about two weeks. A repetition of the change of state occurs in most cases at least once every two years with the most ideal course of the disease.
The onset of the disease often occurs at the age of 20-30 years. Relatives may mistake the condition for a mental disorder. On average, the disease affects two out of a hundred people.
Danger to yourself and others
The social significance of the clinical picture is great. If at the asthenic stage patients can take care of themselves, and many are able to work, then with increasing severity of the disease they can first become dangerous for people around them (explosive, euphoric stage), and later for themselves (apathetic stage) due to pronounced apathy and helplessness.
Therefore, organic mental disorders require timely correction. If there is one or another option, you need to contact a psychiatrist.
All materials on the site are presented for informational purposes only, approved by certified physician Mikhail Vasiliev, diploma series 064834, in accordance with license No. LO-77-005297 dated September 17, 2012, by a certified specialist in the field of psychiatry, certificate number 0177241425770.
Bipolar affective disorder diagnosis
The diagnosis is carried out by a psychiatrist or psychotherapist. When determining the diagnosis, the following is carried out:
- conversation with the patient and his environment;
- conducting a pathopsychological study by a clinical psychologist;
- laboratory tests are performed, including a blood test, neurotest, EEG, and a neurophysiological test system is prescribed;
- Consultations with a neurologist, cardiologist, and endocrinologist are necessary.
In difficult cases, it is recommended to undergo a medical commission that brings together several specialists. At the moment, signs of the disease cannot be detected using CT and MRI.
Symptoms of mood disorders
Accurate diagnosis of affective disorders is complicated by a wide range of causes that can provoke deterioration in health. The disease cannot be self-diagnosed. Only a psychiatrist or psychotherapist can give an accurate assessment. Specialists determine the exact diagnosis.
However, in medical practice there is a list of symptoms that suggest the presence of an affective disorder. Signs common to all types:
- mood changes occur with high frequency for a long period;
- the level of activity and mental pace decreases;
- a person’s perception of himself and situations changes dramatically;
- a noticeable decrease in the level of activity, depression, loss of interest in what is happening;
- appetite changes, usually decreases to complete starvation, but can also increase sharply;
- the patient is tormented by lack of sleep;
- moral suffering can lead to pain in any part of the body without any reason;
- sexual activity decreases, to complete asexuality.
Correct treatment can only be prescribed by a specialist after consultation.
Classification of organic mood disorder and symptoms
There are two degrees of severity of this pathology:
- psychotic – characterized by inappropriate reactions, lack of control of behavior, and uncriticality of the patient’s own condition;
- non-psychotic - although emotions are at their peak, the patient, understanding what is happening to him, can partially regulate behavior and comply with accepted norms in society.
As for the manifestations, they are as follows:
- manic - accompanied by a feeling of immense happiness, universal joy. The patient is hyperactive, fussy, in high spirits, behaves very relaxed, can literally move mountains;
- depressive - the individual is overcome with melancholy, he cannot do anything, he is depressed, sad, the mental sphere is depressed;
- bipolar - mania and depression cyclically replace one another;
- mixed or combined - the above states alternate chaotically.
The clinical picture of organic affective disorder depends on its form.
Depressed patients have a low mood, are apathetic, passive, sad, and show no interest in anything. It is difficult for him to perform physical and mental work; his head, as they say, does not cook, he is even dizzy. The muscles are sluggish and fatigue sets in quickly. The patient cannot concentrate and collect thoughts “in a heap”, thinks about the uselessness of his existence, is disappointed in life, blames himself for something. No appetite, can't sleep.
Manic disorder , on the contrary, is characterized by high mood, activity of thought and movement. The individual acts chaotically, quickly, but aimlessly. He thinks quickly, the process of cognition is accelerated, but shallow, since he cannot fully analyze anything. The behavior is impulsive, difficulties that arise encourage aggression. With the psychotic severity of the disorder, delusional states may occur.
If measures are not taken in time, then organic affective mood disorder is fraught with big problems. Depressed patients withdraw into themselves, do not want to contact anyone, and lie in bed all day long. Their condition may deteriorate so much that it may end in suicide. In manic patients, an outburst of aggression can lead to an antisocial act or crime. Unable to resist the excitement, they start fights, damage other people's property, etc.
Types of Mood Disorders
All types of affective disorders are described in the international classifier under the ICD 10 code, episodes F30-39. According to the classifier, types are defined as follows:
- F30 manic episode, diagnosed only in the case of a one-time manifestation of the disease; if repeated, doctors establish the fact of bipolar disorder;
- F31 bipolar mental disorder, characterized by recurrent occurrences;
- F32 depressive episode, accompanied by a decrease in activity, the presence of a depressed mood, increased fatigue, decreased appetite, insomnia, decreased self-confidence and self-esteem. It can be mild, pronounced and severe.
- F33 recurrent depressive disorder is defined by the presence of recurrent episodes of depression. There are no mood swings, with the change from mania to euphoria. The onset of the disease is possible at any age. Including in childhood. With a manic episode, especially if it recurs, it is classified as bipolar disorder.
- F34 persistent mood disorders that last for years, often throughout life, but are not severe enough to be classified as a mild depressive episode or a hippomanic episode.
- F38 Other mood disorders that do not fall into the types listed.
- F39 NOS (affective psychosis).
The diagnosis is made in a clinical setting. Accurate diagnosis is carried out only by a qualified psychotherapist or psychologist.
Publications in the media
Mood disorders are disorders in which the main disturbance is a change in affect or mood towards elevation (mania) or depression (depression), accompanied by a change in the general level of activity. Depressive and manic states can occur in many somatic and almost all mental illnesses, and can also be caused by drugs (for example, narcotic analgesics, antihypertensives, antitumor drugs, sedatives, antiparkinsonian drugs, antibiotics, antipsychotics, GCs).
Frequency. The lifetime risk of developing various forms of mood disorders is 8–9%. Women get sick 2 times more often with a predominance of depressive variants. Only 20% of patients go to medical institutions, half of them do not realize the nature of their disease and present somatic complaints, and only 30% are recognized by a doctor. 25% of patients receive adequate therapy. CLINICAL PICTURE The clinical picture of mood disorders includes depressive and manic syndromes. Depressive syndromes Depending on the number and severity of symptoms, depressive syndromes are classified as mild, moderate and severe. • Moderately severe depressive syndrome •• Decreased mood with a feeling of melancholy, slower pace of thinking and motor retardation are the main signs of depressive syndrome •• The appearance of patients is characteristic: a sad expression on the face, a suffering vertical fold between the eyebrows, hunched posture, head down, gaze fixed down. Despite their difficult mental state, some patients are able to joke and smile (“smiling depression”) •• Motor retardation is a common symptom of depression (although agitation, described below for agitated depression, is not excluded). The patient's movements are slow and performed only when absolutely necessary. With severe motor retardation, patients spend most of their time lying in bed or sitting, without feeling the need for active action. The slowing down of the pace of thinking is reflected in the speech of patients: questions are answered with a long delay, after long pauses •• Patients are especially painfully experiencing a depressed mood with a feeling of melancholy. Patients rarely describe their condition as low mood. More often they complain of sadness, a feeling of melancholy, lethargy, apathy, depression, depression. Melancholy is described by patients as mental heaviness in the chest, in the area of the heart, in the head, sometimes in the neck or abdomen; explain that this mental, “moral” pain •• Other common symptoms of depression are anxiety (see Anxiety disorders) and irritability. The increase in anxiety most often occurs in the evening. As depression deepens, anxiety turns into agitation: patients in this state are unable to sit still, rush about, moan, and wring their hands; often attempt suicide in the presence of medical personnel or other persons. Irritability in depression is manifested by constant irritation, gloominess, dissatisfaction with oneself and others •• Loss of interests and the ability to have fun. Patients complain about their insensitivity, say that the feelings of other people are inaccessible to them, everything around them loses value (here this condition should not be confused with emotional emptiness in patients with schizophrenia). In severe cases, patients claim that they have lost love for people previously dear to them, have ceased to feel the beauty of nature, music, and have generally become insensitive; talking about this, patients have a hard time experiencing their change, so this condition is called painful mental insensitivity (anaesthesia psychica dolorosa) •• Almost all patients with depression complain of decreased energy, it is difficult for them to start something, to finish what they started; academic performance and productivity decreases. Many patients attribute their lack of energy to some physical illness. •• With depressive syndrome, biological symptoms are often observed. These include sleep disorders (early awakenings are the most typical: the patient wakes up 2-3 hours before the usual time of awakening and can no longer fall asleep, experiences anxiety, restlessness, thinks about the coming day), diurnal mood swings (deterioration of mood in the morning), decreased appetite, weight loss, constipation, amenorrhea, decreased sexual function •• Depressive thoughts (depressive thinking) are an important symptom of depression. Identifying depressive thoughts helps the doctor predict and prevent possible suicide attempts. Depressive thoughts can be divided into three groups ••• The first group relates to the present time. Patients perceive their surroundings in a gloomy light and are focused on thoughts of self-deprecation. For example, the patient believes that he cannot cope with his work, and those around him consider him a failure, despite obvious successes ••• The second group concerns the future tense. Patients completely lose hope for anything good in the future, are filled with a feeling of hopelessness, the hopelessness of their situation and the aimlessness of further life. For example, the patient is sure that in the future he will become unemployed or get cancer). Suicidal attempts during depression are most often caused by this particular group of depressive thoughts ••• The third group refers to the past tense. Patients experience an inappropriately strong feeling of guilt, remembering minor misdeeds from a past life, cases when they behaved insufficiently ethically, made mistakes, etc. •• Complaints about somatic symptoms are often noted in depression. They can be very diverse, but the most common complaints are constipation and pain (or discomfort) in any part of the body •• With depressive syndrome, other mental disorders are observed: depersonalization, obsessive states (see Obsessive-compulsive disorder), phobias (see Disorders phobic), etc. •• Patients often complain of memory impairment, which is associated with impaired concentration. However, if the patient makes an effort, then the processes of memorization and reproduction themselves turn out to be intact. But sometimes these memory impairments, especially in the elderly, become so severe that the clinical picture is similar to dementia. • Masked depression •• Masked (larved, hidden) depression is a subdepressive state combined with somatic disorders dominant in the clinical picture that mask low mood. The frequency of masked depression exceeds the number of overt depression by 10–20 times. Initially, such patients are treated by doctors of various specialties, most often by therapists and neurologists. Masked depression is most often observed in mild and moderate depressive syndrome, and much less frequently in severe depressive syndrome. •• The most common complaints are complaints about disorders of the cardiovascular system (attacks of pain in the heart) and digestive organs (decreased appetite, diarrhea, constipation, flatulence, abdominal pain). Various sleep disorders are very often noted. Patients complain of a feeling of loss of strength, weakness, loss of interest in favorite activities, a feeling of vague anxiety, rapidly developing fatigue when reading a book or watching television •• There are often cases when masked depression causes alcohol abuse.
• Severe depressive syndrome •• With further development and severity of the depressive syndrome, all of its symptoms described above appear with greater intensity. A distinctive feature of severe depressive syndrome is the addition of psychotic symptoms: delusions and hallucinations (therefore, some authors call this disorder the term “psychotic depression”) •• Delusions in severe depressive syndrome are represented by ideas of self-abasement, guilt, the presence of severe somatic diseases (hypochondriacal delusions) •• With severe depressive syndrome, patients most often experience auditory hallucinations, the content of which reflects the painful depressive state of the patients. For example, a patient hears a voice reporting the hopelessness and meaninglessness of his suffering, recommendations to commit suicide, or the groans of dying loved ones, their calls for help, etc. Much less often, patients experience visual hallucinations, which also reflect a depressive mood (for example, scenes of death or execution). • Agitated depression - depression with agitation. Agitation is motor restlessness combined with anxiety and fear. Patients are extremely tense and do not find a place for themselves: they stereotypically rub their hands, finger their clothes with their hands, walk a lot, persistently turn to the staff and others with some kind of request or remark, sometimes they stand at the doors of the department for hours, shifting from foot to foot and grabbing clothes passing.
• Inhibited (adynamic) depression. With inhibited depression, the leading symptom is psychomotor retardation. In some cases, the severity of psychomotor retardation reaches the level of stupor (depressive stupor). If symptoms reverse during treatment, when depression is still strong and motor retardation disappears, the risk of suicide increases sharply! • Mild depressive syndrome (subdepression) - depression of mild severity. The affect of deep melancholy and motor retardation are absent, outwardly the behavior of patients can remain orderly, although devoid of energy and activity. The patients' condition is dominated by anhedonia, lack of mood, anxiety, and self-doubt. Patients note that in the morning it is difficult to force themselves to get out of bed, get dressed, and wash; Carrying out the usual duties at home and at work requires a lot of effort, there are no desires, there is no confidence in the success of any undertaking. When waking up, there is no sensation of transition from sleep to wakefulness - hence the unfounded complaints of “complete insomnia.” Anxiety, common in subdepression, is often accompanied by hypochondria, obsessive thoughts and phobias.
Manic syndrome Manic syndrome is a combination of elevated mood, accelerated tempo of thinking and increased motor activity. • Patients' appearance often reflects elevated mood. Patients, especially women, tend to dress brightly and provocatively, and use cosmetics excessively. The eyes are shiny, the face is hyperemic, and when talking, splashes of saliva often fly out of the mouth. Facial expressions are lively, movements are fast and impetuous, gestures and postures are emphatically expressive. • High spirits are combined with unshakable optimism. All the experiences of patients are painted only in rainbow tones. Patients are carefree and have no problems. Past troubles and misfortunes are forgotten, the future is painted only in bright colors. Patients describe their own physical well-being as excellent; the feeling of excess energy is a constant phenomenon. At first glance, such patients may give an outside observer the impression of being mentally healthy, but unusually cheerful, cheerful and sociable. Other patients experience irritability and easily develop reactions of anger and hostility. Orientation, as a rule, is not impaired, but consciousness of the disease is often absent. • Increased motor activity - patients are constantly on the move, cannot sit still, walk, interfere in everything, try to command the patients, etc. During conversations with a doctor, patients often change their position, spin, jump up, begin to walk and often even run around the office. They take on any task, but only move from one thing to another, without bringing anything to the end. Patients with manic syndrome are very willing to communicate with others and actively intervene in conversations that do not concern them in any way. • Acceleration of the pace of thinking - patients talk a lot, loudly, quickly, often without stopping. With prolonged speech stimulation, the voice becomes hoarse. The content of the statements is inconsistent. Easily move from one topic to another. With increasing speech excitement, a thought that does not have time to finish is already replaced by another, as a result of which statements become fragmentary (“jump of ideas”). The speech alternates with jokes, witticisms, puns, foreign words, and quotes.
• Sleep disturbances manifest themselves in the fact that patients sleep little (3–5 hours a day), but at the same time they always feel cheerful and full of energy. • With manic syndrome, an increase in appetite and increased sexual desire are almost always noted. • Expansive ideas. The possibilities for realizing numerous plans and desires seem limitless to patients; patients do not see any obstacles to their implementation. Self-esteem is always overly elevated. It is easy to overestimate your capabilities - professional, physical, related to entrepreneurship, etc. For some time, patients can be dissuaded from exaggerating their self-esteem. Expansive ideas easily turn into expansive delusions, which are most often manifested by delusional ideas of greatness, invention and reform. • In severe manic syndrome, hallucinations are noted (rarely). Auditory hallucinations are usually of praising content (for example, voices telling the patient that he is a great inventor). With visual hallucinations, the patient sees religious scenes. • The hypomanic state (hypomania) is characterized by the same features as severe mania, but all symptoms are smoothed out, there are no gross behavioral disorders leading to complete social maladjustment. Patients are active, energetic, prone to jokes, and overly talkative. The increase in their mood does not reach the level of conspicuous indomitable gaiety, but is manifested by cheerfulness and optimistic faith in the success of any undertaking. Many plans and ideas arise, sometimes useful and reasonable, sometimes overly risky and frivolous. They make dubious acquaintances, lead an indiscriminate sex life, begin to abuse alcohol, and easily take the path of breaking the law.
CLASSIFICATION OF MOOD DISORDERS Classifications based on etiology • Endogenous and reactive depression. The terms “endogenous” and “reactive” are not included in the modern classification of mental illnesses, but some psychiatrists still use these concepts. With endogenous depression, symptoms are caused by factors not related to the patient’s personality and do not depend on the traumatic situation. In reactive depression, symptoms are directly related to traumatic situations. In practice, only endogenous or only reactive depressions are rare; Mixed depression is much more common. • Primary and secondary depressive syndromes. Secondary depressive syndromes are caused by another mental disorder (for example, schizophrenia, neurosis, alcoholism), a somatic or neurological disease, or the use of certain drugs (for example, GCs). In the case of primary depressive syndrome, it is not possible to detect any cause that caused the depression.
Classification based on symptoms • Neurotic and psychotic depression. With neurotic depression, the symptoms characteristic of psychotic depression (severe depressive syndrome) are more smoothed out, less pronounced, and are often caused by traumatic situations. Neurotic depression is often accompanied by neurotic symptoms such as anxiety, phobias, obsessive-compulsive disorder and, less commonly, dissociative symptoms. In the modern ICD-10 classification, neurotic depression is described as “dysthymia”.
Classification based on course • Bipolar mood disorder •• In the previous ICD-10 classification, these disorders were described under the term “manic-depressive psychosis.” Bipolar mood disorder manifests itself in alternating manic or depressive phases (episodes). Episodes can immediately follow each other (for example, a depressive state is immediately replaced by a manic syndrome) or at intervals of complete mental health (for example, a patient has emerged from a depressive state and after a few months a manic syndrome develops). The disorder does not lead to a decrease in mental functions even with a large number of phases experienced and any duration of the disease •• Bipolar disorders usually begin with depression. To make a diagnosis of bipolar disorder, the development of at least one manic (or hypomanic) episode during the course of the disease is sufficient. • Cyclothymia (cyclothymic disorder) is characterized by a chronic course with numerous and short-lived episodes of hypomanic and subdepressive states. Cyclothymia can be thought of as a milder version of bipolar disorder. Clinical manifestations are similar to those of bipolar mood disorder, but they are either less pronounced or less persistent. The duration of the phases is significantly shorter than in bipolar disorder (2–6 days). Episodes of disturbed mood occur irregularly, often suddenly. In severe cases, there are no “bright” intervals of normal mood. The onset of the disease is usually gradual and occurs between the ages of 15 and 25 years. 5–10% of patients develop drug addiction. The history indicates frequent changes of residence and involvement in religious and occult sects. • Depressive disorders •• Recurrent depressive mood disorder (unipolar depression, unipolar mood disorder) is a disease that occurs in the form of several major depressive episodes throughout life, separated by periods of complete mental health. The first episode can occur at any age, from childhood to old age. Its onset can be acute or unnoticeable, and its duration can range from several weeks to many months. The risk of a person with recurrent depressive disorder never having a manic episode is never completely eliminated. If this happens, the diagnosis is changed to bipolar affective disorder. Depressive disorders do not lead to a decrease in mental functions even with a large number of phases experienced and any duration of the disease •• Seasonal affective disorder - depression that occurs in winter, with a reduction in daylight hours. Decreases and disappears with the onset of spring and summer. Characterized by drowsiness, increased appetite and psychomotor retardation. Associated with pathological metabolism of melatonin •• Currently, neurotic depression and erased forms of recurrent depressive disorder are combined into dysthymic disorder. In the ICD-10 classification, neurotic depression (depressive neurosis) is included in dysthymic disorder (dysthymia). Dysthymia is a less severe form of depression, usually caused by a long-term traumatic situation. The disorder tends to be chronic. With dysthymia, the symptoms characteristic of severe depressive syndrome are more smoothed out and less pronounced.
DIFFERENTIAL DIAGNOSTICS OF MOOD DISORDERS • Grief reaction. Depressive disorders must be distinguished from the normal grief reaction to severe emotional stress (for example, the death of a child). The grief reaction differs from depressive disorder in the absence of thoughts of committing suicide; patients are easily persuaded, and their condition is alleviated when communicating with other people. Treating grief-stricken patients with antidepressants is ineffective. Some patients with grief reactions subsequently develop major depressive disorder. • Anxiety disorder can be difficult to distinguish from subdepressive conditions, especially since anxiety and depression often co-occur. To make a correct diagnosis, it is necessary to assess the severity of anxiety and depression, as well as the sequence of their onset. If the patient’s symptoms of depression are more pronounced and appear first, and then anxiety joins in, then a diagnosis of depressive disorder is more likely. Conversely, if the disease begins with symptoms of anxiety, which are the only manifestations of the clinical picture, and then symptoms of depression appear, then the patient most likely has an anxiety disorder. The same principle is used in the differential diagnosis of obsessive-compulsive and phobic disorders. • Schizophrenia. Delusions and hallucinations are observed in both manic and depressive episodes. Mood disorders do not lead to a decrease in mental functions even with a large number of phases experienced and any duration of the disease. Whereas in schizophrenia, negative symptoms are observed, leading to persistent personality changes. • Schizoaffective disorder. In cases where the clinical picture shows equally pronounced symptoms of a mood disorder (manic or depressive syndrome) and schizophrenia, a diagnosis of schizoaffective disorder is more likely (see Schizoaffective disorder). • Dementia. Memory impairments in depression have a more acute onset and are caused by impaired concentration; The clinical picture also includes other symptoms of depression, such as depressive thinking. Patients with depression who complain of memory impairment usually do not hesitate to answer questions (“I don’t know”), while patients with dementia try to avoid a direct answer. In depressed patients, memory for current and past events is equally impaired; Dementia patients suffer more from memory for current events than for past ones. • Organic brain damage. When a manic state appears in old age in combination with severe behavioral disturbances (for example, public urination) and especially the absence of a history of manic and depressive episodes, one should think first of all about organic damage to the brain (most often the frontal lobe - “frontal lobe syndrome”), for example a tumor. In this case, additional studies are carried out - MRI/CT, EEG. • Mood disorders caused by substance abuse (eg, heroin, amphetamine). Substance abuse and dependence are typically accompanied by mood disorders. In differential diagnosis, anamnesis data and the results of urine tests for the content of psychoactive substances are taken into account. • Mood disorders caused by drug use. When assessing the patient’s condition, it is necessary to find out what medications he is currently taking, which ones in the past, and whether he has previously had changes in mental well-being while taking any drugs. It is important to adhere to the principle that every drug that the patient takes can be a factor causing a mood disorder.
Research methods • Laboratory methods •• General blood and urine tests •• Dexamethasone suppression test •• Study of thyroid function •• Determination of vitamin B12, folic acid • Special methods •• ECG •• EEG •• CT/MRI • Psychological methods •• Zung Self-Esteem Scale •• Hamilton Depression Scale •• Rorschach Test •• Thematic Apperception Test. Differential diagnosis • Neurological diseases (eg, epilepsy, hydrocephalus, migraine, multiple sclerosis, narcolepsy, brain tumors) • Endocrine disorders (eg, adrenogenital syndrome, hyperaldosteronism) • Psychiatric diseases (eg, dementia, schizophrenia, personality disorders, schizoaffective disorder, adjustment disorder with depressive mood). COURSE AND PROGNOSIS Depressive disorders. 15% of people with depression commit suicide. 10–15% make suicide attempts, 60% plan suicide. It should be remembered that the likelihood of suicide is greatest during the recovery period during treatment with antidepressants. A typical depressive episode, if left untreated, lasts about 10 months. At least 75% of patients experience a second episode of depression, usually within the first 6 months after the first. The average number of depressive episodes during a lifetime is 5. The prognosis is generally favorable: 50% of patients recover, 30% do not recover completely, and in 20% the disease becomes chronic. Approximately 20–30% of patients with dysthymic disorder develop (in decreasing frequency) recurrent depressive disorder (double depression), bipolar disorder. Bipolar disorders. About a third of people with cyclothymia develop bipolar mood disorder. In 45% of cases, manic episodes recur. Manic episodes, if left untreated, last 3–6 months with a high likelihood of relapse. Approximately 80–90% of patients with manic syndromes eventually develop a depressive episode. The prognosis is quite favorable: 15% of patients recover, 50–60% do not recover completely (numerous relapses with good adaptation between episodes), in a third of patients there is a possibility of the disease becoming chronic with persistent social and labor maladjustment.
TREATMENT Basic principles • Combination of drug therapy with psychotherapy • Individual selection of drugs depending on the prevailing symptoms, effectiveness and tolerability of drugs. Prescription of small doses of drugs with a gradual increase • Prescription for exacerbation of drugs that were previously effective • Revision of the treatment regimen if there is no effect within 4-6 weeks Treatment of depressive episodes • TAD - amitriptyline and imipramine. For psychomotor agitation, anxiety, restlessness, irritability or insomnia, amitriptyline is prescribed - 150–300 mg/day; for psychomotor retardation, drowsiness, apathy - imipramine 150–300 mg/day • Selective serotonin reuptake inhibitors. If depression is resistant to treatment with high doses of amitriptyline or imipramine, this does not mean that newer antidepressants will be effective in this case. The development of anticholinergic side effects is the main reason for unauthorized discontinuation of TAD treatment. In addition, amitriptyline and imipramine are contraindicated in patients with heart disease, glaucoma and prostatic hypertrophy. It is preferable for such patients to be prescribed selective serotonin reuptake inhibitors, because they are more secure. Selective serotonin reuptake inhibitors are as effective as imipramine and amitriptyline, do not cause anticholinergic side effects, and are safer in overdose. The drugs are prescribed once in the morning: fluoxetine 20–40 mg/day, sertraline 50–100 mg/day, paroxetine 10–30 mg/day. • MAO inhibitors (eg, nialamide 200–350 mg/day, preferably in 2 doses morning and afternoon) are usually less effective for severe depressive disorders than TADs, and have the same effect for mild disorders. But in some patients resistant to TAD treatment, MAO inhibitors have a therapeutic effect. The effect of drugs in this group develops slowly and reaches a maximum by 6 weeks from the start of treatment. MAO inhibitors enhance the effect of vasoconstrictor amines (including tyramine, found in some foods - cheese, cream, coffee, beer, wine, smoked meats, red wines) and synthetic amines, which can lead to severe arterial hypertension. • Electroconvulsive therapy (ECT). Clinical studies have shown that the antidepressant effect of ECT develops faster and is more effective in patients with severe depressive disorder with delusional ideas than with TAD. Thus, ECT is the method of choice in the treatment of patients suffering from depressive disorder with psychomotor retardation and delirium when drug therapy is ineffective. Synonym. Affective Disorders Abbreviations . ECT - electroconvulsive therapy
ICD-10 • F06.3 Organic mood disorders [affective] • F30 Manic episode • F31 Bipolar affective disorder • F32 Depressive episode • F33 Recurrent depressive disorder • F34 Persistent mood disorders [affective disorders] • F38 Other mood disorders [affective] • F39 Mood disorder [affective] unspecified.
Diagnosis of affective disorders
In the case of sudden mood swings, the presence of affective disorders can be assumed. Common to all types of these diagnoses is a possible connection with seasonality. Exacerbations are often associated with climatic changes in natural conditions. Activation of the diagnosis is directly related to stressful situations in most patients.
The patient or his relatives can only assume the possible presence of such a diagnosis. For an accurate determination, a visit to the doctor is required. Installation is carried out after a personal consultation with a psychologist or psychotherapist. Mood disorders cannot be completely cured. In order to exclude relapses, observation by a doctor will be lifelong.
To establish a diagnosis, laboratory tests are performed: EEG, blood test. First of all, they are designed to exclude the presence of additional diagnoses. MRI or CT scans are not used for research.
Affective personality disorder
Mood dysregulation affects many people throughout their lives. Impressionable citizens who are prone to heightened perception of what is happening suffer from such changes or are simply different. But not all cases of dysregulation are clinical.
The pathology is characterized by a noticeable and cyclical change of depression and euphoria. In the absence of treatment, such changes can occur even without additional provoking factors.
Patients suffering from affective personality disorder of any type are rarely able to control the change in their condition. To monitor the condition, observation by a specialist is required in order to promptly initiate drug treatment. Affective personality disorder without treatment leads to the destruction of the patient’s personality. It reduces the quality of life and destroys personal and social life. Periods of low and high energy destroy the body, often leading to suicidal tendencies.
Causes of affect
Among the causes of affect are:
- The emergence of circumstances that threaten a person’s physical existence, related to his biological instincts and needs.
- Conflict, contradiction between a person’s strong attraction, desire, desire for something and the objective impossibility of satisfying the urge that has arisen.
- Actions of others that affect a person’s self-esteem and traumatize his personality.
Affect arises in an already existing specific situation and serves for the subject as a unique form of exit from it, a release. In an affectogenic situation, a person must act and feels an irresistible need to do so, but does not find suitable methods of action. This contradiction is what causes the affect. If a person clearly sees the possibilities of adequate behavior, affect does not occur.
Individual psychological characteristics predisposing to the development of affective states are:
- A complex of innate properties of the nervous system (in people with a weak type of nervous system, which is characterized by mild excitability, increased sensitivity to stimuli, low resistance to strong stimuli).
- The specific structure of personality, in particular, the features of its self-esteem.
- Age characteristics of the subject.
- Temporary functional psychophysiological states that disrupt a person’s resistance to an affectogenic situation (fatigue, insomnia, menstrual periods in women, etc.).
Seasonal affective disorder
It is observed in people prone to seasonal depression. The periods occur at approximately the same time of year. Within the general disorder it is classified as F32.1.
There are two types. The most common is winter, starting in the autumn months. Typically in September and October. The active period lasts until early spring. Much less common is the summer type, which lasts from early spring to late autumn.
The first attack in most cases occurs between 15 and 55 years. The average age of patients first presenting with seasonal affective disorder is 23 years. The risk of developing the disease decreases with age. Depending on the season, women suffer from depression more often than men.
About a third of patients tolerate seasonal depression quite easily. The disease manifests itself in the form of some loss of strength and deterioration in mood. Most patients experience seasonal depression with difficulty. They worsen the quality of life, destroy personal relationships, and ruin careers.
At risk are:
- people with a family history of mood disorders and GAP;
- residents of northern latitudes, where daylight hours are very short most of the day.
Patients suffer from decreased libido, increased drowsiness, hypochondria, and continued fatigue despite long periods of rest. Autonomic disorders are observed.
This type of affective disorder in most situations goes away completely on its own after the season ends.
As a result, it is worth noting that with proper treatment, affective disorders are successfully corrected, moving into a state of stable remission. To avoid relapses, patients require constant medical supervision, compliance with recommendations and, if necessary, taking medications.
Affective syndrome is a fairly common cause of disruption of the human body. It is characterized by the onset of changes in the functioning of the brain at the dienfective level. Due to this, the regulation of the biotones of the body is disrupted; due to a decrease in their regulation, mood and the pace of mental processes occur. Treatment of affective syndrome is carried out under the supervision of specialists.
History of affect
Historical reference. At the beginning of the 20th century, among the various “feelings”, affects began to stand out as an independent group. Affects were spoken of as emotional reactions aimed at defusing the emotional arousal that had arisen. According to Witwicki, affect is a sensory state that “acquires very significant strength and becomes a general violent disturbance of mental life.” He classified fear, horror, anger, etc. as affects. K. Stumpf, considering feelings a type of sensation, identified affects as a special type of mental phenomena. Gradually, the idea of some independence of affect became established, and when classifying emotional phenomena, it began to be distinguished along with emotional tone, mood, and emotions themselves. In addition to other well-known signs of affects, A. N. Leontiev identifies one that, in his opinion, distinguishes them from emotions: affects arise in response to a situation that has already actually occurred and in this sense are, as it were, shifted towards the end of the event, while emotions anticipate events that have not yet occurred. Emotions and affect are also shared by A. Sh. Tkhostov and I. G. Kolymba. From their point of view, both of these emotional phenomena represent extreme points of a continuum, “defining the main differences. Then affect appears as an uncontrollable, often pointless experience that forms the natural basis of emotions.”
Manifestation of affective syndrome
Pathology manifests itself in the form of negative emotional disorders, depressive states and mania. In some cases, accompanied by physiological disorders:
- difficulty breathing with a feeling of incomplete inspiration;
- heaviness in the chest;
- inhibition of movements and reactions;
- slowing down thought processes;
- loss of interest in things that were previously important to the patient.
Various types of depressive states manifested in pathology:
- manic-depressive psychoses;
- psychogenic depression;
- endogenous depressive states;
- depression of a somatic nature.
It is characterized by a sharp change, often occurring within one day. The period of attacks can last for several months and even years. Sleep disturbances are observed, appetite changes, and weight loss may occur.
Treatment of affective syndrome
When eliminating pathology, complex therapy is used with the use of medications and psychological training. Patients with mental disorders manifested in panic attacks are prescribed classes to master self-regulation techniques. Work is being done to improve self-esteem.
Social adaptation is used for successful therapy. In such a situation, the participation of family members and the patient’s immediate environment is recommended in group psychological trainings.
Affective syndrome in children
Affective disorders of depressive and manic types occur not only in adult patients, but also in children. Medicine is not able to accurately determine the cause of these disorders in minors. Provoking factors include genetic predisposition and constant traumatic situations. Manifestations are observed at the earliest stages of child development. The period from 12 to 20 months is especially dangerous for the start of the diagnosis.
The unstable psycho-emotional state of the baby with frequent mood swings allows one to suspect the presence of a diagnosis. Children suffer from hallucinations. Attacks may occur over significant time intervals. Immediate medical attention is required:
- in case of threats to commit suicide;
- attempts to cause physical harm to oneself;
- identifying cases of hallucinations.
Treatment is carried out jointly by a child psychologist, a psychiatrist, and a pediatrician. Due to the lack of a clear understanding of the causes of the onset of the disease, there are no preventive measures. If the disease is detected early, the prognosis is favorable. The combination of drug therapy and psychological practices makes it possible to reverse the development of pathology in a child.
A type of affective syndrome
Diagnosis and successful initiation of treatment for affective syndrome is associated with a clear definition of the type of pathology.
Affective respiratory syndrome
The cause of the onset of pathology is a serious psycho-emotional stimulus. Accompanied by attacks of suffocation, panic attacks caused by the inability to continue normal breathing. It occurs quite rarely in adult patients, due to the acquisition of the skill to control one’s emotional state in the event of sudden moral and physical shocks.
Affectively delusional syndrome
A polymorphic psychotic disorder, often caused by schizophrenia. Manifestations in situations of diagnosing delirium and depression in patients suffering from various mental illnesses.
Affectively paranoid syndrome
Refers to exacerbations in recurrent and schizophrenia, acute paraphrenia and other psychiatric diagnoses. It manifests itself as symptoms of switching off consciousness in the form of coma, a state of stupor, hypochondria, and a constant feeling of guilt. Accompanied by movement disorders. Such as agitation, the speed of associations changes from complete slowdown to acceleration at the level of a “whirlwind of ideas.”
Affectively endogenous syndrome
Occurs with endogenous diagnoses, somatogenic mental pathologies. Accompanied by frequent changes in mood phases. The maximum duration of depressive periods lasts up to 6 months. During the period of remission, the pathology may be virtually invisible.
Affective respiratory syndrome in children
It is a frequent response of the body to sudden provoking situations in the form of holding or even stopping breathing. This manifestation also occurs in a situation of prolonged prolonged crying. May be accompanied by convulsions and loss of consciousness. In rare situations, it turns into epilepsy.
Affective instability syndrome
A state of emotional instability that is on the verge of normal. It is recommended to contact a specialist:
- in case of frequent breakdowns, the so-called “crazy”;
- affective outbursts;
- mood swings, often occurring at an unconscious level;
- low level behavior control.
Manifestations in most situations are associated with stressful conditions and weather changes. Unstable psychopathy borders on schizophrenia.
Affective depressive syndrome
Constantly depressed mood, energy and performance decrease, often patients are characterized by a refusal to control their appearance. Ungrooming appears. The mood does not improve in pleasant company. Thoughts about suicide often appear.
Affective pathology syndromes
Extremely diverse. A common symptom is a disturbance in the emotional state from a state of excessive joy to deep depression. If frequent mood swings are detected, it is recommended to consult a specialist for an accurate diagnosis.
Affectively hallucinatory syndrome
It is characterized by a combination of delusional and hallucinogenic disorders. Patients may experience visual and auditory hallucinations, decreased emotional status, or, conversely, increased agitation.
Diagnostics
- Clinical criteria (Diagnostic and Statistical Manual of Mental Disorders, 5th edition)
- Thyroxine (T4) and TSH levels to rule out hyperthyroidism
- Exclusion of the fact of use of psychostimulants - clinically or by blood or urine analysis
Diagnosis of bipolar disorder is based on identification of the symptoms of mania or hypomania described above and a history of the disease. Symptoms must be severe enough to significantly impair social or occupational activities or require hospitalization to prevent harm to self or others.
Some patients with depressive symptoms may have previously experienced episodes of hypomania or mania, but they will not disclose this unless specifically asked. Skillful interviewing may reveal distressing signs (eg, excessive spending, impulsive sexual escapades, drug abuse), although such information is likely to be provided by relatives. A structured inventory such as the Mood Disorder Questionnaire may be helpful. All patients should be asked in a gentle but frank manner about suicidal tendencies, plans, or attempts.
Similar acute manic or hypomanic symptoms may occur as a result of stimulant abuse or medical disorders such as hyperthyroidism or pheochromocytoma. Patients with hyperthyroidism typically have other physical symptoms and signs, but thyroid hormone testing (T4 and TSH) is recommended as part of the initial diagnosis. Patients with pheochromocytoma suffer from severe hypertension; if not, then testing is not indicated. Other disorders are less likely to cause symptoms of mania, but depressive symptoms can occur in a number of disorders.
Taking a history of substance use (especially amphetamines and cocaine) and screening blood or urine for the presence of drugs can help determine a drug cause of the condition. However, because the episode could be caused by drug use in a patient with bipolar disorder, looking for the presence of symptoms (manic or depressive) not related to drug use is important.
Some patients suffering from schizoaffective disorder exhibit manic symptoms, but such patients may not return to normal between episodes.
People with bipolar disorder may also develop anxiety disorders (eg, social phobia, panic attacks, obsessive-compulsive disorder), which can make diagnosis difficult.