The word “tumor” evokes fear in most patients, even if it is called “benign.” In this case, things are much better than with a cancerous tumor, but we still have no right to relax.
Some benign tumors have the ability to degenerate into a malignant disease. At this time, the main thing is to detect and treat the formation before it changes its status and threatens a person’s life.
A polyp is also a benign tumor. This is the result of abnormal growth and proliferation of mucosal cells. Polyps appear in many organs. Sometimes it is completely harmless, sometimes it is a precancerous condition and requires strict monitoring. In this article we will talk about the most common polyps, the reasons for their development, the risk of degeneration and treatment methods.
Polyps in the intestines
The content of the article
The favorite place for polyps is the large intestine and rectum. Formations developing from the epithelial cells of these organs are called colorectal. These are the polyps that are most often found, so let's start with them.
Rectal polyp
According to statistics, 20-30% of adults have some kind of colorectal polyp. It is true that most of these tumors are harmless, but it is also possible for a colorectal polyp to cause bowel cancer.
Why and how the polyp develops is still unknown. For now we can only name the factors that contribute to this process. Also, doctors cannot say with certainty whether a person is completely insured against the development of polyps or, on the contrary, this is an inevitable disease. One way or another, it is known that a polyp is nothing more than the result of extracellular cell activity.
A normal cell grows and divides systematically. This is a natural process. Problems begin when genes mutate and cells begin to multiply out of control—new cells are not needed, but they can still form. Uncontrollably growing intestinal cells produce polyps. Polyps can occur in any area of the intestine, although they most often occur on the left side of the colon and rectum.
The essence of the problem
Polyp is a medical term adopted to designate a formation that rises above the surface of the mucous membrane of a hollow organ. Polyps can grow in the stomach, intestines, gall bladder, sinuses, bladder, and on the inner surface of the cervix and body of the uterus.
The term “polyp” implies a benign process, but the exact nature of a suspicious neoplasm can only be determined through histological examination of its cells.
The large intestine is a favorite location for such neoplasms. Preventative colonoscopy detects polyps in 3% of patients; 70% of neoplasms are localized in the rectum.
Men suffer from this pathology 2-3 times more often than women.
The risk of development depends on age (78% of patients have crossed the age line of 55 years).
Types of intestinal polyps
There are two types of polyps – non-tumor and neoplastic. The first type of polyps is not characterized by malignant degeneration, the second is dangerous. Neoplastic polyps are divided into adenomas and serrated polyps. Most intestinal polyps are adenomas. This polyp resembles a gland. It is often called an adenoma, and the cancer that develops from it is called adenocarcinoma. Adenocarcinoma is the most common type of colorectal cancer.
In general, the larger the polyp, the higher the risk of malignancy, especially in the case of tumor polyps.
Increases the risk of developing polyps themselves:
- Age over 50 years;
- Inflammatory bowel diseases (Crohn's disease, ulcerative colitis);
- Family history of polyposis;
- Smoking and excessive alcohol consumption;
- Obesity and low physical activity;
- African American descent;
- Poorly controlled type 2 diabetes.
Ulcerative colitis
There are human genetic mutations that cause the heredity of polyps. The presence of such a mutation also increases the risk of developing colorectal cancer.
Congenital pathologies that cause polyps are:
- Lynch syndrome
– a person with this condition develops a small number of polyps, although they tend to quickly become malignant. Lynch syndrome is the most common cause of congenital bowel cancer. It has also been linked to breast, stomach, small bowel, urinary tract and ovarian cancers. - Familial adenoma polyposis
is a rare disease that causes hundreds and sometimes thousands of polyps in the colon. The disease begins in adolescence. Against the background of acceptable polyposis, cancer develops in almost one hundred cases out of a hundred, and, as a rule, before 40 years of age. - Gardner's syndrome
- with this disease, polyps develop in the large and small intestines. The syndrome is characterized by the appearance of tumors on the skin, bones and other parts of the body. - MYH-associated polyposis
– This condition is similar to Gardner's syndrome. This time mutations in the so-called. MYH develops in genes. The patient is often diagnosed with multiple adenoma polyps and develops colon cancer at an early age. - Pacers-Egers syndrome
- the disease begins with the appearance of age spots throughout the body, including the lips, gums, feet, and then polyps appear throughout the intestines. - Dental polyposis syndrome
- during this time, multiple serrated polyps develop in the upper part of the colon.
Preparing for surgery
2-3 days before surgery, you should avoid coarse fiber, as well as foods that stimulate gas formation in the intestines. The ban includes black bread, products made from wholemeal flour, cabbage, legumes, fresh fruits and vegetables, milk and dairy products, juices, carbonated and alcoholic drinks.
1-2 days before surgery, care should be taken to “put off” bowel movements for several days. To do this, switch to a slag-free diet: • lean chicken and/or turkey; • cracker; • mashed potatoes; • vegetable soups; • boiled rice.
On the eve of the operation, dinner should be light and early; breakfast will have to be abandoned.
At this stage it will be necessary to cleanse the intestines. To ensure the success of the operation, the procedure is carried out twice – in the morning and in the evening.
You can use a regular medical enema (rinsing to clean water), but most patients prefer saline laxatives such as Fortrans (it should be used according to the instructions) or Microlax microenemas.
Symptoms of polyps in the intestines
Polyps rarely cause clinical symptoms. This is bad. Judge for yourself: an invisible harmless neoplasm turns into an invisible dangerous disease and appears when it is already too late. Even in the case of clinical manifestations, symptoms are nonspecific.
For example, a polyp is characterized by:
- Rectal bleeding
. Bleeding from the rectum is caused by many other diseases: hemorrhoids, anal fissures, rectal cancer. No one can tell with the naked eye what is behind the bleeding, but the symptom requires attention in any case. - Change in stool color
. Blood sometimes appears as red drops in the stool, sometimes it changes the color of the stool to crimson. Foods, medications, and dietary supplements can also change the color of your stool. So this sign is also non-specific, but worthy of attention. - Changes in bowel function
. The list of diseases that cause constipation or diarrhea is even more extensive. If bowel movements continue for more than a week, we may be dealing with a large polyp. Mucus discharge from the rectum is also a noticeable sign. - Pain
. Colon polyps also periodically manifest as pain. The formation partially compresses the intestines and causes cramping pain in the lower abdomen. It is clear that the polyp is not the only cause of this symptom. - Iron-deficiency anemia
. The list of causes of anemia is also quite extensive. Anemia is indicated by general weakness, fatigue, shortness of breath, and diarrhea. What is the connection between polyps and anemia? When a polyp causes bleeding, iron deficiency anemia is expected.
Rectal bleeding
Chronic bleeding leads to iron deficiency, which over time leads to a lack of red blood cells and hemoglobin, so in case of anemia, the patient should be examined for hidden bleeding, which in turn may indicate the presence of polyps.
Thus, abdominal pain, bloody stools, and changes in bowel movements indicate the need to see a doctor, however, as we have already said, these symptoms do not always appear, so you cannot count on them.
Recovery period
The duration of the recovery period depends on the method of surgical intervention and can range from 2 weeks to 2 months.
Postoperative dietary restrictions also vary widely.
If the operation was performed on an outpatient basis or you were in the hospital for a short time, we recommend that you carefully monitor your own health and immediately consult a doctor if suspicious symptoms appear: • increasing fever; • blood in stool; • persistent pain syndrome; • swelling of the extremities.
Even in cases where the injuries received during surgery are minimal, doctors recommend sticking to a slag-free diet 1 week
During the recovery period, you should avoid increased physical activity, thermal procedures, alcohol and drugs. Smokers are advised to reduce their nicotine intake to a minimum.
Diagnosis of intestinal polyps
The main means of diagnosing the underlying disease is screening. This is the gold standard for diagnosing the disease and the most effective strategy - screening allows us to detect a problem before it develops into a malignant disease. Screening can also detect cancer at an early stage, and starting treatment at this stage is much safer and more effective.
Since a colorectal polyp is considered a precancerous condition, special attention is paid to identifying this pathology during screening.
During screening, two tests are performed. The stool is first examined for occult bleeding. This method detects even small amounts of blood in the stool that is not visible during gastric emptying. However, a positive test result does not mean the presence of a polyp, especially cancer. This only indicates that there is hidden bleeding in the body. Colonoscopy helps determine its cause.
Colonoscopy is the most sensitive method for detecting polyps and cancer. During the examination, a thin tube with a camera is inserted into the back of the body. The doctor sees the intestinal mucosa with his own eyes. The examination also allows you to do a biopsy - take a sample of polyp tissue for histological examination. A wire loop is also placed over the colonoscope to remove polyps painlessly.
Colonoscopy
If the result of a stool test is within the normal range, a repeat test is prescribed after two years, but if prescribed by a doctor, it can be done earlier.
Polyps can be detected using a virtual colonoscope (CT colonography), a moving sigmoidoscope, and other methods, but you will still need a colonoscopy to biopsy or remove the polyp.
Reviews from patients and recommendations from doctors
We analyzed patient reviews of operations performed to remove polyps. There is practically no negativity. Surgical interventions are well tolerated, the postoperative period goes smoothly.
Some patients consider the “short-term” effect of the operation and the need to undergo annual preventive examinations as a disadvantage.
In most cases, recovery occurs without the need for further surgery. However, for example, adenomatous and villous polyps are today considered as precancerous conditions, and patients who have undergone surgery require constant medical supervision. In other cases, a repeated consultation with a proctologist once every 1-3 years is sufficient.
The likelihood of relapse and the time frame for re-application can only be determined by your attending physician after the initial rehabilitation period has passed.
Reviews of the work of doctors at City Clinical Hospital No. 31 can be read here.
Treatment of polyps - polypectomy
“No polyp – no risk” - this is the main principle of polyp treatment. Most polyps are not cancerous, however, unfortunately, no one can say for sure which polyp will turn into cancer and which will remain harmless, so the approach is simple: all polyps should be removed, and the sooner this happens, the better.
There are several ways to do a polypectomy:
- Removal with tweezers or a wire loop - in this case, polypectomy is performed during a colonoscopy. If the polyp is longer than one centimeter, fluid is injected under it. The formation rises high, which allows it to be isolated from surrounding tissues and facilitate its removal.
- Minimally invasive surgery – Polyps that are excessively large or that cannot be removed safely should be removed laparoscopically during a colonoscopy. This is a minimally invasive procedure.
- Complete proctocolectomy - in case of congenital pathologies, due to the large number of polyps, it is impossible to remove them one by one, so the doctor completely excises the large intestine and rectum.
Treatment and observation do not end with the removal of polyps, especially if the polyp is neoplastic and large. According to statistics, in thirty cases out of a hundred, tendon regeneration occurs, so observation after polypectomy is necessary.
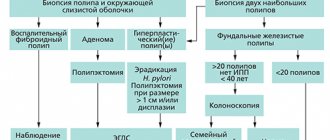
Colonoscopy is recommended after polyp resection:
- 5-10 years later if you only had one or two small polyps;
- After 3 years, if you had more than two or at least 1 cm of adenoma polyp;
- 3 years if you had more than ten adenomas;
- 6 months if you had a very large adenoma or an adenoma that needed to be removed piece by piece.
By the way, it is believed that aspirin and non-steroidal anti-inflammatory drugs reduce the risk of polyp recurrence, but they can only be taken with a doctor’s prescription and in no case arbitrarily.
Therapy methods
Drug treatment for polyps is not effective. Neoplasms are removed exclusively surgically. There are several options for radical treatment. The choice of method depends on the final diagnosis, general condition and location of the tumors. A prerequisite is that the cell body of the neoplasm is sent for research in order to establish its nature.
The decision on the need for surgical removal of tumors is made by the treating specialist. It is worth understanding that only juvenile polyps disappear on their own - all others tend to grow or degenerate.
In some cases, the doctor can simply observe the dynamics of growth development, recommending a special diet to the patient. If there is no proliferation of tumor cells, then the operation can be postponed indefinitely.
The most popular methods for removing intestinal polyps are gastroscopy or colotomy. If pathology of all parts of the intestine is diagnosed or the neoplasm is large, abdominal surgery would be advisable.
Is prevention possible?
The basis for the prevention of colon cancer and polyps is screening, although there is evidence of the preventive effect of other factors. For example, some studies show that calcium intake prevents the recurrence of colon adenomas (unfortunately, it is still unknown whether calcium has a protective effect against colon cancer), while other studies show that vitamin D helps prevent the development of colorectal cancer .
This issue is still under study, but there are already proven and tested recommendations: the risk of developing dangerous intestinal diseases will be significantly reduced if you develop healthy habits - include more fruits, vegetables, grains in your diet, reduce fat, avoid. Physically, you need to maintain a healthy weight.
ONLINE REGISTRATION at the DIANA clinic
You can sign up by calling the toll-free phone number 8-800-707-15-60 or filling out the contact form. In this case, we will contact you ourselves.
If you find an error, please select a piece of text and press Ctrl+Enter
Risk factors
Risk factors and mechanisms of colon polyps are being actively studied. Among the environmental factors, the nature of nutrition is significant, with a predominance of refined foods in the diet, which contribute to constipation and prolonged stasis of intestinal contents. Dysbacteriosis of the colon has some influence on the occurrence of polyps, reflecting a violation of local and decreased general immunity, contributing to changes in the differentiation and regeneration of mucosal cells. The role of concomitant diseases of the biliary system and impaired production of bile acids, which have a mutagenic effect on the mucous membrane, is also noted as a risk factor. Active chronic inflammation and mucosal dysplasia play a certain role in the occurrence of polyps.