Helicobacter bacterium: symptoms and causes
Abdominal pain, nausea, belching of air - all this may indicate that a dangerous, harmful Helicobacter bacterium has settled in the body, the treatment of which must be serious and thorough.
Helicobacter pylori is a very dangerous pathogenic microorganism that can lead to gastric and duodenal ulcers, gastritis and other diseases dangerous to the digestive system. Helicobacter was first discovered only 30 years ago. Medical research conducted since that time has proven that gastritis can have an infectious etiology. Also, according to studies of this bacterium, scientists have proven that, according to statistics, 75% of cases of stomach cancer in developed countries are caused by Helicobacter. In developing countries, this figure is even more frightening: 90% of patients with stomach cancer contracted the disease due to Helicobacter pylori.
Thus, it is worth pointing out the special role of early diagnosis of gastritis and gastric ulcers. It is a timely visit to a doctor that can save health and life.
Basis and superstructure of Helicobacter pylori eradication therapy regimens
Yuri Pavlovich Uspensky , professor, doctor of medical sciences:
– Dear colleagues, the next part of our gastroenterology section is devoted to the problem of human helicobacteriosis. And I would be happy to give the floor to the deeply respected Tatyana Lvovna Lapina with such a philosophical report: “The basis and superstructure of Helicobacter pylori eradication therapy regimens.”
Tatyana Lvovna Lapina , associate professor, candidate of medical sciences:
– Thank you very much, Yuri Pavlovich. So, dear colleagues, these terms are indeed taken from the old philosophy: “The basis and superstructure of Helicobacter pyloric eradication therapy regimens.” If we talk about the variety of schemes that have ever been used and described in the literature in order to eradicate Helicobacter pyloric, then this variety of schemes is impossible to describe. This is such an abundance of different medications, a variety of combinations, a variety of durations, an attempt to give two-stage regimens, and so on. But if we look at modern standard schemes, then by and large they are known by comparison. These are the schemes that are presented in the IV Maastricht Consensus. First of all, this is standard triple therapy with clarithromycin (proton pump inhibitor + clarithromycin + amoxicillin). Then, of course, we need to talk about quadruple therapy with a bismuth drug (proton pump inhibitor + bismuth drug + tetracycline + metronidazole). As a backup regimen, triple therapy with levofloxacin (proton pump inhibitor + levofloxacin + amoxicillin). And the options for using widely known antimicrobial agents to destroy Helicobacter pylorus are clarithromycin + amoxicillin + metronidazole as part of sequential and so-called quadruple therapy without bismuth, that is, a combined Helicobacter pyloric eradication scheme.
The Russian Gastroenterological Association, in its recommendations for the diagnosis and treatment of Helicobacter pyloric infection, tried to very clearly outline for practicing physicians the procedure for applying these treatment regimens. As the first line, we can choose standard triple therapy or quadruple therapy. If first-line therapy fails, we can turn to quadruple therapy with bismuth. And if this treatment regimen fails, we can turn to a backup antibiotic as part of triple therapy with Levofloxacin.
So, it seems that we are treating a microbial agent. Perhaps the most important thing in the eradication therapy scheme, the basis, is antibacterial drugs. You know, I would still say that the main thing in the eradication therapy regimen, the basis, is proton pump inhibitors. Please note that when listing all regimens, drugs from the group of proton pump inhibitors are given first place. Why are proton pump inhibitors so important for eradication therapy? The thing is that we can very well predict the effectiveness of proton pump inhibitors. If we turn to this classical scheme of the necessary maintenance of the level of intragastric pH for the treatment of acid-dependent diseases, then here we see the resulting pH >3 for the successful healing of a duodenal ulcer. Let me remind you that this is a classic work - Borget's meta-analysis. (00:04:24) We see a threshold value here - it is necessary to maintain pH>4 enterogastrically for a long enough period of time, during the day, in order to successfully heal erosions in erosive esophagitis. This is Bell's work - also a classic meta-analysis. But the most interesting thing is that we are most interested in today, why, in fact, we are talking about proton pump inhibitors as the basis in eradication therapy regimens - this is maintaining enterogastric pH>5. In order for the eradication of Helicobacter pyloric to be successful, the most stringent values for maintaining enterogastric pH have been established for the action of acid-suppressive drugs. Why?
Let's return to the classic ideas about Helicobacter pylori. Any bacterium produces ATP using the so-called proton motive force, that is, an electrochemical gradient of hydrogen ions. Here the redux pump (in the diagram it is a redox pump) creates a negative charge of the electrochemical gradient inside the cell, which, in fact, is used for the formation of ATP (ATP). Thus, the bacterial cell functions normally. It is calculated that if Helicobacter pylori is in an environment with a pH of 7, then the internal environment of the bacterium has a pH of 8 and 4. That is, the pH gradient is 1.4 and in electrical terms it is equal to 90 millivolts. This is a very convenient good condition for Helicobacter pylori, its normal life activity. But we understand that Helicobacter lives in the acidic environment of the stomach. How acidic it is under the layer of mucus on the surface of epithelial cells, of course, is difficult to say, but if the pH in the stomach is somewhere on the order of, for example, 2, then perhaps in the wall layer of mucus the pH is about 4.
What allows Helicobacter to actively survive? Urease enzyme, which decomposes urea to form ammonium ions. Ammonium ions essentially protect this very electrochemical gradient of hydrogen ions. A completely different situation arises when we prescribe proton pump inhibitors to the patient, and we artificially bring the enterogastric pH to the desired values in order for us to successfully scar a duodenal ulcer, heal erosions in gastroesophageal reflux disease, or eradicate Helicobacter pyloric. The thing is that Helicobacter pyloricus does not withstand alkalization of external environmental conditions. And, in general, any practicing doctor knows this very well, because he understands that if he prescribes even two very good antibiotics, eradication most likely will not work.
Let me introduce you to a very old classic study. We see two groups of columns here. The first columns show us the percentage of eradication when prescribing our favorite antibiotics, Amoxicillin and Clarithromycin, but only the yellow column without proton pump inhibitors. Please look - in fact, no eradication occurs. But if we give three drugs based on proton pump inhibitors, then the difference in eradication percentage is simply colossal.
The same applies to other options for standard triple therapy: Clarithromycin, Metronidazole. We see that if we give the patient only Clarithromycin with Metronidazole without a proton pump inhibitor, then there is a very large increase in effective eradication that the proton pump inhibitor gives us. And, naturally, if we prescribe motor therapy with a proton pump inhibitor, then Helicobacter pyloricus tries to somehow maintain its standard good vital activity. For example, it mainly existed in the antrum, where it was relatively acidic and practically not very alkaline. And when we prescribe proton pump inhibitors, Helicobacter pyloric translocation occurs into the body of the stomach. Where the stomach glands are located, where the environment will be more acidic and, against the background of proton pump inhibitors, approaches more desirable pH conditions. In order to prevent an increase in the foothold of chronic gastritis, as one of the provisions of the IV Maastricht consensus, eradication therapy is recommended for those patients who are planning long-term treatment with proton pump inhibitors. For what? In order to cure gastritis, so that they do not have Helicobacter pyloric, in order to prevent changes in Helicobacter pyloric translocations on the surface of the stomach.
So, proton pump inhibitors are really the mainstay of eradication therapy regimens, and the better they work, the better they can maintain enterogastric pH >5. Why? Because it is under such conditions that Helicobacter pylorus becomes especially sensitive to the action of those antibiotics that form the superstructure of the eradication therapy regimen. Today we will mainly use the drug “Rabeprazole” as an example of the basis of the eradication therapy regimen. I am pleased to draw your attention to the bioequivalence graph of Rabeprazole produced by KRKA to the original drug.
So, what is the basis for prescribing an eradication therapy regimen? Of course, the ability of proton pump inhibitors to maintain enterogastric pH within a given range for a given period of time. And if we look at a recent meta-analysis, then indeed the latest generation proton pump inhibitors, including Rabeprazole, in terms of the percentage of average time pH>4 when taking a standard dose during a course, show, of course, very, very good results.
Let's return to eradication therapy regimens. The standard triple regimen of eradication therapy was adopted as the first-line treatment regimen: proton pump inhibitor (PPI) at a standard dose twice a day, Clarithromycin (CLA) 500 milligrams twice daily, Amoxicillin (AMO) 1000 milligrams twice daily per day.
It is possible to choose quadruple therapy with a bismuth drug in certain clinical situations. For example, it is very important for us to provide a regimen with the highest possible efficiency, for example, in the case of gastric MALT lymphoma, when we plan eradication of Helicobacter pyloricus in order to achieve histological remission of the tumor. This, of course, is a combination of a proton pump inhibitor at a standard dose twice a day, Bismuth Tripotassium Dicitrate (BTD) 120 milligrams four times a day, Tetracycline (TET) and Metronidazole (MET).
As a regimen that gastroenterologists can prescribe in controversial, complex cases, the Russian Gastroenterological Association recommends the use of a regimen with Levofloxacin. I repeat once again, of course, this is not an appointment from a primary care doctor, it is still an appointment that should be made by a gastroenterologist. Is there data on sequential therapy in Russia? Unfortunately, there is not a lot of data, although there are isolated works that indicate that this scheme can be applied. Again, this sequential therapy is quite complex, which consists of two stages of prescribing drugs for the eradication of Helicobacter pyloricus, and is more likely to be included in the arsenal of a gastroenterologist than a primary care physician. Let's see how standard triple therapy based on Rabeprazole works. Please look, the dose of Rabeprazole here is quite small, 10 milligrams twice a day. And, despite the fact that this is an Asian population, in which it is always difficult to achieve successful eradication of Helicobacter pyloricus, in real clinical practice the eradication percentage exceeds 80.
Can the effectiveness of standard triple therapy be increased? It is possible, and working both with the basis of the circuit and with the superstructure of the circuit. For example, we can add bismuth to standard triple therapy. I think this is a very good addition to the circuit superstructure. We can increase the dose of the proton pump inhibitor, and this additional anti-acid effect will increase the eradication of Helicobacter pyloric infection. We can increase the duration of the standard triple therapy. It is difficult, of course, to say that any of us will receive such a remarkable increase in eradication percentage, depending on whether we prescribe standard triple therapy for 7, 10 or 14 days. But still, the current trend, of course, suggests that the longer we carry out eradication therapy within the designated time frame, the higher the percentage of eradication.
And, of course, I would like to draw attention once again to the basic drugs in eradication therapy regimens. Please look at 35 studies, almost 6 thousand patients. A meta-analysis that examined whether the newer proton pump inhibitors, Rabeprazole and Esomeprazole, are superior to the older, more classical proton pump inhibitors. And, you see, here the number of patients who need to be treated is 23. Indeed, there is evidence that regimens based on Rabeprazole are more effective. What do I want to show? I would like to show this meta-analysis in terms of different dosages of proton pump inhibitors. Please look: here 10 milligrams twice a day of Rabeprazole was used. But the same meta-analysis – 20 milligrams twice a day. And we see that thanks to the powerful, acid-suppressing effect of Rabeprazole, even a dose of 10 milligrams twice a day works perfectly for the eradication of Helicobacter pyloricus.
I must say that when I saw this terracotta bas-relief from the Roman era - you see Hercules with a club, he deals with the Lernaean hydra - it immediately seemed to me that the Lernaean hydra reminded me a lot of someone. It seems to me that the analogy with Helicobacter pyloricus is evident here. And it is very pleasant to say at the end of my lecture that we really have a weapon to defeat Helicobacter pyloric hydra - these are eradication therapy regimens for Helicobacter pyloric infection. We just need to strictly adhere to the standards for managing patients with Helicobacter pyloric infection.
What is the Helicobacter bacterium?
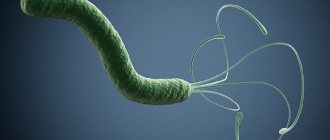
Helicobacter is a special type of pathogenic microorganism. It is a dangerous bacterium that infects the duodenum and stomach of humans. The microorganism itself is a parasite that produces toxic substances that damage the mucous membranes of organs. It is damage to the mucous membrane that leads to peptic ulcers, gastritis and other dangerous ailments.
It has long been believed that no organism is able to survive in the acidic environment of the stomach. But this does not apply to Helicobacter. The bacterium, on the contrary, thrives in an acidic environment, which is preferable for it to any other habitat. Helicobacter pylori has a spiral shape and flagella. This structure of the microorganism allows it to move through the mucous membranes of internal organs and cause irreparable harm to their integrity.
Helicobacter can adapt to almost any habitat. This is explained by the fact that this organism practically does not require oxygen. And another distinctive feature of Helicobacter pylori is its ability to change its own shape and become oval or round.
Russian scientists have come to the decision to introduce a special term - helicobacteriosis. It denotes all the processes that begin to occur in the body immediately after the introduction of this pathogenic microorganism into it. But Western scientists conducted studies of patients’ charts and came to the conclusion that about 60-65% of the population of the entire Earth are susceptible to infection. Thus, Helicobacter is the most common infectious disease of humanity after herpes, which is a viral disease.
Metronidazole
H. pylori is generally very sensitive to metronidazole, the effectiveness of which is independent of pH. After oral or infusion use, high concentrations of the drug are achieved in the gastric juice, which makes it possible to achieve the maximum therapeutic effect. Metronidazole is a prodrug that undergoes activation by bacterial nitroreductase during metabolism. Metronidazole causes H. pylori to lose its helical DNA structure, causing DNA damage and killing the bacterium.
NB!
The result of treatment is considered positive if the results of the test for H. pylori, carried out no earlier than 4 weeks after the course of treatment, are negative. Performing the test before 4 weeks after eradication therapy significantly increases the risk of false negative results. It is preferable to stop taking PPIs two weeks before diagnosis. Helicobacter pylori eradication therapy: scheme
What happens in the body
As soon as Helicobacter enters the human body, it immediately descends into the stomach, where it lives for the rest of the time. In order not to die from gastric juice, the composition of which is quite aggressive, Helicobacter secretes special enzymes that surround it with a shell and neutralize the acid. The spiral-shaped antennae that Helicobacter has allow it to drill through the mucous layer and get to the cells of the parietal tissues, which are usually hidden from acid.
It is the parietal cells of tissues that become the main food for Helicobacter. The pathogenic microorganism eats them and poisons the environment with the products of its vital activity. At the same time, those blood cells that react to Helicobacter and strive to destroy them (neutrophils) wake up in the body. However, by destroying the pathogenic microorganism, neutrophils also destroy mucosal cells that have already been touched by Helicobacter.
After the layer of the mucous membrane is damaged, hydrochloric acid begins to actively affect the tissue. This is how the inflammatory process develops and an ulcer occurs. The localization of ulcers is most often similar. This is explained by the fact that Helicobacter itself is very fond of two parts of the stomach - the bulb and the pylorus.
Proton pump inhibitors (PPIs)
PPI therapy has proven effective in various clinical studies. Although PPIs have a direct antibacterial effect on H. pylori in vitro, they do not play an important role in eradicating the infection.
The mechanism by which PPIs synergize when combined with antimicrobials to enhance the clinical efficacy of eradication therapy has not been fully established. It is assumed that antisecretory drugs of the PPI group may help increase the concentration of antimicrobial agents, in particular metronidazole and clarithromycin, in the gastric lumen. PPIs reduce the volume of gastric juice, as a result of which the leaching of antibiotics from the surface of the mucosa decreases, and the concentration, accordingly, increases. In addition, reducing the volume of hydrochloric acid maintains the stability of antimicrobials.
Causes of Helicobacter pylori infection
Helicobacter bacteria cannot exist in air; with active air intake, these pathogenic organisms die. They are transmitted mainly through human mucus and saliva. Thus, most often infection occurs in the following ways:
- Sharing utensils;
- Using only personal hygiene products;
- Kisses;
- From mother to child.
Thus, friends, family and cohabitants of the patient may be at risk.
In general, infection is facilitated by a low standard of living and neglect of hygiene rules. Very often, helicobacteriosis occurs in people living in communal apartments and dormitories, orphanages, as well as in medical workers. It is worth noting that in third world countries the disease occurs much more often than in developed countries. In Russia, in recent years, the incidence of gastritis and ulcers due to the influence of Helicobacter has begun to be noted among people from wealthy segments of the population.
You can protect yourself, and it is better to take care of prevention in advance than to suffer from an illness and look for ways to fight Helicobacter urgently.
results
- In the intention-to-treat analysis, hybrid therapy was associated with an eradication rate of 96.5, bismuth quadruple therapy with 93.5% effectiveness, and high-dose dual therapy with 86% eradication success. Significant differences were obtained with high-dose therapy (P < 0.001).
- Similar efficacy was observed in the per-protocol assay.
- According to the safety analysis, the incidence of side effects was lowest with dual high-dose therapy (13%). While the frequency of adverse events was 25.5% against the background of hybrid therapy and 34% against the background of quadruple therapy with bismuth.
Antibiotic resistance analysis
- Resistance rates were highest for metronidazole: 28% with quadruple therapy and 34% with hybrid therapy and 37%.
- Resistance to clarithromycin was 23% in individuals receiving quadruple therapy, 16% in individuals receiving hybrid therapy.
- Resistance to amoxicillin and metronidazole was rare and ranged from 0-3%.
- It is noteworthy that in patients receiving quadruple therapy, resistance to metronidazole was associated with failure of eradication.
Source:
Andrew D. Bowser. H. pylori: High Eradication, Fewer Side Events With Hybrid Therapy. Medscape. May 28, 2021.