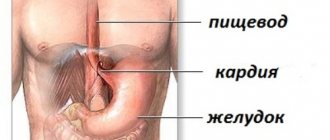
Reflux esophagitis is a chronic disease associated with inflammation of the esophageal mucosa due to the reflux of gastric contents into the esophagus (reflux). Reflux esophagitis is a manifestation of gastroesophageal reflux disease, which in turn most often develops against the background of a hiatal hernia.
Reflux esophagitis is perhaps the most common disease of the gastrointestinal tract. According to various studies, about 50% of the adult population of developed countries experience symptoms of reflux at one time or another, but only 9.5% are diagnosed. This is due to the fact that in mild cases people do not seek medical help.
Complaints with reflux esophagitis
The most common complaint with reflux esophagitis is heartburn. Most often it is perceived as a burning sensation in the chest, sometimes a sour taste in the mouth, and sometimes takes a debilitating form, significantly reducing the quality of life. It occurs when overeating, or eating certain foods, and is often worse when lying down or bending over. Heartburn can also occur on an empty stomach or during prolonged fasting. Heartburn worsens when lying down; in severe cases, it forces patients to sleep in a sitting position.
The second most common symptom of reflux esophagitis is chest pain. The pain is associated with inflammation in the wall of the esophagus. The pain intensifies while eating; patients literally feel the passage of a bolus of food through the esophagus. Analgesics do not relieve pain. Antacids and sometimes drinking cold water provide relief.
Also often with esophagitis, belching occurs, which is associated with a concomitant hiatal hernia.
Often, reflux esophagitis is accompanied by complaints characteristic of other diseases, the so-called extraesophageal manifestations of reflux esophagitis. A dry cough that gets worse after eating or lying down is common. When examining such patients, lung diseases are not detected, but sometimes chronic bronchitis or bronchial asthma are detected, which significantly complicates the diagnosis of reflux esophagitis.
Another common extra-esophageal manifestation of esophagitis is hoarseness and frequent pharyngitis, which are difficult to treat until medications are used to treat esophagitis. Also, with reflux esophagitis, heart rate arrhythmias and tooth decay are not uncommon.
Presentation of symptoms and signs
Reflux esophagitis manifests symptoms and signs with varying degrees of severity, which depends on the stage of the disease:
- heartburn (the most common manifestation);
- pain in the chest near the heart;
- lump in throat and difficulty swallowing;
- frequent cough and inflammation of the respiratory tract;
- weight loss;
- hoarse voice;
- poor sleep;
- nausea and belching;
- bloating;
- vomit.
Are you experiencing symptoms of reflux esophagitis?
Only a doctor can accurately diagnose the disease. Don't delay your consultation - call
Diagnosis of reflux esophagitis
Diagnosis of reflux esophagitis most often does not cause difficulties. For an experienced gastroenterologist, it is often enough to collect complaints and a medical history to suspect a diagnosis of reflux esophagitis.
The most important and informative diagnostic method is gastroscopy (FGDS) .
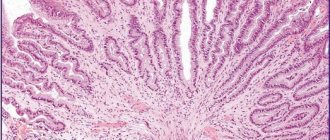
Reflux esophagitis, endoscopic picture
When examining the esophagus, inflammation in its mucous layer, erosion, and ulcers are revealed. According to gastroscopy, the degree of the disease is determined. Sometimes so-called endoscopically negative reflux esophagitis occurs, in which case the wall of the esophagus appears unchanged, although there are complaints.
X-ray of the esophagus with barium - used to diagnose a possible concomitant hiatal hernia; also during this study, it is possible to document the fact of reflux of gastric contents into the esophagus, its severity, and duration. The speed of passage of contrast through the esophagus is also assessed, which makes it possible to judge motility disorders and indirectly judge the presence of inflammation in its walls.
In difficult cases, daily pH measurements or daily impedance measurements are performed to clarify the diagnosis. These studies make it possible to measure acidity in the lumen of the esophagus and identify reflux of gastric contents, determine its nature and the time of contact of aggressive contents with the esophageal mucosa, this is of great importance for developing treatment tactics.
Sometimes, after several years of illness, heartburn either goes away completely or decreases significantly, without treatment, and this is a bad sign, most often indicating the development of complications.
Information about the disease
According to epidemiological studies, about 23.6% of the adult population suffers from gastroesophageal reflux disease in Moscow. The peculiarity is the chronic and recurrent nature of the disease. The reflux of gastric contents into the lower parts of the esophagus occurs spontaneously. At the point of contact with the mucous membrane, an inflammatory process develops, which becomes the cause of discomfort and poor health. In medical practice, the full name of the disease is gastroesophageal reflux disease (GERD).
Classification of reflux esophagitis
The two most widespread classifications of esophagitis in the world are the Savary-Miller classification, adopted in 1977 and modified in 1997 at the 6th European Gastroenterological Conference, and the Los Angeles classification, also adopted in 1997. It is considered more complete and therefore more often used.
Savary-Miller classification
1st degree - one or more erosions occupying less than 10% of the circumference of the esophagus 2nd degree - merging erosions occupying more than 10, but less than 50% of the circumference of the esophagus 3rd degree - multiple erosions occupying the entire circumference of the lower third of the esophagus 4th degree - complications of reflux esophagitis: esophageal ulcer, stricture, Barrett's esophagus
Los Angeles classification of esophagitis
Grade A - damage to the wall no more than 5 cm long, within one fold of the mucosa Grade B - damage more than 5 cm long, but within one fold Grade C - damage more than 5 cm long, occupying up to 75% of the circumference of the esophagus Grade D - damage to the mucosa occupying 75% or more of the circumference of the esophagus
Our services
The administration of CELT JSC regularly updates the price list posted on the clinic’s website. However, in order to avoid possible misunderstandings, we ask you to clarify the cost of services by phone: +7
| Service name | Price in rubles |
| Gastroscopy (videoesophagogastroduodenoscopy) | 6 000 |
| Colonoscopy (video colonoscopy) | 7 000 |
| Ultrasound of the abdominal organs (liver, gall bladder, pancreas, spleen) | 3 800 |
| Fluoroscopy and radiography of the stomach | 4 800 |
All services
Make an appointment through the application or by calling +7 +7 We work every day:
- Monday—Friday: 8.00—20.00
- Saturday: 8.00–18.00
- Sunday is a day off
The nearest metro and MCC stations to the clinic:
- Highway of Enthusiasts or Perovo
- Partisan
- Enthusiast Highway
Driving directions
Complications of reflux esophagitis
With inadequate therapy, or its insufficient effectiveness, or in the absence of treatment, reflux esophagitis continuously progresses and can lead to quite serious complications. The most common complication is the development of Barrett's esophagus, in simple terms, this is a situation when the structure of the cells of the esophageal mucosa, under the influence of constant inflammation, begins to change its structure. This process is called dysplasia. Barrett's esophagus is considered a precancerous disease, as it significantly increases the risk of developing esophageal adenocarcinoma (cancer).
Also a frequent complication is the development of severe erosive ulcerative lesions of the esophageal mucosa, which in turn are complicated by either bleeding or stricture (narrowing) of the esophagus. Bleeding can be either chronic, invisible to the patient, or acute, quite profuse and life-threatening. With chronic bleeding from erosions and ulcers of the esophagus, the patient feels unmotivated weakness and, when taking a blood test, anemia is detected.
Stricture of the esophagus (narrowing of the lumen), as mentioned above, develops against the background of erosive esophagitis, or ulcerative lesions of the esophageal mucosa, in the absence of adequate treatment. Signs of a narrowing of the esophagus include difficulty swallowing and vomiting of food that has just been eaten. Esophageal stricture requires immediate treatment
How to diagnose
In gastroenterology, a number of objective diagnostic methods are used to determine the patient’s condition and the extent of damage to the esophagus. Esophagitis manifests symptoms to a pronounced degree, which is a reason to consult a doctor. Diagnosis and treatment are carried out by a gastroenterologist. The patient examination consists of:
- collecting anamnesis about health, presence of diseases;
- contrast x-ray (with barium);
- endoscopic gastroscopy;
- pH-metry and manometry;
- laboratory tests of gastric juice.
Treatment of reflux esophagitis
Treatment of esophagitis is carried out both conservatively and surgically. Of course, the overwhelming majority of patients are treated conservatively by a gastroenterologist. The goal of treatment is to remove symptoms, prevent the development of complications, and improve quality of life. You need to understand that it is often impossible to cure reflux esophagitis with conservative methods once and for all, and either constant or periodic maintenance therapy is required. The only way to radically get rid of esophagitis is through surgery.
Lifestyle change
The first thing a competent gastroenterologist will recommend when treating reflux esophagitis is optimizing the patient’s lifestyle, and it must be said that this is the most difficult thing in treating this disease. If you are overweight, you should lose weight. Patients are recommended to eat frequent meals, at least five times. Last meal 4 hours before bedtime. It is recommended to sleep with the head end raised, and you should not put pillows on it, but raise the head end of the bed. Alcoholic drinks, coffee, tea, and sour foods are prohibited. Limiting physical activity associated with heavy lifting and working in an inclined position.
So let's summarize what you need to change in your life:
- after eating, avoid bending forward and not lying down;
- sleep with your head elevated;
- do not wear tight clothes and tight belts;
- avoid large meals;
- do not eat at night;
- limit the consumption of foods that cause a decrease in LES pressure and have an irritating effect (fats, alcohol, coffee, chocolate, citrus fruits);
- stop smoking;
- normalize body weight, if it is excess;
- Avoid taking medications that cause reflux (anticholinergics, sedatives and tranquilizers, calcium channel inhibitors, beta blockers, theophylline, prostaglandins, nitrates).
Methods of treating the disease
In case of esophagitis, treatment is prescribed taking into account the patient’s condition and pathogenesis. The most important condition is a change in lifestyle and a systematic reduction in the amount of acid entering the esophagus. The treatment system includes:
- taking medications to reduce stomach acidity;
- antibacterial therapy in the presence of infection;
- diet therapy on an ongoing basis;
- surgical intervention for complicated forms of the disease.
Conservative therapy
For conservative therapy, the following groups of drugs are used:
- antacids and alginates
- proton pump inhibitors
- prokinetics
Antacids and alginates
Antacids and alginates, topical preparations most often containing aluminum and magnesium salts, these drugs act locally, are not absorbed into the blood and do not have a systemic effect. Their advantage is safety of use, but there is also a disadvantage, a short duration of action. Antacids are not used as an independent method of treatment, but are used as first aid for heartburn, and as an intensification of therapy for the speedy healing of erosions and ulcers of the esophagus. Preparations in the form of gels with alginic acid have proven themselves to be the best, which, when interacting with acid in the lumen of the stomach, form foam, thereby increasing the duration of action of the drug and its effectiveness. Antacids are most often prescribed 40 minutes after meals and at night, or on demand in case of heartburn.
Proton pump inhibitors (PPIs)
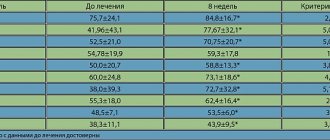
Today they are the main drugs in the treatment of reflux esophagitis, these include the well-known omeprazole, lansoprazole, rabeprazole, etc. These are systemic drugs, they block the transport of hydrogen molecules into the parietal cells of the stomach, responsible for the secretion of hydrochloric acid, and how do we We remember from the school chemistry course, this acid consists of a molecule of hydrogen and chlorine, no hydrogen, no acid. These drugs have revolutionized the treatment of reflux esophagitis, significantly improving the outcome and reducing the number of complications. Previously, H2 histamine receptor blockers were used, which were much less effective and had more side effects. It must be said that these drugs are sometimes used now in combination with PPIs to enhance the effect. The main disadvantage of proton pump inhibitors (PPIs) is their fairly rapid removal from the blood, which requires repeated use throughout the day, and even with double use, so-called acid breakthroughs are described, when, more often at night, the acidity of gastric juice sharply increases. Most often, PPIs are prescribed 20 mg twice a day 20 minutes before meals, morning and evening for 6 to 8 weeks. Then maintenance therapy is prescribed at 10 mg per day or 10 mg twice a day.
Prokinetics
Prokinetics are drugs that improve and normalize peristalsis of the gastrointestinal organs, including the esophagus. The most commonly prescribed drug is itopride, which is considered the most effective and safe drug. Motilium is also prescribed. The previously popular cerucal has recently been deprecated due to its central effect on the brain. Prokinetics are prescribed 1 tablet three times a day 20 minutes before meals. A course of 2 weeks is recommended.
Problems of conservative therapy
The vast majority of patients with reflux esophagitis are treated conservatively, achieving good functional results, but unfortunately, therapy is not always effective. As we wrote above. The cause of reflux esophagitis is the reflux of gastric contents into the esophagus. So the first problem with conservative therapy is that it does not eliminate the cause, but only relieves the symptoms. With conservative therapy, reflux remains, but is no longer acidic, and therefore patients do not feel any complaints. Although some researchers believe that due to the neutralization of acid, bile begins to flow into the esophagus, since it ceases to be inactivated in the stomach, and bile is an even more aggressive environment for the development of complications of esophagitis. Although it should be noted that this is still a theory that has not received sufficient confirmation. But at the same time, a number of scientists associate the growth of esophageal cancer with this hypothesis. Since, despite the widespread use of PPI drugs, the incidence of esophageal cancer is steadily increasing.
Taking medications in itself can cause complications. Evidence has been obtained that proton pump inhibitors increase the risk of stroke, osteoporosis and heart attack, and although the risk is not quite high, about 0.4 - 0.6% per year, it is still there.
Well, perhaps the main thing is that the effect of conservative therapy is temporary and is not always sufficiently effective. So, 6 months after stopping therapy, complaints return in 40-50% of patients, and after 12 months in 80-90%, that is, most patients are forced to take medications daily for many years. Considering the sufficient safety of the drugs, this may not be scary, although it certainly reduces the quality of life. But the problem lies in the fact that with long-term therapy, after three or five years, the effectiveness of the drugs decreases and in 20 - 30% of patients complaints reappear and complications of esophagitis develop, despite the constant use of the prescribed drugs.
Answers to frequently asked questions
How to treat esophagitis?
Esophagitis is treated depending on the degree of manifestation of the disease and the inflammatory process in the esophagus. In acute cases, medications are prescribed and it is recommended to adhere to the principles of dietary nutrition. In complex cases and in advanced stages of reflux esophagitis, surgical intervention may be prescribed.
What kind of disease is esophagitis?
Reflux esophagitis is a non-infectious disease with an inflammatory process in the esophagus due to uncontrolled reflux of gastric contents. GERD is one of the common diseases in gastroenterology.
How to treat reflux esophagitis?
In 90% of patients, the prognosis for recovery is positive. Treatment is prescribed by a doctor after diagnosis and laboratory tests. In most cases, drug treatment is required. Drugs are prescribed that help reduce the acidity of gastric juice and eliminate the symptoms of the disease.
Algorithm for diagnosis and treatment of gastroesophageal reflux disease
P
Gastroesophageal reflux disease (GERD) refers to a certain set of clinical symptoms (heartburn, pain) resulting from pathological reflux of stomach contents into the esophagus, which may or may not be accompanied by morphological changes in the esophageal mucosa. In the first case they talk about “endoscopically negative GERD”, in the second - about “endoscopically positive GERD”, or reflux esophagitis.
The relevance of the problem of GERD is determined by a number of circumstances. First, epidemiological studies
recent years have shown that, in terms of frequency and prevalence, GERD takes a leading position among other gastroenterological diseases. Heartburn, the leading symptom of GERD, is detected in 20-40% of the population of developed countries and in the USA, for example, it affects 25 million people [1, 2].
Secondly, the great clinical significance
of this disease. As evidenced by specially conducted studies, patients with GERD themselves rate their quality of life lower than patients with coronary heart disease [3]. Currently, the closest attention is paid to the “extraesophageal” symptoms of GERD, in particular, its cardiac variant. It was noted that in 50% of cases the cause of pain in the left half of the chest, not associated with heart damage (non-cardiac chest pain), is GERD. The entry of refluxate into the lumen of the bronchi can provoke the occurrence of bronchospasm [4].
Serious complications can develop in patients with GERD and from the esophagus itself. Thus, in 2% of patients with the erosive form of GERD, esophageal bleeding occurs, in 8-20% of patients peptic strictures of the esophagus are formed, and in 10% of patients replacement (metaplasia) of the stratified squamous epithelium of the esophagus occurs with columnar gastric or intestinal epithelium (Barrett's esophagus), increasing the risk development of esophageal adenocarcinoma by 30-125 times [5]. The noticeable increase in the prevalence of GERD among the population explains why in the structure of esophageal cancer there was a significant decrease in the proportion of squamous cell carcinoma and an increase (from 8% to 50%) in the proportion of adenocarcinoma.
Finally, certain difficulties arise in the treatment
patients with GERD. If the average time for scarring of duodenal ulcers is 3-4 weeks, for gastric ulcers - 4-6 weeks, then the healing time for esophageal erosions in many patients can reach 8-12 weeks. At the same time, cessation of medication is accompanied in 60-70% of patients by the rapid (within the first 3 months) development of relapse of the disease [6].
Thus, the three aspects discussed above (epidemiological, clinical and therapeutic) currently make GERD one of the main problems in gastroenterology.
Nowadays, the classification of GERD has become significantly simplified and has become more practical. classification
of GERD
is now used, distinguishing non-erosive (NERD), erosive (ERD) forms of gastroesophageal reflux disease and Barrett's esophagus [7 ]. NERD is the most common form of GERD (occurs in 60% of patients), characterized by a non-progressive course and the absence of complications. Erosive esophagitis is observed in 37% of patients with GERD; this form of the disease can progress and be complicated by the development of bleeding, peptic ulcers and peptic strictures of the esophagus. Finally, Barrett's esophagus occurs in 3% of patients with GERD and is considered a potentially precancerous condition.
Diagnosis and differential diagnosis
24-hour monitoring of intraesophageal pH has now become widespread in the diagnosis of GERD (especially its endoscopically negative forms).
. Using this method, usually carried out in an outpatient setting, episodes of gastroesophageal reflux, manifested by a drop in pH level in the esophagus < 4, are well recognized, and their total frequency and duration are calculated. According to the results of this study, the presence of pathological gastroesophageal reflux is indicated in cases where the patient experiences more than 50 episodes of reflux during the day and/or their total duration exceeds 1 hour [8]. This method can also be used for the purpose of differential diagnosis for pain in the left half of the chest of unknown origin. Thus, by comparing the pH-gram data with entries in the patient’s diary, in which he records by the hour the time of food intake, the time of appearance and disappearance of pain, etc., one can judge whether the patient’s pain in the chest is associated with the presence of gastroesophageal reflux at this moment [9].
X-ray examination provides additional assistance in diagnosing GERD.
esophagus and stomach, especially if it is performed with the patient in a horizontal position. X-ray examination clearly reveals concomitant hiatal hernias and can help in the timely detection of tumors and peptic stricture of the esophagus.
The main place in the diagnosis of GERD and assessment of the severity of reflux esophagitis is occupied by endoscopic examination
. If the development of Barrett's syndrome or a malignant tumor of the esophagus is suspected, esophagogastroscopy should be supplemented with a targeted biopsy of the esophageal mucosa. To clarify the nature of esophageal motility disorders, esophagotonomanometry can be used. The value of this method increases when it is necessary to choose tactics for surgical treatment of patients.
Other methods used in the diagnosis of GERD include bilimetry, which allows the detection of alkaline (bile) reflux, and scintigraphy. In order to recognize endoscopically negative GERD, the so-called Bernstein test: infusion of hydrochloric acid solution into the esophagus leads to the appearance of typical clinical symptoms in the presence of GERD.
Gastroesophageal reflux disease is included in the differential diagnostic search
in the presence of unclear chest pain, dysphagia, gastrointestinal bleeding, broncho-obstructive syndrome. When making a differential diagnosis between GERD and coronary heart disease, it is necessary to keep in mind that, unlike angina, pain with GERD depends on the position of the body (occurs in a horizontal position and bending of the body), is associated with food intake, and is relieved not by nitroglycerin, but by taking antacids and antisecretory drugs. GERD can also provoke the occurrence of various heart rhythm disturbances (extrasystole, transient bundle branch block, etc.). Timely detection of GERD in such patients and its adequate treatment often contribute to the disappearance of these disorders.
The presence of Barrett's esophagus must be excluded in any patient with a long-term (more than 5 years) history of GERD. During endoscopic examination in such cases, attention is drawn to a change in the usual color of the mucous membrane of the esophagus, which becomes bright pink (sometimes characteristic “tongues” of the changed mucous membrane are revealed, stretching up the thoracic esophagus). The diagnosis is confirmed histologically by detecting small intestinal columnar epithelium in biopsies of the esophageal mucosa.
Treatment
Treatment of patients with GERD begins with general measures referred to as “lifestyle modification”. These measures include certain dietary guidelines (frequent and small meals, eating no later than 3-4 hours before bedtime, the recommendation not to lie down after eating, avoidance of coffee, chocolate and other foods that reduce the tone of the lower esophageal sphincter), stopping smoking, drinking alcoholic beverages and using medications that provoke gastroesophageal reflux, raising the head of the bed by 15-20 cm, abstaining from physical exercises associated with bending the body, normalizing body weight.
General measures are usually combined with the administration of non-absorbable antacids
, containing aluminum hydroxide and magnesium hydroxide, which can provide a quick, albeit short-lived, symptomatic effect.
Taking into account the important role of motility disorders of the esophagus and stomach in the pathogenesis of GERD, a significant place in the treatment of such patients is given to prokinetics
- drugs that normalize the motor function of the gastrointestinal tract.
Until recently, the dopamine receptor blocker metoclopramide was used for this purpose. Now they try not to prescribe this drug due to the central side effects of metoclopramide (extrapyramidal disorders) and its hyperprolactinemic effect. Domperidone
, which is a blocker of peripheral dopamine receptors, and
cisapride
, which activates serotonin 5-HT4 receptors, increase the tone of the lower esophageal sphincter, improve esophageal clearance, normalize gastric emptying and, when prescribed at a dose of 10 mg 4 times a day, have a good effect without causing central side effects and hyperprolactinemia. However, when prescribing cisapride, one should keep in mind the possibility of its arrhythmogenic effect.
Previously, prokinetics were prescribed as monotherapy (especially for non-erosive forms of GERD), proving effective in 70-80% of patients. Now these drugs play an auxiliary role and are used in combination with proton pump blockers. Currently, the effectiveness of a new prokinetic agent, the selective 5-HT4 receptor agonist tegaserod,
, which has proven itself in the treatment of irritable bowel syndrome.
In the early 90s, based on a meta-analysis of a large number of studies, the so-called “Bell's rule”, according to which healing of esophageal erosions occurs in 80-90% of cases if it is possible to maintain pH in the esophagus > 4 for at least 16-22 hours throughout the day [10]. The H2-blockers previously used for this purpose (ranitidine, famotidine, etc.), even in very high doses, were not able to fulfill this rule, and therefore they have now finally given way to proton pump blockers
(omeprazole, lansoprazole, rabeprazole, etc.). The results of a meta-analysis of 43 comparative studies, including a total of 7635 patients with GERD, showed that proton pump blockers relieve pain twice as quickly as H2 blockers, and the overall rate of pain resolution with these drugs is 77.4% and 47.0%, respectively. 6% [11].
Proton pump blockers are by far the most effective drugs used in the treatment of GERD. Prescribed in double (omeprazole 80 mg) or standard (rabeprazole 20 mg) doses, these drugs allow healing of esophageal erosions in 89-90% of patients.
Until recently, two drug regimens were most often used in the treatment of GERD. The “step-up treatment” regimen was prescribed for mild cases of the disease and provided for a sequential transition from less powerful drugs to more powerful ones. Thus, at the 1st stage of treatment, the main attention was paid to lifestyle changes and the use of antacid drugs. If these measures were not enough, then at the 2nd stage prokinetics or H2-blockers were prescribed. If there was no effect and clinical symptoms persisted, at the 3rd stage of treatment, proton pump blockers or (in especially resistant cases) a combination of proton pump blockers with prokinetics or H2 blockers were used.
When using a “step down” treatment regimen, proton pump blockers were prescribed from the very beginning, and after obtaining a clinical effect, patients were gradually transferred to taking H2-blockers or prokinetics.
Currently, proton pump blockers have occupied the main niche in the treatment of GERD, and their prescription regimen
began to be determined by the form of the disease (erosive, non-erosive, Barrett’s esophagus) (Fig. 1) [12].
Rice. 1. Algorithm for diagnosis and treatment of GERD (explanations in the text)
For the non-erosive form of GERD, proton pump blockers are prescribed in standard (
omeprazole
) or half (
rabeprazole
) doses. The main course of treatment is 8 weeks, after which patients are transferred to maintenance use of these drugs (for 26-52 weeks). Currently, a maintenance therapy regimen is being developed in the “on demand” mode, when patients themselves determine the need for maintenance use of proton pump blockers, depending on their well-being.
For the erosive form of GERD, proton pump blockers are used in double (omeprazole 40 mg) or standard (rabeprazole 20 mg) doses. The main course of treatment lasts 8-12 weeks. If the dynamics of epithelization of erosions is not good enough, the dose of rabeprazole can be increased to 40 mg per day, omeprazole - to 60-80 mg per day. In addition, prokinetic agents may be added to treatment. The combination of proton pump blockers and H2 blockers, as recent studies have shown, did not justify itself and did not lead to improved treatment results compared to monotherapy with proton pump blockers. After healing of erosions is achieved, patients are also transferred to maintenance (preferably daily) standard (omeprazole 20 mg) or half (rabeprazole 10 mg) doses.
In case of a complicated course of the disease (repeated esophageal-gastric bleeding, development of peptic strictures of the esophagus, etc.), as well as the ineffectiveness of conservative therapy, surgical treatment is indicated. The current preference is for laparoscopic Nissen fundoplication, which provides more than 90% of good to excellent results.
When Barrett's esophagus
A thorough search for dysplasia of the esophageal epithelium is carried out. In the absence of epithelial dysplasia, treatment with proton pump blockers is carried out under the monitoring of the dynamics of clinical symptoms and healing of esophageal erosions, and follow-up with endoscopic examination after a year is recommended.
If low-grade dysplasia is detected, proton pump blockers are prescribed (omeprazole at a dose of 40 mg per day, rabeprazole at a dose of 20 mg per day) for 8-12 weeks with repeated histological examination after 3 months. If low-grade epithelial dysplasia persists, it is recommended to continue continuous use of proton pump blockers with control histological examination after 3 and 6 months. Subsequently, endoscopic and histological examinations are carried out annually.
If high-grade dysplasia is detected, the issue of endoscopic
(laser or photodynamic coagulation of areas of metaplastic epithelium) or
surgical treatment
(resection). Laser and photodynamic destruction of the esophageal mucosa in Barrett's syndrome can lead to the restoration of normal stratified squamous epithelium in the esophagus. This treatment method must also be accompanied by proton pump blockers.
Thus, adherence to a strict algorithm for the diagnosis and treatment of GERD, the correct choice of medication and treatment method can achieve significant success in the treatment of this common disease and the prevention of its complications.
References:
1. Lundell L. Advances in treatment strategies for gastroesophageal reflux disease // EAGE Postgraduate Course. - Geneva, 2002. - P. 13-22.
2. Spechler SJ Epidemiology of gastro-oesophageal history of gastro-oesophageal reflux disease // Digestion.- 1992.-Vol.51.- Suppl.1.- P.24-29.
3. Dimenas E., Glise H., Hallerback B. et al. Quality of life in patients with UGI symptoms // Scand. J. Gastroenterol. - 1993. - Vol.28. — P.681-687.
4. Roshchina T.V. Gastroesophageal reflux disease in patients with bronchial asthma. Author's abstract. dis. Ph.D. honey. Sci. - M., 2002. - 21 p.
5. Peters FTM, Kleibeuker JH Barrett's oesophagus and carcinoma // Recent insights into its development and possible prevention // Scand. J. Gastroenterol. - 1993. - Vol.28. - Suppl.200. — P.59-64.
6. Sontag SJ Rolling review: gastroesophageal reflux disease // Aliment. Pharmacol. Ther. - 1993. - Vol.7. — P.293-312.
7. Quigley EMM GORD: progress in clinical understanding? // “The Art of GORD Treatment: Evolution Towards Perfection” - An Interactive Symposium. - 9 UEGW. - Amsterdam, 2001. - Abstract Book. — P.4-5.
8. Smout AJPM, Akkermans LMA Normal and disturbed motility of the gastrointestinal tract. — Petersfield, 1992.
9. Zain Ul Abidin, Ivashkin V.T., Sheptulin A.A., Trukhmanov A.S., Okhlobystin A.V. The importance of daily pH monitoring in the diagnosis of gastroesophageal reflux disease and assessment of the effectiveness of drugs // Clinical Med. - 1999. - No. 7. — P.39-42.
10. Bell NJV, Burget D, Howden CW et al. Appropriate acid suppression for the management of gastro-esophageal reflux disease // Digestion. - 1992. - Vol.51. - Suppl. 1. - P.59-67.
11. Chiba N., De Gara CJ, Wilkinson JM Speed of healing and symptom relief in grade II to IV gastroesophageal reflux disease: a meta-analysis // Gastroenterology - 1997. - Vol. 112. - 1798-1810.
12. Ivashkin V.T., Sheptulin A.A., Trukhmanov A.S., Sklyanskaya O.A., Gurvich R.N., Konkov M.Yu. Recommendations for the examination and treatment of patients with gastroesophageal reflux disease. - M., 2002. - 20 p.
Advantages of laparoscopic surgery
- Less traumatic and no pain in the postoperative period;
- Short period of hospitalization - no more than three days;
- Rapid recovery - after two weeks, patients return to their normal lifestyle.
Since patients often have other diseases that require surgical treatment, so-called simultaneous operations can be performed using laparoscopic access. I have been performing similar interventions for more than two decades. When performing a simultaneous operation during one anesthesia, you can immediately get rid of 2-5 surgical pathologies (for example, calculous cholecystitis, cholelithiasis, tumors, cysts, etc.).
Many, even experiencing painful attacks of heartburn, are in no hurry to see a doctor, trying to alleviate the condition in various ways, including with the help of medications. Is it necessary to treat reflux esophagitis if the symptoms are eliminated with the help of drugs that can be bought at any pharmacy? Of course, since there is a risk of developing severe complications. In addition, in the absence of adequate treatment, you will have to take medications throughout your life and adhere to strict dietary restrictions. At the same time, the effect of the drugs is very short-lived, and any physical activity immediately causes unpleasant and even painful sensations. To determine the extent of the disease and choose the most appropriate treatment tactics, just contact me by email or by scheduling a consultation.
Carrying out surgical interventions for diseases of the esophagus and stomach requires excellent command of surgical techniques, including endoscopic suture, which is impossible without appropriate experience. Over more than 25 years of experience, I have performed more than 2000 surgical interventions for reflux esophagitis, GERD and hiatal hernia. I am the author of monographs and more than 50 scientific papers devoted to these problems. I also regularly conduct seminars and master classes on these diseases, which are attended by specialists from various clinics and centers.