Signs and symptoms
The incubation period of the virus in the human body is 3-6 days.
In many cases, the disease is asymptomatic. When symptoms appear, the most common are fever, muscle pain with severe back pain, headache, loss of appetite and nausea or vomiting. In most cases, symptoms disappear within 3-4 days. However, in a small proportion of patients, a second, more severe phase of the disease occurs within 24 hours after the initial symptoms disappear. The temperature rises again and a number of body systems are damaged, usually the liver and kidneys. This phase is often characterized by jaundice (yellowing of the skin and eyeballs, hence the name of the disease - “yellow fever”), dark urine, abdominal pain and vomiting. There may be bleeding from the mouth, nose, or stomach bleeding. Half of the patients whose disease enters the toxic phase die within 7-10 days.
Very rarely observed reactions
If you are allergic to egg white or other components of the vaccine, normal allergic reactions may occur within a few minutes or hours after vaccination, for example, hives, swelling of the mucous membranes of the throat, accompanied by shortness of breath, or possibly a state of shock. Up to two weeks after vaccination, people who are particularly prone to allergic reactions may experience delayed allergic reactions in the form of various manifestations on the skin or muscle/joint pain, and in rare cases, a decrease in platelet levels with a predisposition to bleeding. In extremely rare cases, after primary vaccination, inflammation of the brain or its membranes may begin, or a severe disease of other organs may occur, symptomatically similar to yellow fever.
Globally, among more than 600 million people vaccinated, there have been about 100 cases of severe side effects and 25 deaths. In Germany, not a single death has been reported after vaccination. An increased risk of severe side effects (yellow fever, inflammation of the brain) primarily exists in cases of impaired protective function of the body or when vaccinating newborns under 6 months of age.
The risk group also includes older people - according to the annotation for the STAMARIL® yellow fever vaccine, vaccination of people over 60 years of age can only be performed when there is a significant and imminent risk of infection with the yellow fever virus.
If you belong to this group, you should consult your doctor before vaccination. Since organic or functional thymus disease has been observed in some vaccinated individuals who have experienced severe side effects, these should also be considered as additional severe side effects.
Diagnostics
Yellow fever is difficult to diagnose, especially in the early stages. Severe forms of the disease can be confused with severe malaria, leptospirosis, viral hepatitis (especially fulminant), other hemorrhagic fevers, infection with other flaviviruses (for example, dengue hemorrhagic fever) and poisoning.
In some cases, a blood test (RT-PCR) can detect the virus in the early stages of the disease. In the later stages of the disease, testing for the presence of antibodies is necessary (enzyme immunoassay and plaque neutralization test).
Pathological anatomy
The skin of a patient with Yellow Fever is yellow, often with a pronounced purple tint due to venous congestion. The most affected are the liver, where focal eosinophilic coagulative necrosis of liver cells develops, and the kidneys: they are enlarged in size, yellowish in color, and fatty degeneration is noted on the section. The renal cortex is indistinctly separated from the medulla. There are multiple hemorrhages in the stomach, intestines, lungs, pericardium, pleura and other organs, dystrophic changes in the heart muscle, perivascular infiltrates and hemorrhages in the brain.
At-risk groups
Forty-seven countries—in Africa (34) and Central and South America (13)—are either endemic or have regions where yellow fever is endemic. Modeling based on data from African sources estimated the burden of yellow fever in 2013 to be 84,000–170,000 severe cases and 29,000–60,000 deaths.
Occasionally, travelers to countries where yellow fever is endemic may introduce the disease to countries where it is not present. To prevent imported infections, many countries require proof of yellow fever vaccination when issuing visas, especially if the person lives in or has visited an endemic area.
In the past (17th to 19th centuries), yellow fever spread to North America and Europe, causing major outbreaks of the disease, damaging the economies of countries, disrupting their development and, in some cases, leading to the death of large numbers of people.
Clinical picture
The incubation period is 3-6 days, sometimes up to 10 days. In typical cases, the disease has a two-wave course with three periods - initial, remission and reaction. Based on severity, there are mild, moderate, severe and fulminant forms of the disease.
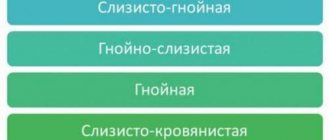
The initial, or febrile, period, also called the period of active hyperemia, lasts 3-4 days. Prodromal phenomena are usually absent. The disease usually begins acutely. Severe headache and dizziness, pain in the lower back and limbs appear. The temperature on the first day reaches 39-40° and above, accompanied by chills. Objectively, there is hyperemia of the face, neck and upper body, hyperemia of the conjunctiva, pronounced injection of scleral vessels, puffiness of the face, swelling of the eyelids, swelling of the lips, and a bright red tongue. Skin is dry and hot. Patients are euphoric, irritable, and suffer from insomnia. Characterized by thirst, nausea, and repeated vomiting of mucus. Pulse 100-130 beats per minute, blood pressure is normal, heart sounds are muffled. On the 3rd day, the patient’s condition worsens, cyanosis appears, jaundice is possible in the form of subicteric or icteric sclera, nosebleeds, bleeding gums, blood in the vomit that looks like coffee grounds, feces may be mixed with blood. The liver and spleen are slightly enlarged and sensitive to palpation. From this time on, bradycardia due to severe intoxication, oliguria, leukopenia and albuminuria are detected. The patient's appearance, called the “amaryl mask,” is characteristic: the face is puffy with a purplish-bluish tint, the eyes are shiny, the conjunctivae are hyperemic, photophobia, lacrimation, bright red lips, a restless, frightened expression.
On the 4th-5th day. from the onset of the disease, a period of remission begins (lasting from several hours to 1 day): the temperature drops to normal or low-grade levels, the condition improves significantly, headache and muscle pain weaken or disappear altogether, nausea and vomiting stop.
There may be no remission, in which case the initial period is immediately followed by a period of reaction. In mild cases, recovery begins with a drop in temperature.
Moderate and severe forms of the disease are more often observed. In these cases, the period of remission is replaced by a period of reaction lasting 3-4 days. or a period of venous stasis, characterized by severe intoxication and the absence of viremia. The condition of the patients progressively worsens, the temperature rises again, a severe hemorrhagic and icteric syndrome develops, as well as renal failure with severe albuminuria; Oliguria may give way to anuria, and azotemia is possible. During this period, the puffiness of the face disappears, hyperemia of the skin gives way to pallor with a bluish tint (venous stasis), and hemorrhages are noted on the mucous membranes. The pulse rate is 50 and even 40 beats per minute, heart sounds are muffled, sometimes with systolic murmur at the apex, blood pressure drops, extrasystole and collapse are possible. The liver is dense and painful on palpation. Indicators of bilirubin increase - direct and indirect (see Hyperbilirubinemia), aldolase, aminotransferases, bromsulfophthalein test (see), urobilinuria is recorded (see). The most common hemorrhagic manifestations are gastrointestinal bleeding (see); Less common are nosebleeds (see), hematuria (see), hemorrhagic rash. Albuminuria - up to 10 g/l or more, depending on the severity of the disease, granular and hyaline casts appear in the urine. In the blood and in this phase, leukopenia is observed (there are 1500-2500 leukocytes in 1 μl), neutropenia and lymphocytopenia, rarely leukocytosis, polyglobulia, high hemoglobin and color index, ROE accelerates, blood clotting slows down. These changes are most pronounced on the 6-7th day of illness. Death occurs more often from acute renal failure with the development of uremic coma and toxic encephalitis, less often from hepatic coma or myocarditis.
Convalescence in moderate and severe cases begins around the 10th stage of the disease, the condition of the patients improves, and all clinical and laboratory parameters become completely normal. Asthenia persists for a week. In a mild form (moderate fever lasts 1-3 days), the disease is diagnosed using laboratory methods, but it can be assumed taking into account the epidemiological situation in the endemic focus. The fulminant form leads to death on the 3rd–4th day from the onset of the disease. In moderate and severe forms, death is possible on the 6th–7th day of illness.
Possible complications: pneumonia, mumps, myocarditis, sometimes gangrene of soft tissues or extremities, kidney abscess; there may be encephalitis.
Transmission of infection
Yellow fever virus is an arbovirus of the genus flavivirus, and the main vectors are mosquitoes of the Aedes and Haemogogus species. The habitats of these mosquito species can vary: some breed either near homes (domestic), or in the jungle (wild), or in both habitats (semi-domestic). There are three types of transmission cycles.
- Forest yellow fever: In tropical rainforests, monkeys, which are the main reservoir of infection, become infected by the bite of wild Aedes and Haemogogus mosquitoes and transmit the virus to other monkeys. Periodically, infected mosquitoes bite people working or staying in forests, after which people develop yellow fever.
- Intermediate yellow fever: in this case, semi-domestic mosquitoes (those that breed both in the wild and near homes) infect both monkeys and humans. More frequent contact between people and infected mosquitoes leads to more frequent transmission, and outbreaks can occur simultaneously in many isolated villages in separate areas. This is the most common type of outbreak in Africa.
- Urban yellow fever: Major epidemics occur when infected people introduce the virus into densely populated areas with high population densities of Aedes and Haemogogus mosquitoes and little or no immunity to the disease in the majority of the population due to lack of vaccination or previous yellow fever. Under these conditions, infected mosquitoes transmit the virus from person to person.
Duration of protective effect of yellow fever vaccination and revaccination
The World Health Organization (WHO) states that acquired immunity to yellow fever is lifelong. Until recently, some countries insisted on repeat vaccinations after 10 years. However, according to current WHO guidelines, revaccination is not required.
According to the decision of the standing committee for vaccination of the Robert Koch Institute, if there is a weakened immune response in certain categories of people, then they can benefit from repeated vaccination: children under 2 years of age who have been vaccinated for the first time, especially when simultaneously vaccinated against measles, mumps and rubella , women who were vaccinated during pregnancy, as well as HIV-infected people.
Prevention
Vaccination
Vaccination is the main way to prevent yellow fever. The yellow fever vaccine is safe and inexpensive. Moreover, one dose of the vaccine is sufficient to form lifelong immunity without the need for revaccination. A number of strategies are used to prevent yellow fever and its spread: routine immunization of infants; conducting mass vaccination campaigns to expand coverage in countries at risk of disease outbreaks; vaccination of travelers to areas where yellow fever is endemic. In high-risk areas characterized by low vaccination coverage, the most important condition for preventing epidemics is the timely detection and suppression of disease outbreaks through mass vaccination of the population. At the same time, in order to prevent further spread of the disease in the region where the outbreak is recorded, it is important to ensure high immunization coverage of the population at risk (at least 80%).
In rare cases, serious side effects of the yellow fever vaccine have been reported. The incidence of these serious “adverse events following immunization” (AEFIs), where liver, kidney and nervous system damage occurs after vaccine administration, ranges from 0.09 to 0.4 per 10,000 vaccine doses in populations not exposed to the virus.
The risk of AEFI is higher in persons over 60 years of age, patients with severe immunodeficiency due to symptomatic HIV/AIDS or other factors, and persons with thymus gland disorders. Vaccination of people over 60 years of age should be carried out after a careful assessment of the potential risks and benefits of immunization.
As a rule, people who are not eligible for vaccination include:
- infants under 9 months;
- pregnant women (except in cases of yellow fever outbreak and high risk of infection);
- persons with severe forms of egg white allergy;
- persons with severe immunodeficiency due to symptomatic HIV/AIDS or other factors, and persons with disorders of the thymus gland.
Under the International Health Regulations (IHR), countries have the right to require travelers to provide proof of vaccination against yellow fever. If there are medical contraindications to vaccination, you must provide an appropriate certificate from the competent authorities. The IHR is a legally binding framework designed to prevent the spread of infectious diseases and other public health threats. The requirement for travelers to provide proof of vaccination is left to the discretion of each participating State and is not currently practiced by all countries.
Fighting mosquitoes that carry the disease
The risk of yellow fever transmission in urban areas can be reduced by eliminating mosquito breeding grounds, including treating reservoirs and other standing water with larvicide. Both surveillance and vector control are elements of strategies for the prevention and control of diseases caused by insect vectors, including those used to prevent disease transmission during epidemics. In the case of yellow fever, surveillance of Aedes aegypti and other Aedes species helps provide information about the risk of outbreaks in urban areas.
Based on information about the distribution of mosquito species across the country, it is possible to identify areas where human disease surveillance and testing need to be strengthened, and vector control activities need to be developed. Currently, the arsenal of safe, effective and cost-effective insecticides that can be used against adult mosquitoes is limited. This is mainly due to the resistance of these mosquito species to common insecticides, as well as the abandonment or recall of certain pesticides due to safety reasons or high re-registration costs. In the past, mosquito control campaigns have eradicated Aedes aegypti, the vector of yellow fever, from urban areas in much of Central and South America. However, Aedes aegypti has re-introduced urban areas in the region, again creating a high risk of urban transmission. Mosquito control programs targeting wild mosquito populations in forested areas are not suitable for preventing the transmission of sylvatic yellow fever. To avoid mosquito bites, it is recommended to use personal protective equipment such as covered clothing and repellents. Using mosquito nets on beds has limited effectiveness because Aedes mosquitoes are active during the day.
Epidemic Preparedness and Response
Rapid detection of yellow fever and rapid response through the initiation of emergency vaccination campaigns are critical tools for controlling outbreaks. However, there is a problem of under-reporting of cases, with the actual number of cases estimated to be 10 to 250 times higher than today's official statistics.
WHO recommends that every country at risk of a yellow fever epidemic have at least one national laboratory that can perform basic blood tests for yellow fever. One case in an unvaccinated population is already being considered an outbreak of yellow fever. In any case, all laboratory-confirmed cases should be subject to thorough investigation. Investigation teams must assess the characteristics of the outbreak and implement both immediate and long-term response measures.
Medicines
Photo: medsaala.com
To date, there are no drugs that can act directly on the causative agent of yellow fever. The main methods of treatment are aimed at restoring and maintaining the normal functioning of vital organs: the brain, kidneys, liver, and circulatory system. The doctor diagnoses the disease, identifies the stage of its development and prescribes therapy, which includes:
- Vitamins . The introduction of vitamins C, K and P helps provide the body with enough compounds necessary to restore normal levels of blood clotting. This measure allows you to reduce the number and volume of bleeding.
- Iron containing products . Due to numerous hemorrhages, iron deficiency is compensated not with tablets, but with the use of preparations for intramuscular administration made from the liver of cattle.
- Other medications. The treatment regimen includes medications to improve the functioning of the cardiovascular system, hemostatic agents, antihistamines, hepatoprotectors, etc.
For yellow fever, it is not recommended to use NSAIDs, as they increase the risk of bleeding. In severe cases, intensive therapy is required with the administration of large doses of glucocorticoids, infusions of solutions to eliminate acidosis, blood transfusions and blood substitutes, administration of cardiac glycosides and drugs to raise blood pressure. Patients with infectious complications are prescribed antibiotics.
WHO activities
In 2021, two linked outbreaks of yellow fever in the cities of Luanda (Angola) and Kinshasa (Democratic Republic of Congo) resulted in the disease spreading widely from Angola throughout the world, including China. This fact confirms that yellow fever is a serious global threat that requires a new strategic approach. The Ending Yellow Fever Epidemic (EYE) strategy was developed in response to the growing threat of urban yellow fever outbreaks and the spread of the disease throughout the world. The strategy is led by WHO, UNICEF and GAVI (Global Alliance for Vaccines and Immunization) and covers 40 countries. Over 50 partners are working on its implementation. The EYE Global Strategy is designed to achieve three strategic objectives: 1. protect populations at risk 2. prevent the spread of yellow fever throughout the world 3. quickly eradicate outbreaks To successfully achieve these objectives, five components are needed: 1. accessible vaccines and a stable vaccine market 2. strong political will at international, regional and country levels 3. high-level decision-making through long-term partnerships 4. synergies with other health programs and sectors 5. research and development to improve tools and practices. The EYE strategy is complex, multi-component, combining the efforts of many partners. In addition to recommended vaccination activities, the strategy calls for the creation of urban sustainability centres, urban outbreak preparedness planning and more consistent application of the International Health Regulations (2005). EYE Strategy partners are supporting countries at high and moderate risk of yellow fever in Africa and the Americas by strengthening their surveillance and laboratory capacity to respond to yellow fever outbreaks and cases. In addition, EYE strategy partners support the deployment and sustainable implementation of routine immunization programs and vaccination campaigns (preventive, proactive and reactive) anywhere in the world and at any time when needed.
Course of action after vaccination
For one week after vaccination, you should avoid excessive physical activity (sports, surgery, sauna), exposure to the open sun (sunbathing), and excessive alcohol consumption. You cannot donate blood for four weeks after vaccination. Conception should be avoided for three months or at least 4 weeks after vaccination. Vaccination during pregnancy or conception immediately after vaccination cannot cause termination of pregnancy. Vaccinations should not be performed while breastfeeding. If, within a certain period of time after vaccination, you experience symptoms that you attribute to the vaccination, you should consult your doctor.
To assess the possible risks of side effects after yellow fever vaccination, as well as to exclude contraindications, please answer all the questions in the vaccination form! If you have any additional questions, you can discuss them with your vaccinologist. More information on this topic is available from the M1 Center for Travel and Tropical Medicine.
Laboratory data
The initial stage of the disease is characterized by leukopenia with a sharp shift to the left, neutropenia, thrombocytopenia, at its height - leukocytosis, progressive thrombocytopenia, increased hematocrit, blood nitrogen and potassium. The amount of protein in the urine increases, red blood cells and casts appear. Hyperbilirubinemia and high activity of aminotransferases (mainly AST) are noted. In specialized laboratories, it is possible to isolate the virus from the blood in the initial period, using biological diagnostic methods (infection of newborn mice). Antibodies to the virus are determined using RNGA, RSK, RNIF, indirect hemagglutination inhibition reaction, ELISA.
Interesting Facts
American physician John Gorrie was a proponent of the theory that polluted hot air causes, if not the occurrence of yellow fever, then, ultimately, a poor prognosis for patients with this disease. In 1851, while working at a hospital in Apalachicola, Florida, he patented a cooling device that could cool a hospital room. His device could serve as both a freezer and an air conditioner. However, Gorry’s work was not accepted by his contemporaries, he was humiliated by critics in the slanderous campaign launched against him, and financially damaged, the talented doctor died in 1855 in poverty and complete oblivion. Half a century later, the principle of this type of cooling was used very successfully to create household refrigerators, and then air conditioners...
The famous English novelist and playwright, member of the House of Commons Matthew Gregory Lewis, who created one of the best Gothic novels, The Monk, died of yellow fever on a ship en route from the West Indies to England on May 14, 1818.
The causative agent of yellow fever
The causative agent of the disease is a virus (Viscerophilus tropicus, Yellow Fever virus, YFV) of the Togaviridae family, genus Flavivirus. Belongs to the group of arboviruses (transmitted by vectors).
The virus is filterable, small (12 - 27 nm in diameter), spherical in shape.
The genome contains (+) single-stranded RNA.
According to its antigenic structure, the pathogen has an affinity with the viruses of Dengue fever, St. Louis encephalitis and Japanese encephalitis. Belongs to the 1st group of pathogenicity.
Shows sensitivity to high temperatures (inactivated at temperatures of 55 - 600C and when exposed to disinfectant solutions. It is preserved for a long time when dried, it is stored in a frozen state for more than a year. It survives in the bodies of dead mosquitoes for up to 4 weeks at a temperature of 27 - 300C.
Viruses are cultivated in chicken embryos and mouse testicles. Repeated passages significantly weaken their pathogenicity, which is used to obtain vaccine strains.
The pathogens are pathogenic to primates, sloths, opossums, anteaters, guinea pigs and white mice.
Rice. 2. In the photo, the causative agent of the disease is a virus (Yellow Fever virus).
Treatment
Strict bed rest, a fortified, high-calorie sparing diet is prescribed, taking into account organ pathology. Patient care and monitoring the dynamics of clinical and laboratory parameters are of exceptional importance.
Specific therapy has not been developed. Although there is a hypothetical idea about the possibility of using ribavirin, it did not show any effect on primates suffering from yellow fever. There are currently no convincing results from the use of interferons. Pathogenetic and symptomatic therapy is carried out, which includes detoxification, antishock and hemostatic agents, taking into account the severity of a particular syndrome, respiratory support, transfusion of same-group plasma or blood (in case of massive blood loss), diuretics, correction of acid-base balance. With the development of acute renal failure, hemodialysis is indicated. To prevent the occurrence of bacterial complications, it is recommended to prescribe broad-spectrum antibiotics (excluding hepato- and nephrotoxic ones).
Activities in the epidemic outbreak
Patients are hospitalized in the infectious diseases department. If a sick person is detected on a ship during a voyage, he is isolated in a separate cabin. Disinfection is not carried out in the outbreak. Any vehicle arriving from countries affected by yellow fever must have information about the disinfestation carried out. Unvaccinated persons arriving from endemic areas are subject to isolation with medical supervision for 9 days. If an outbreak of yellow fever occurs, mass immunization of the population begins immediately.
Source: “Infectious diseases and epidemiology” V.I. Pokrovsky, 2007