December 14, 2020
In our medical center you can get vaccinated against pneumococcal infection. We tell you who needs it and why, what vaccine we use, and whether the pneumococcal vaccination can protect against COVID-19.
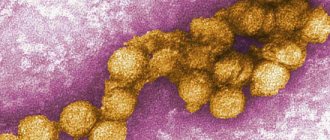
Pneumococcus (Streptococcus pneumoniae) is the causative agent of bacterial infections that manifest as pneumonia, otitis media, meningitis, sinusitis, etc. Pneumococcal pneumonia poses the greatest danger to young children, the elderly, and people with certain health conditions.
It is known that more than 1.5 million people die worldwide each year from complications caused by Streptococcus pneumoniae.
Streptococcus pneumoniae - a formidable bacterium
On the one hand, Streptococcus pneumoniae is a representative of the normal microflora of the human upper respiratory tract. Up to 70% of people are carriers of one or more types of pneumococci. “Organized” (living or being in groups) children and adults have the highest level of carriage. More than 90 different serotypes (immunological variants) of pneumococci are now known. On the other hand, all pneumococci are potentially pathogenic, and about 20 of them cause severe infections.
The saddest thing is that pneumococci have developed resistance to many antibiotics. In countries where antibiotics are widely used, the level of resistance of Streptococcus pneumoniae to penicillin reaches 50% of all isolated pneumococci, and to tetracycline and chloramphenicol - up to approximately 30%.
The problem is aggravated by the fact that the rapid development of the disease - 2-3 days - as a rule, does not leave time for a special determination of the sensitivity of pathogens to antibiotics. Patients with severe infection often die despite standard antibiotic therapy.
Who is at risk for pneumococcal infection?
- people aged 55 years and older;
- children;
- adults with chronic diseases;
- so-called “organized contingents” - children who go to kindergarten, residents of nursing homes and homes for the disabled, military personnel, etc.
Possible side effects
In children 6 weeks to 17 years of age, the most common side effects are irritation, redness or swelling at the injection site, irritability, decreased appetite, decreased or increased sleep, and fever.
Serious but very rare side effects in infants and toddlers include pneumonia, bronchiolitis and gastroenteritis (inflammation of the stomach and small intestine) (0.9% of all vaccine recipients). A temporary pause in breathing after vaccination occurs in some babies born prematurely.
The high safety of vaccination has been confirmed by 230 million years of experience in administering Prevenar over the past 10 years. The vaccine is registered in 88 countries and is included in the national vaccination calendars of 30 countries.
Come get vaccinated at VIRILIS. A full range of vaccines for children and adults, family vaccinations - at a special price!
Vaccination against pneumococcal infection
In Russia, vaccination against pneumococcus began in 2008 using the Prevenar 7 vaccine. Currently, the following are registered in the country:
- Prevenar 7 and Prevenar 13 (Pfizer),
- Pneumovax 23 (Merck Sharp & Dohme Corp),
- Synflorix (GlaxoSmithKline).
The national vaccination schedules of most developed countries include the Prevenar vaccine; it is recommended by the World Health Organization. At the medical level, residents of Novosibirsk can get vaccinated against pneumococcus with this particular drug.
The effectiveness is confirmed by research! The Prevenar vaccine has been used in the United States since 2000. Already in the first 5 years, the frequency of severe forms of infection in children under 4 years of age decreased by 40 times. According to American researchers, the reduction in the number of pneumococcal carriers, which was achieved through mass vaccination with Prevenar, led to a twofold decrease in visits to doctors for otitis of any etiology.
Wanting to achieve greater effectiveness of the drug against complicated pneumonia, scientists created a new 13-valent vaccine. It contains additional strains of pneumococcus, which are responsible for the development of complications of pneumonia.
According to the Russian vaccination calendar, vaccination against pneumococcal infection is mandatory for all children under 5 years of age. For adults, vaccination is recommended when indicated. It is indicated for conscripts, older people with chronic lung diseases, and pensioners who live in boarding schools and nursing homes.
In general, vaccination can be recommended for all people over 55 years of age and adults with chronic diseases.
Prevenar vaccination schedule
- When vaccinating children under 2 years of age according to the National Calendar, the vaccine is administered three times (at 2 and 4.5 months and at 15 months).
- When vaccinated after two years of age - a single injection intramuscularly into the shoulder.
There are 4 vaccines registered in our country:
- Prevenar (Pfizer, USA/UK) – contains a mixture of purified capsular polysaccharides of 7 serotypes of Streptococcus pneumoniae, individually conjugated to a diphtheria carrier protein, used in children from 2 months to 5 years.
- Prevenar 13 (Pfizer, USA/UK) – the vaccine contains a mixture of purified capsular polysaccharides of pneumococcus 13 serotypes.
- Pneumo 23 (Sanofri Pasteur, France) – contains a mixture of purified capsular polysaccharides of 23 serotypes of pneumococcus, used in children over 2 years old, administered once in frequently ill children, as well as in children with severe oncological and hematological diseases.
The following vaccination schedule with Prevenar vaccines is recommended: if vaccination begins after 6 months, the vaccine is administered 3 times (two injections in the 1st year of life with an interval of 1 month, the 3rd injection in the 2nd year of life). If the vaccine is administered in the 2nd year of life in the period from 12 to 15 months, it is recommended to administer it twice with an interval of 2 months; when vaccinated after 2 years, it is administered once intramuscularly into the shoulder.
Currently, the vaccine Synflorix (Glaxo Smith Klein Biologicals) is being registered - a mixture of purified capsular polysaccharides of 10 serotypes of pneumococcus.
All children from 1-2 years of age to 5 years are subject to vaccination against pneumococcal infection; it is especially important for frequently ill children and elderly people over 55 years of age.
Can the pneumococcal vaccine protect against Covid?
In late summer and fall 2021, reports emerged that the pneumococcal vaccine could protect against Covid-19 infection. Actually, no—it only prevents pneumococcal infections. On the other hand, many scientists and doctors believe that the pneumococcal vaccine can protect the patient from secondary complications of coronavirus infection.
In any case, vaccination against other respiratory diseases is still highly recommended during the Covid-19 pandemic.
There are no complications after vaccination with Prevenar. The patient may experience increased temperature and redness at the injection site. However, such a reaction usually occurs in people who have already had pneumococcus.
To get vaccinated, please make an appointment with our vaccination doctor by phone or online chat on the website.
Compatibility with other vaccines
"Prevenar" is combined with any other vaccines included in the immunization schedule for children in the first years of life. "Prevenar" can be administered to children simultaneously (on the same day) with any of the following antigens included in both monovalent and combined vaccines: diphtheria, tetanus, acellular or whole-cell pertussis, Haemophilus influenzae type b, inactivated polio, hepatitis B, measles, mumps, rubella and chickenpox - without changing reactogenicity and immunological parameters.
When simultaneous vaccination with Prevenar and other vaccines, injections are made in different parts of the body.
What components may be contained in modern vaccines?
There are different classifications of drugs for active immunization:
Live with an artificially weakened pathogen
The immune system sees the pathogen in much the same way as a real virus or bacterium. The difference is that it cannot cause disease, because to the extent that it has ceased to be pathogenic. This type of “live” vaccines includes drugs against the following infections: polio (oral vaccine), tuberculosis (BCG vaccine), rubella, measles, mumps, chickenpox, brucellosis, Q fever, etc.
Killed (inactivated)
This case differs from the first only in that the infectious agent is no longer alive and contains killed whole microorganisms (bacteria and viruses) or their parts.
Note:
When it comes to viruses, it is incorrect to talk about a “live” or “dead” virus, because, from the point of view of science, viruses are not something living. It is more correct to talk about virulent ones, i.e. capable of infecting and causing a full-fledged disease, and inactivated - not capable of causing a disease, but sufficient to develop an immune response. For convenience, we will call them alive/killed, especially since this expression has already become firmly established in everyday life.
Examples of inactivated vaccines: against whooping cough (whole cell), against polio (IPV), etc.
Anatoxins
These drugs contain neutralized (inactivated) bacterial toxins that are immunogenic and non-toxic. They are no longer poisonous to the body, but are still capable of causing an immune response. Vaccines are made based on toxoids, for example, against diphtheria, tetanus, whooping cough (a vaccine with an acellular pertussis component).
Note:
An interesting fact is that with natural infection with tetanus, immunity to it is not formed. Because the toxin content in the blood is not enough to form immune memory, and a higher concentration leads to death. In this case, an inactivated toxin is the only opportunity to gain immunity and not be afraid of this infection.
Artificial antigens
The material for creating artificial antigens is recombinant proteins or their fragments synthesized in laboratories using genetic engineering methods. In this case, the vaccine developer acts as an engineer of the design that will be administered to the patient.
To create such a vaccine, it is necessary to go through several stages of development: - first, one of the pathogen proteins is selected to which the immune system responds well; — in the laboratory, a specially “trained” cell culture is created, which will produce this protein according to instructions (gene modification is carried out by inserting a sequence encoding the desired protein into the genome of the producing cells); — provide this culture with everything necessary for the modified cell to actively multiply and produce antigens for the vaccine;
- after some time, they “harvest” by isolating the desired protein from the solution.
An analogy can be drawn with the process of conventional fermentation. That is, “yeast” will act as that specially trained cell culture, and “alcohol” will act as the desired substance that we want to obtain from these cells. Fruit or sugar is food for yeast. The difference is that yeast “knows how” to produce alcohol, but antigens, for example, for a vaccine against viral hepatitis B, do not.
The peculiarity of vaccines with artificial antigens is that they do not contain the real infectious agent at all. Relatively speaking, part of the virus was printed many times on a 3D printer, i.e. cloned.
Examples of such vaccines: against the hepatitis B virus, against the human papillomavirus (HPV).
Routes of infection and symptoms
Pneumococcal infection spreads by airborne droplets, that is, by sneezing or coughing, especially if a sick person is near you. Moreover, the source of infection can be a person without any symptoms. The peak incidence occurs in winter and early spring. The incubation period ranges from 1 to 3 days.
Symptoms of pneumococcal infection
- fever
- cough
- dyspnea
- chest pain
Symptoms of pneumococcal purulent meningitis
- stiff neck
- fever
- confusion and disorientation
- photophobia
Symptoms of pneumococcal bacteremia (a blood poisoning with a mortality rate of up to 50%) may be similar to pneumonia and meningitis, but also include:
- joint pain
- chills
Contraindications
For pneumococcal conjugate vaccines: increased sensitivity to previous vaccination (severe generalized allergic reactions); hypersensitivity to diphtheria toxoid and/or excipients; acute infectious or non-infectious diseases, exacerbations of chronic diseases. Vaccinations against pneumococcal infection are carried out after recovery or during remission. Pneumococcal polysaccharide vaccines: pronounced reaction to the previous vaccination, PPV23 vaccination less than 3 years before the intended PPV23 vaccination.