Prevalence
In the International Classification, the disease is recorded under code K29.6 in the group “Other gastritis”. Since separate records of the disease are not kept, we can rely on data on postoperative complications and studies on attendance at clinics.
It has been shown that duodenogastric reflux occurs in 52.6% of cases as a consequence of operations on the duodenum, and in connection with removal of the gallbladder - in 15.5%. Symptoms similar to biliary reflux gastritis are detected in 25–40% of adults.
Methods for diagnosing and treating gastritis
- Consultation with a gastroenterologist
- Test for Helicobacter pylori
- FGSD (gastroscopy)
- Daily pH monitoring for gastrointestinal examination
- Colonoscopy
The diagnosis is made exclusively by a gastroenterologist based on the patient’s complaints, as well as data from the gastroscopy required in this case.
When treating gastritis, it is necessary to follow a diet that recommends eating at the same time about five times a day. Excluding alcoholic drinks, fatty meats, smoked meats, and shortcrust pastry products. It is very important to stop smoking and drinking alcohol when gastritis occurs.
Experienced doctors at SM-Clinic are ready to assist you in the treatment of diseases of the gastrointestinal tract. You can make an appointment 24 hours a day.
Sources:
- I'M WITH. Zimmerman, Yu.A. Zakharova. Problematic issues of the doctrine of chronic gastritis // Clinical medicine, 2021, No. 95(1), pp. 8-14.
- Sh.Z. Galiev, N.B. Amirov, O.A. Baranova. Morphological signs of reflux gastritis // Kazan Medical Journal, 2021, v. 98, no. 4, p. 533-537.
- Coati I, Fassan M, Farinati F, Graham DY, Genta RM, Rugge M. Autoimmune gastritis: Pathologist's viewpoint // World J Gastroenterol. 2015 Nov 14;21(42):12179-89. doi: 10.3748/wjg.v21.i42.12179.
Causes and provoking factors
To understand why bile enters the stomach, which should be no higher than the duodenum, is necessary to determine the causes of the pathology. The greatest importance is attached to functional disorders of motility (peristalsis) of the stomach, its muscle tone, especially the sphincters. They manifest themselves as accelerated content release or delay. Accordingly, a distinction is made between hyper- and hypokinesia, hyper- and hypotension.
The most common is spastic contraction of the pylorus. In addition to inflammatory diseases of the stomach and duodenum, it is observed in neuroses, mental stress, in people with hysteria, and occupational intoxication. In case of decompensation, the stomach cavity expands. In differential diagnosis it is difficult to distinguish from cicatricial pyloric stenosis.
Hypotension and gastric hypokinesia accompany habitual overeating, drinking too much, and eating fatty foods. Similar disorders are observed with gastritis, enteritis, colitis, cholecystitis, and accompany many serious diseases of other organs, the nervous system (toxic paralysis), and postoperative complications.
Weakened peristalsis and gastric tone (paresis) lead to a gaping of the pylorus, through which contents can be thrown back from the duodenum
Dyskinesia is a group of disorders in the coordination of contraction of the gastric sphincters. They cause reflux of gastric contents into the esophagus, which provokes reflux esophagitis, and from the duodenum into the stomach. In the first case, gastroesophageal reflux disease of the esophagus develops. In this case, the main damaging substance is gastric acid.
Duodenogastric reflux is typical for hiatal hernia, peptic ulcer, duodenitis, pancreatitis, cholecystitis and inflammation of the biliary tract. Here the stomach suffers due to the action of irritating components of bile.
In a healthy person, contents from the underlying sections cannot reach higher levels due to the work of special stomach muscles (sphincters) located at the borders of the organ. They compress sufficiently after the passage of food and do not allow backflow.
Biliary or bile reflux gastritis is caused by the combined influence of several factors:
- impaired contractile function of the pylorus;
- decreased sphincter tone at the border of the stomach and duodenum;
- impaired motility of the digestive organs;
- chronic stagnation of duodenal secretions;
- consequences of surgical intervention on the digestive organs (gastric resection, pyloroplasty, gastroenterostomy, cholecystectomy);
- irritable bowel syndrome;
- prolapse of the stomach (gastroptosis);
- chronic hepatitis;
- peptic ulcers;
- taking non-hormonal anti-inflammatory drugs, antibiotics, painkillers, drugs containing iron and potassium, the action of the drugs causes blocking of the synthesis of prostaglandins, then mucus in the stomach;
- alcohol abuse;
- systemic disorders of nervous and endocrine regulation.
Some medical scientists disagree with the leading role of duodenogastric reflux in the development of biliary inflammation of the stomach. Their position is based on the fact that the gastric epithelium is considered quite resistant to the action of bile. They attribute the process to a physiological protective reaction that allows one to regulate acidity with alkaline contents in response to increased synthesis of hydrochloric acid.
Smoking is one of the provoking factors of pathology
The following factors can complement the listed factors: food excesses, wearing tight clothes, smoking, stressful situations. Biliary reflux occurs temporarily during pregnancy.
How does the surface of the stomach change?
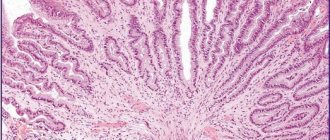
Morphological changes often occur years later. In the section closest to the intestine—the antrum—epithelial cells grow rapidly, and the mucous goblet glands disappear.
The surface becomes swollen, and an accumulation of basophilic leukocytes saturated with nucleic acids is observed. They cause mild inflammation. A long process leads to cell degeneration and then to necrobiosis. Erosion forms and the production of protective mucus stops.
First, a focal process develops. It is possible that areas of mixed inflammation may coexist, alternating with normal mucosa. Subsequently, areas of atrophy grow. If left untreated, the epithelium may transform into malignant with the development of a tumor.
Kinds
Based on the nature of the lesion and the localization of inflammation in the stomach, the following forms of biliary reflux gastritis are distinguished:
- superficial - epithelial dystrophy is typical;
- catarrhal - swelling and inflammation of the inner membrane are associated;
- erosive - deep layers are affected, necrobiosis of cells forms erosions, and symptoms such as bleeding appear;
- antral - indicates the development of gastritis in the lower part of the organ (pyloric canal, antrum, pyloric sphincter), this zone is the first to be affected and suffers the most.
Since there is no single classification, some authors highlight:
- acute biliary reflux gastritis;
- fibrinous with the release of fibrinous-purulent exudate;
- necrotic;
- purulent.
Symptoms
The disease develops gradually and has a chronic course. The most common symptoms:
Signs of atrophic gastritis of the stomach
- pain in the epigastric region on an empty stomach, of varying nature and intensity (acute or constant aching);
- feeling of heaviness in the upper abdomen;
- bloating (flatulence);
- belching of eaten food and air;
- heartburn;
- nausea;
- periodic vomiting of bile;
- unstable stool (alternating diarrhea and constipation);
- decreased appetite;
- weight loss
Digestive disorders cause anemia and hypovitaminosis. They are manifested by increased fatigue, dizziness, dry skin, cracks in the corners of the lips.
The bitter taste in the mouth increases the nervousness of patients
Chronic reflux gastritis is characterized by a wave-like course. There are asymptomatic cases that are detected by fibrogastroscopy. The severity of the symptom is always parallel to the degree of damage to the mucous membrane.
Doctor's comment
If you are worried about heartburn and nausea, and your usual medications and strict adherence to a diet do not bring relief, if you often experience abdominal pain that gets worse after eating, perhaps the cause of this condition is duodenogastric reflux. You can determine its presence in our clinic, where for a high-quality examination you can undergo all the necessary diagnostic procedures - at any time convenient for you. Treatment tactics depend on the degree of the disease. This may be drug therapy or surgical treatment, which is indicated when conservative methods are ineffective. Our patients have the option of treatment in a day hospital. The operation in the clinic is carried out using laparoscopy: all actions are carried out through 3-4 punctures on the abdomen, which subsequently become invisible. During the operation, which is painless and bloodless, the likelihood of complications is virtually eliminated. After 1-3 days, our patients are discharged from the clinic; in the future, there is no need to take medications or strictly follow a diet. Therefore, do not delay treatment, because with advanced duodeno-gastric reflux, treatment will be more difficult and longer.
Head of the surgical service at SwissClinic Konstantin Viktorovich Puchkov
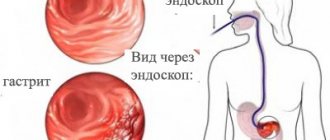
Diagnostics
The doctor becomes suspicious of the disease after careful questioning and clarification of the patient’s complaints, when the cause is identified. Special attitude towards persons who have undergone surgery. They are additionally examined by a surgeon. Indirect confirmation of digestive disorders is possible through blood and stool tests (scatology + occult blood).
The basis of diagnostics is hardware research. Fibrogastroduodenoscopy reveals foci of inflammation in the antrum, swelling of the epithelium, and widening of the sphincter opening between the duodenum and the pyloric part of the stomach.
Modern interpretation of gastritis requires assessment of the condition of the mucosa using a biopsy taken during fibrogastroduodenoscopy. In this way, the form of the disease is confirmed and the presence of epithelial metaplasia during the transition to cancer is checked.
To study the motility and contractility of the gastroduodenal zone, antroduodenal manometry or gastrography is used.
If necessary, daily pH measurements are carried out using the Gastroscan apparatus.
Acidity measurements using pH measurements and the use of a histamine test make it possible to study the influence of the level of acid formation in the stomach. X-ray of the stomach and intestines using a barium suspension helps to trace the movement of stomach contents, record violations of the contraction of the pyloric sphincter and reflux in the images. To check the participation of other organs of the digestive tract in the pathogenesis, an ultrasound of the abdominal cavity is performed.
Conservative treatment of duodenogastric reflux
The goal of conservative therapy is to neutralize the aggressive effect of duodenal contents on the mucous membrane of the stomach and esophagus, improve the evacuation capacity of the stomach and antroduodenal coordination. For this purpose, drugs are prescribed that normalize the motility of the upper gastrointestinal tract, prokinetics, enhancing the peristalsis of the stomach and duodenum and improving the evacuation of their contents, antacids, etc.
In addition, since duodenogastric reflux is often combined with other diseases of the digestive system, drugs are also needed to treat the underlying pathology. In addition, great importance is given to following a diet and giving up bad habits. Conservative treatment is difficult, and although the clinical manifestations of reflux decrease with medication, this is only a temporary improvement. It is possible to achieve good results with conservative therapy only in case of functional disorders that cause reflux.
Treatment of biliary reflux gastritis
Therapy of the disease requires the patient to quit smoking, drinking alcohol, fatty, spicy and fried foods. Much more attention will have to be paid to proper nutrition and adherence to the regime. Intense exercise on the abdominals is not recommended. Muscle tension increases intraperitoneal pressure and promotes reflux movements.
To relieve the negative effects of acidity, drugs and folk remedies with an enveloping effect are used: Maalox, Almagel, decoction of flax seeds, oatmeal jelly. Almagel A also contains Anestezin, so it provides good pain relief to the inflammatory zone. For high acidity, drugs that block the secretion of gastric juice (Omeprazole, Rabeprazole) and histamine receptor blockers are indicated.
Hydrotalcite - contains combined minerals (magnesium, aluminum) that suppress acid secretion
A group of prokinetics is prescribed to improve the tone of the pyloric sphincter and the muscular layer of the stomach (Primer, Motilium, Motilak). Domperidone and Metoclopramide prevent reflux into the stomach. In order to bind bile acids and improve the outflow of bile, ursodeoxycholic acid preparations (Ursofalk, Ursosan, Ursachol, Holacid) are used.
In case of a long course of the disease, vitamins A, E, group B are certainly prescribed. If the examination excludes suspicion of an erosive form and oncology, then courses of physiotherapy are effectively used:
- amplipulse therapy is a method of restoring gastric motility and normalizing secretory function;
- exposure to decimeter waves and ultra-high frequency - relieves swelling of the mucous membrane, pain, stimulates healing.
Indications for acupuncture are considered individually.
Folk remedies
Traditional medicine recipes are popular among patients with moderate biliary reflux gastritis. The decoctions must be taken over a long period of time. Recommended:
- combined use of chamomile, St. John's wort and yarrow;
- dandelion and mint flower syrup.
Typically, chamomile, plantain, calendula, and dandelion are used for low acidity, but their anti-inflammatory properties are needed to treat gastritis. Therefore, use in combination and mixtures is permitted.
Surgical treatment
Surgical intervention for biliary gastritis is rarely used. Usually they operate on emergency indications (bleeding), or routinely when non-healing ulcers, erosions, and tumor formations are detected.
To prevent reflux gastritis, it is necessary to exclude factors that provoke the disease. Monitoring your health after surgery allows you to start preventive treatment earlier and identify complications. Therefore, patients should be examined at least once a year.
Surgical treatment of GHD
If conservative correction is ineffective, surgical intervention is indicated; the purpose of the operation is to strengthen the pyloric valve, as well as reduce the volume of bile thrown into the stomach. The operation is carried out in several directions:
- elimination of the causes that led to duodeno-gastric reflux;
- pyloroplication – performed to reduce symptoms of pyloric dehiscence;
- in the presence of hiatal hernia and calculous cholecystitis, fundoplication with crurorrhaphy and cholecystectomy is indicated.
In our clinic, laparoscopic access is used for surgical treatment of patients with GHD - all surgeon actions are performed through 3-4 punctures on the abdominal wall, and the length of the incision does not exceed 10 mm. Moreover, the operation itself is low-traumatic and painless; during its implementation, the likelihood of complications and blood loss are excluded. As a rule, the patient can go home within 2-3 days; work capacity is restored 2-3 weeks after surgery.