1.General information
As you know, ribs are not only part of the musculoskeletal system, but also serve as mechanical protection for vital internal organs: heart, lungs, liver, gall bladder, etc. Therefore, any pain behind or under the ribs should alert you. If pain discomfort in the hypochondrium has become recurrent or chronic, you should definitely consult a doctor: there are simply no problems in this area that can be neglected. But it is, on the contrary, very easy to waste precious time and miss the development of a dangerous pathology, and this happens, unfortunately, all the time in clinical practice.
On the left under the ribs there are many potential sources of pain: individual parts of the intestines, stomach, spleen, pancreas. Heart pain often radiates to the left hypochondrium, but it would be wrong to assume that “any pain on the left is from the heart.” Possible causes are far from limited to cardiac problems.
A must read! Help with treatment and hospitalization!
Gastrointestinal pathologies
Gastritis and stomach ulcers may be accompanied by a burning sensation on the left side of the abdomen. The pain usually intensifies with long breaks between meals and is accompanied by nausea, vomiting and heartburn. Treatment of gastritis depends on its form. When acidity is high, antacids are prescribed, and when acidity is low, enzymatic preparations are prescribed. A strict diet is recommended. Stomach ulcers require antibiotics, antihistamines, and proton pump blockers.
The cause of the burning sensation may be pancreatitis. When the patient's pancreas becomes inflamed, the production of enzymes decreases and the digestion process is disrupted. Burning sensations on the left turn into girdle pain. In this case, nausea, fever, and malaise are noted. The patient is advised to follow a special diet, as well as take enzymes and antibiotics.
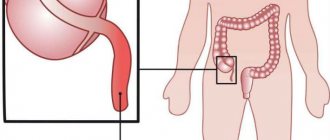
The sigmoid colon is located on the left side of the abdominal cavity. Inflammation of this organ (sigmoiditis) may be accompanied by a burning sensation. The pain intensifies before defecation and when walking. The patient has diarrhea, stool looks like meat slop and has an unpleasant odor. Sigmoiditis is usually a consequence of other gastrointestinal diseases. You can get rid of this pathology only by curing the underlying ailment.
A burning sensation that turns into cramping pain may be one of the first signs of dysentery. This infectious disease is caused by bacteria called Shigella. The patient's health sharply worsens, nausea, general malaise, and severe diarrhea mixed with blood (stools up to 10 times a day) occur. Often there are false painful urges to defecate. The patient must undergo a course of antibacterial therapy, otherwise dysentery may become chronic.
2. Reasons
The most common causes of pain in the left hypochondrium include:
- diseases of the stomach in their entire spectrum (from mild dyspepsia to peptic ulcer of the stomach and/or duodenum);
- enlargement (splenomegaly) or damage to the spleen (especially bruises with rupture);
- inflammatory processes in the pancreas (pancreatitis);
- malignant neoplasms that have reached a certain size;
- pyelonephritis, calculi (stones) in the left kidney;
- myocardial infarction and (less commonly) other heart diseases;
- osteochondrosis;
- pathology of the diaphragm (usually an abscessing inflammatory process);
- lung damage (pneumonia, metastatic stages of cancer, etc.).
However, this list is not complete. Some neurological and endocrine disorders can also manifest as pain in the left hypochondrium; finally, the reason may lie in damage to the ribs themselves - their bruise or fracture.
Visit our Therapy page
What kind of pain is there?
Information about the location of unpleasant sensations gives the doctor an almost exact picture of what exactly is happening to the patient at the moment.
- Constant pain with a clear localization is called peritoneal. It is considered a symptom of exacerbation of inflammatory processes in the gastrointestinal tract or kidneys, and is felt more strongly during breathing and when walking.
- If the patient complains of discomfort in the front, then this is a direct indication of injury to the spleen or stomach.
- When an unpleasant feeling shifts to the center of the abdomen, then gallbladder disorders can be suspected.
- When a patient talks about the localization of pain in the back, then in most cases, this is an indicator of damage to the left renal pelvis or developing pyelonephritis.
- Such pain may appear during examination if a person suffers from osteochondrosis in the thoracic region.
- The pain may be described as stabbing. This is one of the main symptoms of acute pancreatitis. The discomfort may be relieved slightly if the person sits or leans forward.
Doctors also highlight visceral pain, which can develop with intestinal colic, excessive accumulation of gases, and also with sprained muscles and ligaments. Another mechanism of occurrence is referred pain. Develops as a result of disruption of the functioning of organs not located in the abdomen. As a rule, it is localized there during myocardial infarction, as well as inflammatory changes in the tissues of the lungs: pneumonia and pleurisy.
Table. Nature of pain by group.
| Group | Description |
| Visceral | This group includes pain associated with pathological changes in gastrointestinal motility. The pain is dull and can be jerky or cramping. They radiate to both the shoulder and thigh area. Most often occur with intestinal spasms. The cause may also be stretching of muscle fibers. With acute flatulence, the pain is cramping in nature, and with intestinal colic it radiates to all nearby organs. |
| Peritoneal | They arise due to irritation of peritoneal receptors, which occur as a result of ruptures of organs and the release of their contents into the surrounding tissue. They are distinguished by the severity of their manifestations, cutting, clearly localized, lasting constantly, intensifying with activity and stress. More often they are encircling. May occur when a gastric ulcer perforates. They intensify with any load, movement, even with breathing, from inhalation and exhalation. |
| Spastic | They are generated by a spasm of smooth muscles. They occur with pathologies of internal organs of any nature - from colic to poisoning. They appear suddenly and just as suddenly go out. They can radiate to the shoulder blade and lower back, as well as to the legs. |
| Reflected | The cause of these pains is inflammatory changes. They can be different in duration and in character too - from aching and pulling, to pain and colic. They are “reflected” from organs located quite far from the left hypochondrium. They can occur with a heart attack, pleurisy, left-sided pulmonary inflammation and other diseases. |
| Psychogenic | This type of pain is not at all associated with diseases of any internal organs. Neurotic pain that cannot be diagnosed. But the patient is not pretending, but may actually experience acute pain, especially when in a depressive state or in the stage of a mental disorder. |
For example, with cardiomyopathy, pain is felt after exercise, with pneumonia - during coughing, with stomach and intestinal infections, pain is associated with meals, intensifying after eating, and with stomach cancer it is constant.
3. Symptoms, diagnosis
Pain in the left hypochondrium, given the huge number of possible causes, is so diverse that its common property can only be considered localization at the edge of the costal arch. However, options are also possible here: pain in the left hypochondrium in the front carries slightly different information than pain on the side or behind. The nagging, tolerable, but almost constant debilitating pain in chronic inflammation of the internal organs is incomparable with the sharp, dagger-like pain in renal colic, perforated gastric ulcer or myocardial infarction.
Therefore, quick and accurate diagnosis of the causes is very important. For this purpose, the most detailed anamnesis is collected, an external examination, palpation (palpation), auscultation (listening), percussion (tapping) is necessarily performed, and for an experienced doctor these “ancient” methods are sometimes as important and informative as the most modern high-tech ones devices. As the situation becomes clearer, additional tests are prescribed and/or the patient is referred to a specialized specialist.
Obviously, in the diagnosis of subcostal pain, imaging methods are of great importance: various types of radiography, ultrasound, and tomography. In some cases, the primary role is given to laboratory analyzes of biological fluids, in others, only a biopsy, endoscopy or diagnostic laparoscopy can provide decisive answers.
About our clinic Chistye Prudy metro station Medintercom page!
Examination methods
To establish an accurate diagnosis and determine the cause of the pathology, you will need an examination, including:
- Laboratory tests of stool, urine and blood;
- ECG;
- X-ray studies;
- Ultrasound diagnostics of internal organs;
- Magnetic resonance or computed tomography.
The specialist will definitely conduct a differential diagnosis with a pre-infarction or infarction condition.
4.Treatment
Of course, it would be wrong to talk about the treatment of pain in the left hypochondrium itself, or, even more so, to give some “general approaches” to their treatment. Modern medicine strictly follows the etiopathogenetic principle: at all costs, find the cause and, as far as possible, eliminate it (ideally, eliminate it completely). Considering the special importance of the left hypochondrium zone, the examination should be as thorough as possible, even if it takes a lot of time and requires significant costs, and its results should give, as far as possible, complete, evidence-based, comprehensive answers about the nature and localization of the pathology, probable prognosis options and the most effective methods of treatment ad hoc (Latin for “for a given case”). A common, fully justified and advisable practice is the above-mentioned redirection of the patient to a specialized specialist: it is wiser to entrust the treatment of the stomach to a gastroenterologist, and the lungs to a pulmonologist; and if the initial contact was made to the wrong address, or the reason could not be determined “on the fly,” this does not mean that “doctors are playing tricks on each other” or “grabbing money for examinations.”
In conclusion, we emphasize once again: the causes of pain in the left hypochondrium, as well as the pain itself, are very diverse, but this is always a reason to visit a doctor. And if you are not sure which one, i.e. If you don’t know what exactly hurts—for example, you’ve never had pain before—it’s best to start by consulting a therapist as the most universal of all doctors.
Preventive measures
To prevent problems with the functioning of the gastrointestinal tract, it is important to adhere to a special diet - eat small portions, but often, and avoid overeating. The daily diet should consist of vegetables, fruits, dietary meats and fish, and cereals. You should avoid fried, fatty and smoked foods.
Disease prevention also involves leading a healthy lifestyle. You need to move a lot and play sports. Preventive examinations with a therapist and other highly specialized specialists will help prevent the development of serious pathological conditions. You need to visit doctors and get tested annually, regardless of how you feel.
Osteochondrosis
Currently, this is the most common spinal disease. During its development, degenerative-dystrophic changes in bone and cartilage tissue occur. According to statistics, about 90% of the world's population suffers from osteochondrosis.
The main reasons for the development of the disease:
- improper formation of the spine during intrauterine development;
- hereditary predisposition;
- the natural aging process of the body;
- disturbance of phosphorus and calcium metabolism;
- unbalanced diet;
- inactive lifestyle or, on the contrary, high-intensity physical activity;
- vibrations that are long-lasting or regular (for example, when driving);
- excess body weight;
- smoking;
- various types of injuries;
- weakness of muscle tissue in the back;
- scoliosis;
- flat feet;
- infectious diseases;
- constantly being in a state of stress;
- living in unfavorable environmental conditions;
- wearing uncomfortable shoes, including high-heeled models;
- pregnancy.
If, when you inhale, there is a stabbing sensation in the left side under the ribs, this is considered a symptom of thoracic osteochondrosis. In addition, a person may experience a feeling of numbness in the area of the heart and stomach. Often the pain radiates to the left shoulder blade or shoulder. The patient also experiences rapid onset of fatigue even with minimal mental and physical exertion.
In most cases, the treatment regimen for osteochondrosis includes the following points: medication, physical therapy, physiotherapy, massage, traction, kinesiotaping, diet.
Rumbling and transfusion in the left side
Hello, I hope for your help! A year and a half ago, I developed excessive intestinal bloating, accompanied by gurgling and rumbling in the left side. After visiting a doctor, I was prescribed: lactofiltrum, dicetel and metronidazole. After a course of treatment, things get better for a while and then everything starts again. Now for the fourth day, gases have been accumulating, especially at night, I wake up from the fact that the intestines are swollen, but only on the left side, when pressed, it rumbles and gurgles, after defecation the day is normal, and in the evening it starts again. It gets better after the gas passes. During the day I constantly burp. Blood tests are normal except for slightly increased bilirubin and ALT, ultrasound showed everything was normal except for the inflection of the bile duct. Please tell me what this could be and how to treat it. Thank you in advance!
Related and recommended questions
11 answers
Hello! Your complaints are caused by disturbances in the functioning of the pancreas and biliary system; there may also be intestinal dysbiosis. You need to undergo comprehensive treatment from your gastroenterologist, who will also select an individual diet for you.
Hello, my stomach has been rumbling and belching for a year now. I was diagnosed with IBS, took a bunch of pills, nothing. Now I'm taking colofort. It seems to help a little. But I was also diagnosed with chronic gastritis, I have a sour mouth, and sometimes heartburn. It also rumbles when I lie down on my left side and during PMS it rumbles below. What could it be? IBS or gastritis?
This is what they put on the FGDS. Nothing has helped the forest for over a year now. I am prescribed colofort, neobutin, etc. Doesn't help me. Perhaps it is not the symptom that needs to be treated, but the disease? Could it be due to the diagnosis of FGDS?
Considering FGDS, it is necessary to deal with bile reflux. Diet 5, it is advisable to eat frequently and in small portions so that bile is secreted correctly. Phosphalugel 3-4r
Source
Rumbling and transfusion in the left side
Hello, I hope for your help! A year and a half ago, I developed excessive intestinal bloating, accompanied by gurgling and rumbling in the left side. After visiting a doctor, I was prescribed: lactofiltrum, dicetel and metronidazole. After a course of treatment, things get better for a while and then everything starts again. Now for the fourth day, gases have been accumulating, especially at night, I wake up from the fact that the intestines are swollen, but only on the left side, when pressed, it rumbles and gurgles, after defecation the day is normal, and in the evening it starts again. It gets better after the gas passes. During the day I constantly burp. Blood tests are normal except for slightly increased bilirubin and ALT, ultrasound showed everything was normal except for the inflection of the bile duct. Please tell me what this could be and how to treat it. Thank you in advance!
Related and recommended questions
11 answers
Hello! Your complaints are caused by disturbances in the functioning of the pancreas and biliary system; there may also be intestinal dysbiosis. You need to undergo comprehensive treatment from your gastroenterologist, who will also select an individual diet for you.