Zometa, 1 piece, 5 ml, 4 mg/5 ml, concentrate for solution for infusion
Use for liver dysfunction.
Since there are limited clinical data on the use of the drug in patients with severe liver failure, it is not possible to make specific recommendations for this category of patients.
Use for renal dysfunction.
When deciding on the use of Zometa in patients with hypercalcemia caused by a malignant tumor, against the background of impaired renal function, it is necessary to assess the patient’s condition and conclude whether the potential benefit of administering the drug outweighs the possible risk.
Before each administration of Zometa, the serum creatinine concentration should be determined. At the beginning of treatment with the drug in patients with bone metastases and with mild to moderate renal dysfunction, it is recommended to use Zometa in reduced doses. In patients who develop renal impairment during Zometa therapy, treatment with the drug can be continued only after the creatinine concentration returns to values that are within 10% of the initial value.
Considering the possibility of renal dysfunction when using bisphosphonates, incl. Zometa, as well as due to the lack of comprehensive data on the clinical safety of the drug in patients with severely impaired renal function (serum creatinine concentration ≥400 µmol/l or ≥4.5 mg/dl in patients with hypercalcemia caused by a malignant tumor and ≥265 µmol /l or ≥3.0 mg/dl - in patients with malignant tumors with bone metastases) and the presence of very limited pharmacokinetic data in patients with initial severe renal impairment (Cl creatinine ≤30 ml/min), the use of Zometa in this population patients is not recommended.
Before infusion, ensure that the patient is adequately hydrated. If necessary, it is recommended to administer saline before, in parallel or after the infusion of Zometa. Overhydration of the patient should be avoided due to the risk of cardiovascular complications.
After administration of Zometa, constant monitoring of the concentrations of calcium, phosphorus, magnesium and creatinine in the blood serum is necessary. If hypocalcemia, hypophosphatemia or hypomagnesemia develops, short-term additional administration of the corresponding substances may be necessary. Patients with untreated hypercalcemia usually have impaired renal function, so careful monitoring of renal function in this category of patients is necessary.
When deciding whether to treat patients with bone metastases with Zometa in order to reduce the risk of pathological fractures, spinal cord compression, tumor-related hypercalcemia, and reduce the need for radiation therapy or bone surgery, it should be taken into account that the therapeutic effect occurs after 2 –3 months after starting treatment with Zometa.
There are isolated reports of renal dysfunction associated with the use of bisphosphonates. Risk factors for such complications include dehydration, previous renal failure, repeated administration of Zometa or other bisphosphonates, as well as the use of nephrotoxic drugs, and too rapid administration of the drug. Despite the fact that the risk of the above-described complications is reduced if Zometa is administered at a dose of 4 mg for at least 15 minutes, the possibility of impaired renal function remains.
There have been cases of deterioration in renal function, progression of renal failure and the need for hemodialysis with the first or single use of Zometa.
Increases in serum creatinine concentrations have also been observed in some patients with long-term use of Zometa at recommended doses, although less frequently.
Since there are limited clinical data on the use of the drug in patients with severe liver failure, it is not possible to make specific recommendations for this category of patients.
Cases of osteonecrosis of the jaw have been described in cancer patients during antitumor treatment, including bisphosphonates (including Zometa). Many patients had signs of a local infectious and inflammatory process, including osteomyelitis.
In clinical practice, the development of osteonecrosis of the jaw was most often observed in patients with advanced breast cancer and multiple myeloma, as well as in the presence of dental diseases (including after tooth extraction, periodontal diseases, unsatisfactory fixation of dentures). Known risk factors for osteonecrosis of the jaw are: cancer, cancer-related treatment (including chemotherapy, radiation therapy, corticosteroids), concomitant diseases (including anemia, coagulopathy, infection, pre-existing oral disease).
Before prescribing bisphosphonates, patients with cancer should undergo a dental examination and appropriate preventive procedures, and recommend strict adherence to good oral hygiene.
Dental surgery should be avoided if possible during treatment of these patients. There is no evidence that interrupting bisphosphonate treatment before dental procedures reduces the risk of osteonecrosis of the jaw. The treatment plan for a particular patient should be based on an individual assessment of the risk/benefit ratio.
In clinical practice, rare cases of severe and in some cases disabling pain in bones, joints and muscles have been reported with the use of bisphosphonates, which include zoledronic acid.
These symptoms developed over a period of 1 day to several months from the start of treatment. Symptoms resolved in most patients after treatment was stopped. In several patients, symptoms recurred when therapy was restarted or another bisphosphonate was prescribed.
Zometa contains the same active ingredient as Aklasta - zoledronic acid. Patients receiving Zometa therapy should not receive Aklasta at the same time.
Use in pediatrics.
The effectiveness and safety of Zometa in pediatric practice have not yet been established.
Impact on the ability to drive vehicles and operate machinery
The effect of Zometa on the ability to drive vehicles and operate machinery has not been studied.
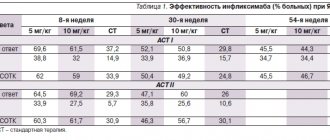
Zometa in the treatment of bone metastases and mineral metabolism disorders in cancer patients
Osteoporosis in patients with malignant neoplasms is characterized by a decrease in bone tissue density and can develop both as a result of age-related changes and as a result of the effect on the bone of biologically active substances produced by the tumor. In cancer patients, the risk of developing osteoporosis is higher than in the general population, since risk factors for the development of osteoporosis are not only concomitant diseases (diabetes, bronchial asthma, anemia, etc.) and some other factors (smoking), but also substances affecting the condition of bone tissue , produced by the tumor, antitumor treatment (systemic chemotherapy, radiation therapy, androgen or estrogen deprivation), concomitant therapy (long-term use of glucocorticoids). Hypercalcemia in patients with malignant neoplasms is divided into local and humoral. In the case of local hypercalcemia, the increase in serum calcium levels is associated with local bone destruction by tumor cells. In the case of humoral hypercalcemia, calcium levels increase under the influence of biologically active substances produced by the tumor: parathyroid hormone-like peptide (90%), other products (growth factors, tumor necrosis factors, interleukins, cytokines). Humoral hypercalcemia in the absence of bone metastases occurs in 10% of patients and is more typical for tumors that secrete biologically active substances, such as lung cancer, thyroid cancer and tumors of a neuroendocrine nature. In bone metastases of breast, lung, prostate cancer, and multiple myeloma, hypercalcemia, according to some authors, is detected in 4–13% of patients [1]. In clinical practice, hyperkacemia is understood as an increase in calcium levels above the upper limit of normal - 2.6 mmol/l; They distinguish a mild degree - a calcium level of 2.6-3.0 mmol/l, a medium - a calcium level of 3.0-3.38 mmol/l, a high - a calcium level above 3.38 mmol/l. Hypercalcemia leads to polyuria and gastrointestinal disorders, progressive dehydration and a decrease in glomerular filtration rate. As a result, the reabsorption of calcium in the kidneys increases, systemic hypercalcemia worsens and creates a pathological “vicious circle”. Symptoms of hypercalcemia vary depending on serum calcium levels and the patient's condition, ranging from dry mouth, thirst, polyuria, constipation, nausea, vomiting to renal failure and confusion. Hypercalcemia with serum calcium levels above 3.0–3.2 mmol/l is a condition that poses a real threat to the lives of patients and requires intensive fluid therapy. According to nephrologists, treatment of patients with moderate and high degrees of hypercalcemia should begin with infusion therapy under the control of general condition, serum electrolyte levels and diuresis. Bone metastases Throughout a person’s life, constant bone formation occurs; an important role in this process is played by the activity of osteoclasts, which resorb bone tissue, and osteoblasts, which contribute to its formation. In the process of metastasis through blood vessels, tumor cells penetrate into bone tissue. In the formation of bone metastasis, the determining events are the colonization of tumor cells in the bone, the influence of tumor cells on bone marrow cells with the subsequent “displacement” of normal cells, disruption of the relationship between osteoclasts and osteoblasts, with the subsequent “uncoupling” of their work - under the influence of substances secreted by tumor cells (growth factors, tumor necrosis factors, interleukins, cytokines, parathyroid hormone-like peptide, etc.). Depending on the pathogenesis, bone metastases are divided into lytic, blastic and mixed. Activation of osteoclasts leads to destruction of bone structure (osteolysis) and the development of lytic metastases; this type of lesion is characteristic, for example, of breast cancer and multiple myeloma. On the contrary, activation of osteoblasts leads to pathological bone formation and the development of blastic metastases; this type of lesion is characteristic, for example, of prostate cancer [2,3]. With mixed metastases, activation of both types of cells (both osteoclasts and osteoblasts) is observed. Figure 1 shows a diagram of the interaction between a tumor cell and bone. The main complaints of patients with bone metastases are pain and limited activity. Bone metastases may not be accompanied by clinical manifestations (for example, blastic metastases are often asymptomatic). It has been established that pain in the bones does not depend on the type of tumor, location, number and size of metastatic foci. The pathogenesis of pain in metastases is associated with disruption of the structure and normal anatomy of the bone (microcracks in the bone trabecula, stretching of the periosteum, involvement of nerve endings) and the effect on pain receptors of biologically active substances produced by tumor cells. The diagnosis of metastatic bone lesions is established on the basis of radioisotope studies of skeletal bones and radiological methods (radiography, computed tomography, magnetic resonance imaging). It should be remembered that about 10% of metastases detected by the radioisotope method do not have radiological signs, that is, they are X-ray negative. Currently, most researchers believe that in such cases, only radioisotope data are sufficient to establish a diagnosis. Based on these X-ray examination methods, the type of bone lesion is determined (lytic, mixed, blastic). Additional information is provided by determination of bone markers in serum and urine. Bone markers are elevated in approximately 50% of patients with bone metastases. Markers of osteoclast activity - collagen degradation products (NTX, CTX) and tartrate-resistant alkaline phosphatase (TRACPS), osteoblasts - bone fraction of alkaline phosphatase (CPALP, normally approximately 50% of the total level of alkaline phosphatase in serum), bone matrix proteins: collagen – type 1 procollagen, non-collagen – osteocalcin [4]. Bone markers in clinical practice are used as additional factors for assessing the effectiveness of therapy. To treat bone metastases, the entire arsenal of methods is used: systemic specific antitumor therapy (cytostatics, endocrine therapy drugs), local treatment methods (surgery, radiation therapy), so-called maintenance therapy, including the prescription of bisphosphonates (to suppress bone resorption) and analgesics . Patients with bone metastases may experience complications associated with changes in the bones - so-called skeletal-related events (SRE, skeletal related events). In addition to the standard criteria for assessing the effectiveness of treatment, adopted by practical oncologists, in the case of treatment of bone metastases, the following criteria are also used: frequency and risk of developing SRE, time before development of SRE, time between the first and second SRE [5]. Bone complications (SRE) include the following events: 1) pathological bone fractures, including vertebral compression fractures (with a decrease in vertebral body height of 25% or more between two x-ray examinations); 2) compression of the spinal cord; 3) the appearance or intensification of pain associated with bone metastases; 4) the need for surgical intervention; 5) the need for radiation therapy. In patients with metastatic lesions of the skeletal bones, an average of 4 bone complications per year are observed. Pathological bone fractures occur on average 11 months after the diagnosis of metastatic bone disease. Table 1 presents data on the frequency (in%) of bone complications in patients with various malignant neoplasms. The development of SRE not only reduces the quality of life of patients with bone metastases, often leading to their disability, but also prevents the continuation of specific antitumor treatment, thus negatively affecting the life expectancy of patients with disseminated malignant neoplasms with bone metastases. From an economic point of view, preventing the development of bone complications, reducing their frequency and increasing the time before their development seems obviously more profitable than treating bone complications and social adaptation of patients with complications of bone metastases. Numerous clinical and experimental studies in the field of biology of bone metastases have allowed scientists to develop a new class of drugs called bisphosphonates. Bisphosphonates in their chemical structure are analogues of bone matrix pyrophosphates, which are resistant to the degrading action of enzymes (alkaline phosphatase). Bisphosphonates reduce the activity of osteoclasts, which results in suppression of bone resorption. In addition, a number of studies have shown the ability of bisphosphonates to potentiate the antitumor effect of cytostatics, hormones and radiation therapy [6,7]. The introduction into clinical practice of bisphosphonates, a group of drugs aimed at the specific correction of mineral metabolism disorders and selective action on metastatic bone, has opened up new opportunities for palliative care for cancer patients. There are bisphosphonates for intravenous administration and oral administration: the most commonly prescribed for intravenous administration are Zometa (zoledronic acid) and Bondronate (ibandronic acid), oral drugs are represented by Bonefos (clodronic acid) and tableted Bondronate. Table 2 provides data on the bisphosphonates most commonly used in clinical practice. Zometa® – Zoledronic acid [1-Hydroxy-2(1H-imidazol-1yl) ethylidene]bis[phosphonic acid] is a third generation bisphosphonate. Zometa's unique formula - the molecule contains two nitrogen atoms (other bisphosphonates have one) - makes the drug active not only against areas of bone defects caused by metastases, but also against the tumor cells themselves. Zometa selectively acts on bone metastases: penetrating into bone tissue, it concentrates around osteoclasts and in resorption lacunae, delays the maturation and migration of osteoclasts, causes their apoptosis, reduces the secretion of lysosomal enzymes (except P450), which leads to disruption of the adhesion of tumor cells to bones and the cessation of tumor resorption of bone tissue. Unlike other bisphosphonates, Zometa has the ability to inhibit neovascularization in tumors (antiangiogenic effect) and cause apoptosis of tumor cells. The antitumor effect of Zometa has previously been proven in studies against breast cancer and myeloma cells. In 2007, similar data emerged for prostate and lung cancer cells. A number of clinical studies have shown the potentiating effect of Zometa on the antitumor effect of cytostatics used in tumor chemotherapy. Zometa is available in the form of a concentrate for infusion, 1 bottle contains 4 mg of zoledronic acid - the dose required for a single injection. Before administration, zoledronic acid concentrate is diluted in 100 ml of saline and administered as an intravenous infusion for at least 15 minutes. The prepared but unused solution is stored at a temperature of +4 – +8°C for no more than 24 hours; the solution must be used within 24 hours from the moment of preparation. Adverse events during treatment with Zometa are usually minor and transient. Side effects of Zometa are not fundamentally different in frequency and severity from other intravenous bisphosphonates, that is, they are characteristic of the entire drug group [7]. Data on adverse events and their frequency are presented in Table 3. Increased temperature, muscle and back pain, and flu-like syndrome are more often observed in the first two days after infusion of Zometa, and are easily relieved by taking nonspecific anti-inflammatory drugs. With subsequent administration of Zometa, anti-inflammatory drugs may be prescribed for prophylactic purposes. Zoledronic acid is excreted unchanged through the kidneys; During Zometa therapy, an increase in serum creatinine levels may be observed; in patients with renal failure, a deterioration in renal function may occur. Reducing the infusion time of Zometa (less than 15 minutes) may be more likely to result in renal damage to zoledronate. In patients with underlying renal impairment, Zometa should be prescribed with caution; if creatinine levels increase, Zometa should be temporarily discontinued. Zometa infusions should be resumed when creatinine levels normalize or decrease to baseline (±10%). All patients receiving Zometa should have their serum creatinine levels determined before each infusion and the infusion time should not be reduced. Table 4 provides recommendations for dose adjustment of Zometa in patients with renal failure depending on creatinine levels; Zometa should not be prescribed to patients with creatinine levels less than 30 ml/min. (there is currently no experience in clinical studies of bisphosphonates, including Zometa, in patients in this group). When treated with Zometa, reactions from the gastrointestinal tract (nausea, vomiting) are possible. Local reactions at the injection site, such as redness and swelling, are uncommon. In most cases, nonspecific treatment is required and symptoms subside within 24 to 48 hours. Serious but rare complications of long-term bisphosphonate therapy include osteonecrosis of the jaw (usually the lower jaw). With continuous therapy with Zometa for 12 months, osteonecrosis of the jaw develops with a frequency of up to 1%; the risk of developing a complication increases slightly with long-term continuous treatment. The nature of the complication is not completely clear; risk factors for the development of osteonecrosis of the jaw include: tooth extraction (or other trauma in the oral cavity), poor oral hygiene, exposure to systemic factors (immunosuppression, chemotherapy, bisphosphonates), as well as malignant bone tumors (such as primary and metastatic). The American Dental Society (ADA) together with specialists from the American Society of Clinical Oncologists (ASCO) have developed clinical guidelines for the prevention of osteonecrosis of the jaw. A physician who prescribes bisphosphonates, including Zometa, should examine the patient's oral cavity before prescribing any bisphosphonate (or refer the patient to a dentist), warn the patient about the likelihood of developing such a complication and the need for careful adherence to oral hygiene rules, and should also avoid time of bisphosphonate therapy and invasive dental procedures. In clinical practice, Zometa is widely used both for the treatment of metastatic bone lesions and for the correction of mineral metabolism disorders - hypercalcemia, osteoporosis, in cancer patients. For tumor-associated hypercalcemia, Zometa reduces serum calcium levels and increases its urinary excretion. After administration of Zometa, the calcium level in 88% of patients is normalized by the 10th day, the average time until calcium normalization is 4 days. The average time to relapse (recurrence of serum calcium levels) is 30–40 days. In patients with hypercalcemia of 2–3 degrees of severity and clinical and laboratory signs of dehydration, treatment should begin with intensive infusion therapy: intravenous administration of crystalloid solutions under the control of the patient’s general condition, diuresis, level of electrolytes in the blood serum, treatment with Zometa can be started when the patient’s condition improves (recommendations of the International Society of Nephrology). After administration of Zometa, during the first 1–4 days, a transient decrease in the level of calcium in the blood serum may be observed; calcium supplements (500–1000 mg per day) and vitamin D (400 IU per day) can be prescribed to prevent hypocalcemia. Zometa is the most effective drug of the bisphosphonate group for the treatment of hypercalcemia (Table 5); normalization of calcium levels when prescribed Zometa was observed in the largest number of patients for the maximum (32 days) period of time. It should also be noted that tablet forms of bisphosphonates are much less effective for hypercalcemia [7]. Information on the activity of Zometa and other bisphosphonates is presented in Table 5. Treatment of osteoporosis In recent years, aromatase inhibitors (AIs) have been widely used in the adjuvant treatment of hormone-dependent early breast cancer in postmenopausal women. The ability of IA to reduce the mineral density of bone tissue (BMD - Bone Mineral Density) is well known, which leads to the development of osteoporosis and the threat of fractures. In two parallel randomized studies of the III phase of the Z - Fast and Zo - Fast (Zometa - Femara adjuvant Synergy Trial), the zomete's ability to prevent the development of osteoporosis [8]. Zometha was prescribed for women in postmenopause, which receives therapy with aromatase inhibitors for early breast cancer; When prescribing a zomet of 4 mg 2 times a year for 2 years, against the background of the continuing therapy of aromatase inhibitors, the mineral density of bone tissue increased, by 3.6% - in lumbar vertebrae, by 1.47% - in femoral bones. Registration of this indication is currently taking place in Russia. Zometa also showed its high efficiency in the prevention and treatment of osteoporosis in patients with prostate cancer after androgenic blockade and oncological patients who have long received corticosteroids [9,10]. Metastatic lesions of bones are an indication by which Zometha is prescribed most often. Unlike other representatives of the Bisphosphonat group, Zomet is active not only in cases of lytic and mixed metastases, but also in relation to the blatical foci (Table 2). For the treatment of bone metastases, Zometha is prescribed in the form of intravenous infusion of 4 mg every 3-4 weeks. Recommended by ASCO experts (American Clinical Oncologists) Duration of treatment with zometa is: 2 years for prostate cancer patients with bone metastases, 1 year for patients with breast cancer with metastashes and patients with multiple myeloma, 9 months for patients with metastases In the bones of other solid tumors. In the treatment of metastases in the bone of Zomet, it has an analgesic effect, lengthens the time to the first bone complication, reduces the frequency of bone complications and the risk of their occurrence, lengthens the interval between the first and second bone complications; Thanks to the anti -rezorbative properties and the ability to enhance the effect of antitumor drugs, Zometha increases the duration and improves the quality of life of patients with bone metastases [11,12]. In a number of large international studies, a comparison of the effectiveness of a zoet with other bisphosphonates was compared, and the advantages of the appointment of a zoet were evaluated compared to patients who did not receive the treatment of bisphosphonates. Let us dwell briefly on the results of some studies. In the study of the III phase (Protocol 010), Zometha and Pamidronate were compared at the risk indicator of skeletal complications (SRE) and time to the first skeletal event in patients with breast cancer with metastases in the bone and multiple myeloma. 377 patients received Zometa, Pamidronate - 389 patients. The study showed that the effect of 4 mg of the zoet is the same as 90 mg of Pamidronate, while the advantage of the zoet is obvious by the method of administration (infusion of 15 minutes against 3 -hour infusion of Pamidronate) [4]. With an additional multifactorial analysis of the results of the protocol 010 according to the Anderson - Gill method, it was established that Zometa is 20% more reduces the risk of skeletal complications compared to pamipronate, and in a group of patients with breast cancer receiving hormone therapy - by 30% (p <0.01) [12]. A direct comparison of the zometa with a placebo (protocol 039) was carried out in 643 patients with bone metastases of hormone -resistant cancer of the prostate gland [8]. The advantage of the zoet is shown both in the frequency of SRE complications (33% versus 44%, p = 0.021), and in the number of pathological fractures: 13% in the group for zometa and 22% in the placebo group (p = 0.015). In addition, in the group of the median zometa, time before the first SRE compared to placebo was more than 6 months (488 days against 321 days, p = 0.01). According to the results of this study, Zometha is recommended as a standard for the treatment of bone metastases in patients with hormone -resistant prostate cancer. Table 6 presents the results of protocols 039, 032/Int and NCIC PR 06 for the treatment of bone metastases of hormone -resistant cancer of the prostate gland. In one of them (032/int), treatment was carried out by pamidronate (90 mg every 3 weeks) compared to placebo. In another (NCIC PR 06) a combination of mitoxantron and prednisone with or without intravenous clodronate was compared. An analysis of the results of three studies showed that only Zometa reduces the risk of skeletal complications (SRE). It was established that Zometa reduced the level of markers of osteoclast activity (NTX) in the urine by 70–80%, while Pamidronate is only 50% [8]. When patients with breast cancer, prostate cancer, cancer of the lung Zomet, reduced the amount of SRE by 30% per month, increased the time before the first SRE occurred by 83%, increased by 35% the time between the first and second bone complications. In a number of studies, 3 phases (036/037, 010, 1501, 039, 011) are shown the ability of the zometa to reduce the risk of bone complications: with breast cancer - by 41%, the prostate cancer - by 36%, lung cancer by 32% , kidney cancer - by 58%, bladder cancer - by 18%, other solid tumors - by 31%[11]. In case of kidney cancer with metastatic bone damage, the purpose of the zoet increased the total survival by 131 days (11.5 months against 7.2 months in patients who did not receive Zomet; p = 0.104). Table 7 Summarized data on the activity of the zoom with bone metastases of various malignant tumors [2]. In these studies, it was shown that with bone metastases of prostate cancer, light and multiple myeloma in patients who respond to treatment, the frequency of SRE complications significantly decreases and they come later. In addition, a decrease in mortality indicators associated with damage to the skeleton was noted. An increase in the level of bone markers for metastases in the bone is observed in approximately half of the patients. Recent studies have established a clear relationship between the degree of bone resorption, the risk of skeletal complications and death in bone metastases of breast and prostate cancer [4,13]. The main biochemical marker of the degree of bone resorption is the product of the collagen of type I -type collagen - N - cowlopeptide (NTX). The authors indicate that the biochemical monitoring of NTX in the urine with a high degree of reliability reveals patients with a high risk of complications and death (P <0.001). The most unfavorable group is patients with NTX level? 100 NMOL/MMOL creatinine. A similar relationship is detected between bone resorption and alkaline phosphatase, but NTX is a more sensitive marker. Increasing the level of NTX? 100 NMOL/NMOL CREATININIS RIRE RISK COMPETION is 1.79, the risk of progression is 1.91, death - 2.67. With an increase in the level of bone fraction of alkaline phosphatase, the risk of the development of SRE is 1.87, the risk of progression is 2.01, death - 1.79. Zometha in patients with an increased level of bone markers reduced the risk of bone complications, with an increased level of N -conventor protein (NTX) by 35%, with an increased level of alkaline phosphatase - by 46%. The first messages about the effectiveness of the zometa appeared when prescribing it in the 2nd line to patients with breast cancer after the progression of bone metastases on the 1st line of therapy with other bisphosphonates [14]. The study evaluated the intensity of the pain syndrome, the quality of life and the marker of bone resorption - N - Teleopeptide (NTX). After 8 weeks, a significant decrease in pain syndrome was noted in 41.9% of patients, which correlated with a decrease in the level of NTX in the urine in the same time. The trend towards a decrease in NTX was noted after one week. Thus, a more active bisphosphonat Zomet has had a palliative effect with the ineffectiveness of other drugs. N - Telepeptide in clinical practice can be used as a marker that predicts the effect of therapy with bisphosphonates, and as a criterion for the selection of patients to continue the treatment of bisphosphonates. In a number of studies conducted, the possibility of using bisphosphonates, including zometes, in the adyuvant treatment of breast cancer of the II - III stage, is studied to prevent metastasis to prevent bone and other organs [5]. According to modern ideas, Zometha treatment should be carried out for a long time, indications for the cancellation of the drug can be pronounced toxicity or sharp deterioration of the general condition of the patient, when the continuation of therapy with zometha is impossible or inappropriate. Conclusion Modern possibilities of treating patients with bone metastases of malignant tumors expanded significantly with the introduction of bisphosphonates into the clinical practice. Zometa - intravenous nitrogen -containing bisphosphonate of the third generation is the most effective drug of this group, with proven activity in all types of metastases (lytic, blatical, mixed), hypercalcemia associated with a tumor, osteoporosis. In experimental and clinical studies, the ability of the zoet is the ability to directly suppress the tumor growth in vitro and in vivo, induce apoptosis, and suppress angiogenesis to the tumor. In patients with bone damage, Zometha metastases reduces the frequency of bone complications with multiple myeloma and breast cancer by 54%, with hormone -resistant prostate cancer - by 50%, with lung cancer - by 30%. At the same time, Zometha increases the time before the first SRE occurs by 80%, and the time between the first and the second SRE is 30%. The drug should be prescribed immediately after the detection of bone metastases and used for a long time, if necessary in combination with other types of treatment (chemotherapy, hormone therapy, radiation therapy). The introduction of bone resorption markers (NTX, bone alkaline phosphatase) in the clinical practice of markers, which are reduced or normalized when the clinical effect is achieved, can be used for individual planning of zometa therapy, the prediction of the response to treatment and evaluating the effectiveness of treatment. Currently, clinical studies are ongoing to assess the possibility of using a zoet to prevent the development of metastases in the bone of the early cancer of the mammary, prostate glands and the means of preventing the development of osteopenia during hormonal treatment (aromatase inhibitors, androgen blockade) in these patients. Based on the results of the studies of bisphosphonates, including Zomet, the most active drug of this group is recommended in the USA and European countries, as an obligatory component of complex treatment of metastases in the bone of breast and prostate cancer, light, kidney, multiple myeloma and other substantial tumors , as well as to correct disorders of mineral metabolism in cancer patients: osteoporosis and hypercalcemia associated with a tumor.
References 1. Guise T., “Molecular mechanisms of osteolytic bone metastases. Cancer suppl., june 2000, v.88, no. 12: 2892–2898. 2. Roodman DG “Mechanism of bone metastases” N.Eng.J.Medicine 2004 350: 1655–1664. 3. Harvey MA, L.von Reyn Cream “Biology of bone Metastases: Causes and Consequences.” J. Clin. Breast Cancer, Vol. 7, Suppl. S7–S13, 2007. 4. Coleman RE “The clinical use of bone resorption markers in malignant bone diseases.” Cancer 2002; 94:2521–33. 5. Coleman RE “Clinical features of metastatic bone disease and risk of skeletal morbidity.” Clin.Cancer Res. 2006; 12 (20 suppl.) 6243s–6249s. 6. Coleman RE “Potential use of bisphosphonates in the prevention of metastasis in early–stage breast cancer.” Clin.Breast Cancer; Vol.7; Suppl. 1. s29–s35; 2007. 7. Zometa (zoledronic acid) Injection product label, Nov 2004. Novartis Pharm Corp., NJ. 8. Brufsky A, Bundred N, Coleman K, “An integrated analysis of Zoledronic acid (ZA) for prevention of aromatase inhibitor associated bone loss (AIBL) in postmenopausal women (PMW) with early breast cancer receiving adjuvant letrozole (LET). ” Breast Cancer Res. Treat. 2006; 100: (abs. 107). 9. Saad F, Gleason DM, Murray R et al., “A randomized, placebo–controlled trial of zoledronic acid in patients with hormone–refractory metastatic prostate carcinoma.” J.Nat.Cancer Inst. 94: 1458–1468, 2002. 10. Saad F, Gleason DM, Murray R et al., “Long-term efficacy of zoledronic acid for the prevention of skeletal complications in patients with metastatic hormone–refractory prostate cancer.” J.Nat.Cancer Inst. 96: 879–882, 2004. 11. Rosen LS, Gordon D, Tchekmodyian S et al., “Zoledronic acid versus placebo in the treatment of skeletal metastases in patients with lung cancer and other solid tumors: a phase III, double–blind ,randomized trial.” J Clin Oncol 2003; 21: 3150–3157. 12. Rosen LS, Gordon DH, Dugan et al., “Zolendronic acid is superior to pamidronate for the treatment of bone metastases in breast carcinoma patients with at least one osteolytic lesion.” Cancer 2004; 100: 36–43 13. Braun JE, Thomson C, Ellis S et al., “Bone resorption predicts skeletal complications in metastatic bone disease.” Br J Cancer 2003; 89:2031–7. 14. Clemons MJ, Dranitsaris G, Ooi S. et al., “Phase II trial evaluating the palliative benefit of second–line Zoledronic acid in breast cancer patients with either a skeletal related event of progressive bone metastases despite first–line bisphosphonate therapy.” ” J.of Clin. Oncology 2006, 24: 4895–4900.
Instructions for use ZOMETA
The drug is administered intravenously as an infusion.
Prevention of symptoms associated with bone damage in patients with malignant neoplasms
For adults and elderly patients
The recommended dose of the drug is 4 mg. The concentrate should be diluted in 100 ml of sterile 0.9% sodium chloride solution or 5% glucose solution and administered as an infusion for at least 15 minutes once every 3-4 weeks.
Patients also need to be prescribed calcium supplements orally at a dose of 500 mg and vitamin D at a dose of 400 IU per day.
When starting treatment with Zometa in patients with multiple myeloma or metastatic bone disease due to a solid tumor
it is necessary to determine the content of serum creatinine and creatinine.
to patients with severely impaired renal function (creatinine clearance <30 ml/min)
.
Clinical studies with Zometa have not been conducted
in patients with serum creatinine levels > 265 µmol/L or > 3.0 mg/dL Recommended doses of Zometa for patients with mild or moderate renal impairment (creatinine clearance from 30 to 60 ml/min)
are presented in the table.
| Initial CC (ml/min) | Recommended dose |
| > 60 | 4.0 |
| 50-60 | 3.5 |
| 40-49 | 3.3 |
| 30-39 | 3.0 |
Drug doses were calculated based on a target AUC of 0.66 mg × h/l (CC = 75 ml/min). For patients with impaired renal function, the dose is reduced to a level that achieves an AUC the same as in patients with CC = 75 ml/min.
After initiation of therapy, serum creatinine should be determined before each dose of the drug, and if renal function deteriorates, treatment should be discontinued. In clinical trials, worsening kidney function is defined as follows:
- for patients with normal initial serum creatinine (<1.4 mg/dL or <124 µmol/L) - an increase of 0.5 mg/dL or 44 µmol/L;
- for patients with altered initial serum creatinine levels (>1.4 mg/dL or >124 µmol/L) - an increase of 1 mg/dL or 88 µmol/L.
Treatment with Zometa should be resumed at the same dose as before treatment was interrupted.
Treatment of hypercalcemia associated with malignancy
For adults and elderly patients
The recommended dose for hypercalcemia (albumin-corrected serum calcium ≥ 12 mg/dL or 3 mmol/L) is 4 mg zoledronic acid. The concentrate should be diluted in 100 ml of 0.9% sodium chloride solution or 5% glucose solution and administered as an infusion for at least 15 minutes once every 3-4 weeks. Before administering Zometa, you should assess the state of the body's water balance and make sure that there are no signs of dehydration.
Hypercalcemia associated with malignancy.
Prescribing the drug to patients with
severe renal impairment
is possible only after assessing the risks and benefits of treatment.
clinical experience with the use of the drug in patients with serum creatinine levels > 400 µmol/l or > 4.5 mg/dl
.
Patients with serum levels <400 µmol/L or <4.5 mg/dL
do not require dosage adjustment.
Prevention of symptoms associated with bone tissue damage in patients with malignant neoplasms.
Instructions for preparing reduced doses of Zometa
Take the appropriate volume of liquid concentrate needed:
- 4.4 ml - for a dose of 3.5 mg;
4.1 ml - for a dose of 3.3 mg;
3.8 ml - for a dose of 3.0 mg.
The taken amount of liquid concentrate should be diluted in 100 ml of a sterile 0.9% sodium chloride solution or 5% glucose solution. The dose should be administered as an intravenous infusion over at least 15 minutes.
If the solution is cooled, it should be kept indoors until it reaches room temperature before administration.