The text is for informational purposes only. We strongly urge you not to use diets, resort to any therapeutic menus or fasting without medical supervision. We recommend reading: “Why you can’t go on a diet on your own.”
Nutrition for gastric and duodenal ulcers is a dietary diet aimed at restoring damaged mucous membranes. This is a prerequisite for full treatment and prevention of relapse of the disease.
A stomach ulcer is dangerous because it can lead to the development of serious complications that threaten the patient’s life. The consequences of the pathological process can be: penetration, perforation of the ulcer and bleeding, malignancy and the development of pyloric stenosis. Remember, peptic ulcer is a dangerous diagnosis that requires urgent medical treatment.
To improve the condition, reduce the frequency of relapses, protect the patient from complications and preserve his ability to work, drug therapy (or preventive measures) is usually combined with proper nutrition. Strictly limiting the patient’s diet to “allowed” and “forbidden” foods increases the chances of recovery and accelerates the scarring of ulcers.
Therapy will not bring results if you do not adhere to the correct diet.
Ulcer - what is it?
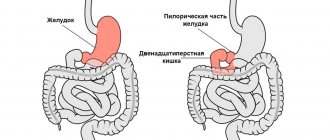
This is a chronic disease accompanied by the formation of defects (ulcers and erosions) on the mucous membrane of the stomach and duodenum. In 70% of cases, the pathology develops in men between the ages of 20 and 40 and is accompanied by frequent relapses, especially in spring and autumn.
Content:
- Ulcer - what is it?
- Diet principles
- Prohibited Products
- Authorized Products
- Medicinal products
- Diets for ulcers
- FAQ
- Menu for a week during an exacerbation of a stomach ulcer
- Conclusion
As a result of exposure to excess hydrochloric acid and enzymes, the lining of the stomach is damaged and an ulcer occurs.
According to statistics, 14% of the world's population suffers from the disease.
The main cause of the disease is an imbalance between aggressive factors and the protective mechanisms of the stomach.
Factors that increase the risk of developing ulcers include smoking, poor diet, frequent stressful situations, abuse of alcohol, carbonated and caffeine-containing drinks, taking anti-inflammatory drugs on a regular basis (such as ibuprofen), Helicobacter infection, eating hot or cold foods that damage the gastrointestinal tract .
Overstrain of the nervous system is accompanied by spasms of blood vessels and muscles in the digestive tract, which leads to impaired circulation in the gastric mucosa and a decrease in its resistance to the aggressive effects of gastric juice.
The prognosis of peptic ulcer disease depends on the localization of the process, the age and gender of the patient, the presence of complications, the characteristics of the clinical course of the pathology, household and professional factors. In advanced, severe stages, complications may develop that require surgical intervention.
Diet principles
What postulates should be followed when preparing a dietary diet?
- Balance. The patient's daily menu should be varied, and its total energy value should be at least 3000 calories.
- Minimum portion size. To avoid overloading the damaged organ, a single meal should not exceed 150 grams (fit in the palms of your hands).
- Avoiding foods that increase gas formation.
- Fractionality. Breaks between meals vary in the range of 2 - 3 hours.
- Minimize salt intake.
- Prohibition on fried, spicy, fatty, smoked products, marinades.
- Increasing the amount of water you drink to 2 liters per day, provided there are no diseases of the urinary system or thyroid gland.
- Prohibition on cold and hot food. Dishes with temperatures up to or above 30 degrees slow down the restoration of epithelial tissue of the stomach and inhibit the function of enzyme secretion.
- Priority is given to gentle food that does not irritate the already inflamed walls of the stomach. Acceptable variations in the heat treatment of dishes: steaming, stewing, boiling, blanching.
- Refusal of foods that stimulate the production of gastric juice.
- The principle of zigzag nutrition. The essence of the method is to train the gastrointestinal tract. It implies that for a short period of time the patient is allowed to consume foods from the prohibited list (within reasonable limits), and then follow the diet menu again. This principle is practiced only at the recovery stage.
- Tracking the time it takes to digest food. Liquid in the body is retained in the stomach for 0.5 - 1.5 hours. Boiled vegetables, baked goods, and cereals take up to 3 hours to digest. And legumes, meat and fish load the digestive tract for 5 hours. At the same time, fruits eaten as part of the main meal, together with other food products, inhibit the absorption of the latter, which leads to food rotting. In this regard, they are recommended to be consumed exclusively in between meals.
- The principle of individuality. When composing your diet, take into account the characteristics of the disease and the body. If there is an individual intolerance to an approved product, it is excluded from the diet.
The main goal of nutrition for ulcers is to normalize the digestion process and accelerate the regeneration of the mucous membrane that lines the stomach.
To improve the patient’s condition, the diet must be followed for at least 1 year after an exacerbation of the pathology. Only in this case is it possible to permanently heal defects in the gastric mucosa and prevent repeated cases of exacerbation of the disease.
Completeness of the diet
On a note
When prescribing a diet, it is extremely important to take into account the nature and stage of the disease, the condition of other organs and systems.
If the diet is used for a long time, it is necessary to take care of the completeness of the diet. And with this, “Diso®” “Nutrimune” will provide invaluable assistance, which compensates for the protein component of the diet without overloading the gastrointestinal tract.
"Diso®" "Nutrimune" helps to compensate for protein deficiency in dietary nutrition and does not put additional stress on the digestive system.
The product is odorless and does not affect the usual taste and consistency of dishes. It can be added to soups, porridges, jelly and other dishes at any stage of preparation.
Prohibited Products
An ulcer is a dangerous disease that requires long-term treatment. For successful therapy and restoration of the patient’s health, food that irritates the gastric mucosa, which takes a long time to digest, increases gas formation, and contains a large amount of salt, is excluded from the patient’s diet.
What should you not eat?
- Sauerkraut cabbage soup, okroshka.
- Smoked products, sausages. The exception is ham in moderate quantities (up to 70 grams per day).
- Rich meat and fish broths, soups based on them.
- Dairy products with acid (tan, ayran, kefir).
- Cucumbers, tomatoes, tomato paste.
- Mushroom dishes.
- Fatty meat, fish, lard, caviar.
- Vegetables with a high fiber content, which make it difficult to digest food: peas, beans, rutabaga, white cabbage, turnips, radishes, radishes.
- Cereal side dishes from corn, wild rice, pearl barley, bran granules, muesli.
- Canned foods, including pates.
- Fatty dairy products: cream, cheeses, condensed milk, whole milk, buttermilk.
- Sour berries and fruits: lemon, orange, lime, gooseberries, figs, grapes, pineapple, tangerine, currants.
- Hard-boiled eggs.
- Products of plant origin that irritate the gastric mucosa: garlic, onion, sorrel, rhubarb.
- Salty, spicy sauces: ketchup, vinegar, mustard, horseradish.
- All carbonated drinks.
- Pastries, rye bread.
- Ice cream and chocolate.
- Alcohol, tea, coffee, cocoa.
- Dried fruits, nuts, apricots.
When processing meat, veins and cartilage are removed from it, which are difficult to digest and burden the digestive tract.
Authorized Products
If you have a peptic ulcer, you should never go hungry, otherwise the stomach begins to digest its walls, which can lead to complications and worsening of the patient’s condition. The ideal interval between meals is 3 hours. During breaks, drink plenty of clean and alkaline water, anti-inflammatory herbal infusions (chamomile, St. John's wort, sage, linden).
List of permitted products:
- Wheat bread (yesterday's).
- Meat soups with secondary broth.
- Biscuit.
- Baked goods made from unleavened (yeast-free) dough filled with lean meat, cottage cheese, fish, and apples.
- Milk and cereal soups.
- Non-fatty fish (boiled or steamed, in foil).
- Main courses from dietary varieties of meat without veins: turkey, beef, chicken, rabbit. It is best to cook by steaming, no frying. The priority is soufflé, meatballs, zrazy, meatballs, cutlets.
- Scrambled eggs.
- Dairy products with a small percentage of fat content: sour cream, yogurt, fermented baked milk, milk, cottage cheese, unleavened cheeses.
- Porridge: oatmeal, semolina, buckwheat, rice. In addition, boiled pasta is beneficial.
- Natural honey, marshmallows, marshmallows, marmalade, jelly, mousses.
- Baked apples and pears, fresh sweet berries and fruits, crushed to puree.
- Vegetable oil (sunflower or unrefined olive), in moderation.
- For dressing dishes, give preference to white milk sauce.
- Drinks allowed are compotes, weakly brewed teas, freshly pressed sweet juices diluted with water by 50%, decoctions of wheat bran and rose hips.
According to medical research, in 90% of cases, stomach ulcers develop due to colonization of the bacterium Helicobacter Pylori. Therefore, to treat acute attacks of the disease, along with antibiotics, products and agents with bactericidal properties (honey, cauliflower, white cabbage, broccoli) are used. If you have a stomach ulcer, any vegetables in your diet should be heat treated so as not to worsen the patient’s condition. It all depends on the individual characteristics of the body: the aggressiveness of the gastric environment.
Medicinal products
Despite the wide range of foods and drinks allowed for consumption, for stomach ulcers, among them there are those that have a healing effect. They support the body during such a critical period and actively fight the bacterium Helicobacter Pylori, which causes ulcers and erosions on the mucous membrane of the stomach and duodenum.
These include:
- Milk. Envelops the walls of the stomach, speeds up the healing process. However, you should drink the drink carefully, as it can cause heartburn and pain.
- Honey. Relieves inflammation and irritation of the gastric mucosa, reduces secretion and neutralizes the effect of hydrochloric acid, relieves pain. In addition, honey increases hemoglobin levels and prevents the development of anemia.
- Freshly squeezed cabbage juice. The medicinal properties of the drink are due to the content of anti-ulcer vitamin U and a stable form of ascorbic acid in the composition. It is the juice that fights pathogenic bacteria Helicobacter Pylori and stimulates scarring of wounds.
- Yogurt. Biologically active bacteria (Bulgarian bacillus, probiotics, lactic acid streptococci) included in the product suppress the activity of harmful microorganisms that cause stomach ulcers. In addition, yogurt contains a bioavailable protein that has a wound-healing effect on the ulcerated surface of the mucous membrane of the damaged organ.
Interestingly, in the laboratories of Guangzhou, China, an acidophilic yogurt starter containing the Helicobacter pylori adhesin gene was invented. This component fights pathogenic flora, which causes exacerbation of stomach ulcers. Today the product is at the development stage with the goal of subsequent introduction into mass production.
Diets for ulcers
For effective treatment of ulcerative pathology - restoration of failure of the digestive process and regeneration of stomach tissue, patients are prescribed diet No. 1a (during an exacerbation for 10 - 20 days, depending on the patient’s condition), then switch to a more advanced version No. 1 or 5 (at the stage of remission ), at the discretion of the attending physician. In any case, to improve your health, the prescribed diet must be strictly followed, without making independent adjustments.
Diet No. 1
Prescribed to patients at the stage of subsiding exacerbation, restoration of the mucous membrane.
The duration of diet No. 1 varies from 3 to 5 months, and the calorie content of the daily diet reaches 3000 calories. This method of eating involves eating boiled or steamed dishes, ground into a homogeneous mass. In this form, products do not have a mechanical effect on the walls of the stomach and are quickly digested without loading the digestive tract. The ratio of B (proteins) : F (fats) : Y (carbohydrates) of the daily menu should correspond to 5 : 1 : 1, and the frequency of meals should occur every 2 – 3 hours.
The diet menu consists of the following products: lean boiled meat, yesterday's baked goods, egg whites, unleavened biscuit, milk soup, pureed cereal porridge, pudding, vegetable puree, small vermicelli, non-sour cottage cheese, sour cream, milk. For dessert, you are allowed to eat boiled or baked sweet fruits (strawberries, pears, apples).
Diet No. 1a
It is prescribed during an exacerbation of peptic ulcer disease, in which bed rest is a prerequisite.
This is a strict subtype of diet No. 1. To soothe the irritated gastric mucosa, foods that increase the production of gastric juice are excluded from the patient’s diet. When using diet No. 1a, food is taken in small portions up to 8 times a day. The ratio B: F: Y is 0.8: 0.8: 2, and the energy value of the diet should not exceed 2000 calories per day.
The consumption of vegetable dishes and bread is prohibited. The basis of the diet is slimy soups and porridges (from rice, semolina, oatmeal), milk, butter (in moderation), lean fish and meat, soft-boiled eggs. You can use berry jelly, fruit soufflé, honey, and jelly in your diet.
Before serving, the dishes are rubbed through a sieve to avoid injury to the walls of the stomach.
Diet No. 5
Designed for proper nutrition of the patient after the symptoms of an exacerbation have been relieved, during the recovery stage. Diet No. 5 creates favorable conditions for the normalization of the digestive tract and implies the consumption of balanced foods. Exceptions: fried foods, fats (refractory), foods rich in essential substances (ginger, garlic, onions), cholesterol-forming food components, mushrooms, radishes, sorrel. The preferred processing method is still: boiling, baking in the oven, steaming.
You can include sweet vegetables and fruits, dried bread, biscuits, cheesecakes, cabbage soups, tongue, aspic, and non-spicy hard cheese in your diet.
For peptic ulcer disease, the use of herbal decoctions based on linden blossom, yarrow, St. John's wort, chamomile, plantain, fennel, marshmallow, and licorice is encouraged.
To coat the stomach and reduce the aggressive effect of gastric juice on the inflamed walls, it is recommended to take 100 milliliters of flax seed jelly daily 30 minutes before meals.
Remember, a diet for ulcers cannot replace the main treatment, but it plays an important role for the human body: it accelerates the healing of eroded areas and prevents complications.
Cooking recipes
The range of permitted and prohibited foods for duodenal ulcers is only at first glance frightening with a large number of changes in the usual diet. Dietary food is a special section of cooking. From a simple set of products it is easy to prepare many tasty and healthy dishes. The main thing in this case is to adhere to the rules for processing and consuming individual ingredients. Here are some delicious and easy recipes:
- Diet pumpkin pudding. To prepare the dish you will need: 150 g pumpkin pulp, 10 g semolina, 10 g honey, 20 g low-fat milk, 140 g apples, 2 eggs. Grind the apples and pumpkin in a blender. Add semolina and milk, bring the mixture to a boil. Add honey and beaten eggs to the prepared mixture. The pudding should be prepared by steaming or in a slow cooker.
- Oatmeal with pumpkin. For 1 cup of rolled oats, prepare 2 cups of skim milk, 1 cup of finely grated pumpkin pulp, butter, two tablespoons of honey. Boil oatmeal with milk until tender. Mix the porridge with pumpkin and leave the mixture for 10-15 minutes, covering the pan with a lid. Add a small amount of butter and also honey.
- Vegetable cream soup. To prepare this dish, prepare the following ingredients: potatoes, carrots, turnips, skim milk, butter. Select the quantity of ingredients at your discretion. Boil all vegetables and chop in a blender. To dilute the mixture to a puree consistency, use vegetable broth and milk. Before eating the soup, place a small piece of butter in the plate.
The duration of a gentle diet depends on the general well-being of the patient. If therapy proceeds without complications, there is a tendency towards recovery, and you can adjust your diet after three to four months. The standard duration of diet therapy is six months.
FAQ
Is it possible to drink lactic acid drinks (kefir, fermented baked milk, yogurt) if you have an ulcer?
During the period of exacerbation of the disease, kefir and fermented baked milk are prohibited. In addition, in the next 5 days after the attack has stopped, you should also refrain from drinking these drinks, so as not to provoke a relapse of the pathology. Subsequently, they can be gradually introduced into the diet, from small doses (from 50 milliliters).
The main condition is that kefir and fermented baked milk should be fresh, moderately sour, with a minimum fat content. Before drinking, drinks are slightly warmed. To speed up the scarring of the ulcer, add a teaspoon of vegetable oil.
Yogurt is a priority food product for stomach diseases, since it contains bifidobacteria that inhibit the effect of Helicobacter Pylori.
Is it possible to eat cucumbers and tomatoes?
If you have a peptic ulcer, you should avoid eating tomatoes, as they reduce the rate of healing of ulcers and increase the acidity of gastric juice. As a last resort, tomato fruits can be eaten after preliminary heat treatment with boiling water, removing the skin. Cucumbers are contraindicated during the period of exacerbation of the disease, however, during the remission stage, it is allowed to include half a vegetable per day in the patient’s diet - without the skin, in crushed form.
Can you eat bananas?
Judgment about this fruit is contradictory. Nutritionists have different opinions regarding the inclusion of bananas in the diet of a patient with damage to the gastric mucosa. Some claim that it reduces the acidity of gastric juice, eliminates pain, and heals ulcers. Others are convinced that bananas are “heavy” foods that burden the digestive tract and take a long time to digest, which is unacceptable for ulcers.
Is it possible to eat cottage cheese and cheese?
Yes, these are valuable foods for a person with an ulcer. Cottage cheese is a coagulated milk protein that supplies iron, retinol, niacin, and B vitamins to the body. There is no whey in it. It is worth choosing cottage cheese with a minimum percentage of fat content. The product can be used to prepare soufflés, mousses, creams, and casseroles.
Cheese is a storehouse of amino acids, calcium, and easily digestible protein. This is an alternative to meat products. When choosing hard cheeses, give preference to a product with low salt and fat content.
Can I have eggs?
Yes, provided they are cooked soft-boiled. Hard-boiled or fried eggs should not be consumed by patients with stomach ulcers. You should avoid taking the product in its raw form, as it increases the risk of contracting salmonellosis.
Egg white is well absorbed by the human body, and the yolk supplies nutrients: calcium, cobalt, iron, phosphorus, vitamins A, , , , .
Can I have watermelon?
No, it contains coarse fiber, which stimulates the production of gastric juice, increases its acidity, and aggravates the course of the disease.
Can I have seeds?
No, they irritate the gastric mucosa and can mechanically injure it, which threatens to aggravate the pathological process. In addition, seeds contain difficult-to-digest fats. As a result, after the nuclei enter the stomach, the patient feels discomfort in the epigastric region, flatulence and pain occur, the acidity level increases, and the ulcerative process worsens.
Can I have garlic?
This product is strictly prohibited; it cannot be consumed in its pure form or as part of prepared dishes, since it has a pungent taste that irritates the gastric mucosa, increases pain, provokes a relapse of the disease (during remission), a sharp deterioration in the patient’s condition (during acute stage).
Can I have coffee?
No, the drink increases the production of hydrochloric acid, which accelerates the development of the disease. During stable remission, natural brewed coffee can be consumed in moderation (up to 50 milliliters at a time), with weak, half-diluted milk.
Can I drink soda?
The most common symptoms of ulcers are belching and heartburn. To relieve discomfort and relieve the first symptoms, many people use soda. However, not every one of them thinks about whether it is safe and what it can lead to?
The substance actually neutralizes hydrochloric acid, which is formed in excess quantities during stomach diseases. It is worth considering the fact that the soda solution brings relief for a short period of time.
Within 0.5 - 1.5 hours, when it leaves the organ, the body will release a new portion of acid in increased quantities. Which will lead to increased stress on the stomach. In addition, when it reacts with soda, carbon dioxide is released, which puts increased pressure on the walls of the stomach. As a result, the risk of perforation increases at the sites where ulcers form.
If you have a stomach ulcer, you should not drink soda in any quantity.
Why should you not drink strong alcoholic drinks?
This is justified by the fact that ethyl alcohol causes inflammation of the stomach walls, slows down the digestion of food, increases the acidity of gastric juice, which as a result aggravates the pathological process, and increases the risk of gastric bleeding. Alcoholic drinks can be consumed up to 100 milliliters every 2-4 days, when there is no exacerbation of the disease. At the same time, the day before you need to eat a hearty meal of gentle food that envelops the stomach. This is the only way to protect the walls of the organ from the aggressive effects of a strong cocktail.
Is it possible to smoke?
Absolutely forbidden. Tobacco smoke has a stimulating effect on the digestive tract; nicotine inhibits the regeneration process, increases existing inflammation, and provokes belching, heartburn, and pain.
According to statistics, smokers die from stomach ulcers 5 times more often than people without a bad habit.
Basic principles
Experts make the following dietary requirements:
- high nutritional value of the diet;
- a balanced diet, which should include proteins, fats, carbohydrates, vitamins, minerals;
- products should not irritate the gastrointestinal mucosa;
- eating food at room temperature;
- avoidance of foods that increase the secretion of gastric juice;
- fractional meals in small portions;
- eating mashed pureed food;
- limiting table salt.
Menu for a week during an exacerbation of a stomach ulcer
To stop an attack, the patient’s diet consists exclusively of pureed boiled dishes without the addition of spices, in a liquid, mushy form. The frequency of meals is 6–7 times a day, the size of one serving is up to 150 grams. Dishes are consumed exclusively warm; they should not be cold or hot.
Day No. 1
- 8.00 – boiled buckwheat;
- 10.30 – puree from boiled vegetables (broccoli and carrots);
- 13.00 – turkey soufflé, slimy oatmeal soup;
- 15.30 – soft-boiled egg;
- 18.00 – boiled rice porridge;
- 20.30 – cottage cheese soufflé.
Day No. 2
- 8.00 – oatmeal, dried biscuit;
- 10.30 – steamed omelette;
- 13.00 – boiled fish fillet, grated beets;
- 15.30 – slimy green buckwheat soup;
- 18.00 – strawberry jelly;
- 20.30 – semolina porridge.
Day No. 3
- 8.00 – rice porridge;
- 10.30 – boiled veal (pureeed), boiled beets;
- 13.00 – cottage cheese casserole;
- 15.30 – soup with barley (slimy);
- 18.00 – oatmeal cooked in water;
- 20.30 – pureed boiled apples (without seeds, peel).
Day No. 4
- 8.00 – boiled rice;
- 10.30 – soft-boiled egg;
- 13.00 – minced chicken meatballs, slimy oatmeal soup;
- 15.30 – buckwheat porridge;
- 18.00 – puree soup from boiled vegetables (carrots, beets, kohlrabi);
- 20.30 – peach mousse.
Day No. 5
- 8.00 – slimy green buckwheat;
- 10.30 – pear jelly, without added sugar;
- 13.00 – oatmeal;
- 15.30 – boiled zucchini, steamed turkey;
- 18.00 – milk jelly;
- 20.30 – sugared rosehip infusion.
Day No. 6
- 8.00 – rice porridge;
- 10.30 – apple and pear puree from boiled fruits without peels or seeds;
- 13.00 – boiled fish (hake), boiled carrots;
- 15.30 – boiled beets, grated;
- 18.00 – barley soup (slimy);
- 20.30 – milk jelly.
Day No. 7
- 8.00 – semolina porridge;
- 10.30 – steamed omelette;
- 13.00 – rabbit soufflé, slimy rice soup;
- 15.30 – vegetable puree from boiled pumpkin and zucchini;
- 18.00 – baked cottage cheese with honey;
- 20.30 – milk jelly.
Subsequently, when the attack of the disease passes, you can expand the menu, introduce new products, move from dietary menu No. 1a to table No. 1 or No. 5.
Reviews and results
This dietary food is prescribed for a long period, since it is balanced, and the diet is significantly expanded compared to Diets No. 1A and 1B . This allows you to eat a varied diet without feeling deprived. Reviews from patients indicate the positive impact of such nutrition on the gastrointestinal tract: pain, belching, heartburn , bitterness in the mouth disappear, and intestinal bloating does not bother you. For some, pain in the pancreas and bowel disorders associated with pancreatitis disappear.
- “...I have had duodenal ulcer for many years. When it was first detected, I was treated well in the hospital, after which there were no exacerbations, and if there were, they were not severe and without the formation of a “new ulcer.” It’s just that in the fall or after nervous stress, sucking pain appears in the stomach area. This is a signal that you need to drink De-nol, Lansoprozole for 2 weeks and switch to proper nutrition. In such cases, I manage without a hospital. I maintain the diet well for 3-4 weeks, and then I switch to regular food, but without spicy, smoked or fried foods. I like steamed cutlets made from different types of meat and poultry - they are not completely tasteless, since my wife adds a little grated onion and dried dill to them (this does not cause pain or other discomfort). I eat soups in water without spices or frying. These are mainly cereal soups with well-cooked or crushed cereals. I eat all the cereals, mashed potatoes, and pureed vegetable supplements. Already in the second week the stomach calms down. In a month of eating this way, I lose a little weight”;
- “... Several years ago there was a perforated ulcer, but it was not very complex, so we operated on it using the endoscopic method. I recovered quickly after this operation, but I had to follow the diet for a long time, and I also took medication for about a month. At first I ate everything pureed for a month, and then I switched to the first table that was not pureed. I adhered to it very strictly for six months, although after a month nothing bothered me, and only 3 scars reminded me of the operation. During these six months, I got used to cooking dishes in a double boiler and a slow cooker, added new recipes to the list, and the food did not seem monotonous and boring. The dietary restrictions affected my weight—I lost 5 kg. I hope to continue to adhere to a healthy diet - the perforation really scared me”;
- “...Frequent exacerbations of ulcers occur once every two years. I think this is due to smoking, irregular meals (and even dry food) and business trips. It is clear that far from home there is no opportunity to eat properly. So it turns out that I periodically end up in the hospital. There they immediately assign Table 1B, and after 2 weeks - the main table for stomach patients.”