What is breathing
It's amazing how differently breathing works in different living creatures! Animals living in water breathe through the surface of their bodies and gills. In insects, air is carried to the tissues by numerous trachea tubes, which tightly cover the body.
Human breathing is actually something fascinating! This is not just the entry of oxygen into the body and the release of carbon dioxide, but a complex process that includes:
- External respiration, that is, the exchange of gases between the environment and the blood.
- Transport of gases by blood.
- Oxidation of organic substances through the resulting oxygen (tissue respiration). As a result of this process, energy is released in the cells, thanks to which the body lives.
And now more about external and tissue respiration.
External breathing.
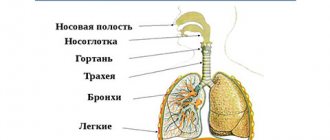
The function of human external respiration is provided by the respiratory system. 98% of gas exchange between the external environment and the blood occurs in the alveoli of the lungs, another 2% of oxygen enters through the skin. Alveoli are vesicles entwined with a network of capillaries. Arranged in clusters. Even though they are tiny, their surface area is approximately 50 times (!) larger than that of a person.
Just imagine how these numerous tiny air-filled bubbles work! More than 700 million alveoli (there are about 375 million in each lung) absorb oxygen delivered to them through the respiratory tract through their respiratory cells. From the alveoli, this gas enters the cells of the capillaries covering them. In exchange, the vessels release carbon dioxide, which enters the air inside the alveoli. This gas exchange occurs passively, due to the difference in oxygen content in the air and blood.
Light, by the way, are light because they are light in weight, because they are filled with air. If you put them in water, they will not drown.
Tissue respiration.
A person breathes not only through his nose and mouth, but also through every living cell of his body. The cell lives due to the fact that oxygen enters it and carbon dioxide is released.
We can say that the only biological function of oxygen is the oxidation (burning, utilization) of fats, proteins, carbohydrates and through this the formation of “combustion” energy necessary for the life of the body.
Athletes are well aware that cellular respiration can be oxygenated (aerobic) and oxygen-free (anaerobic). In the second case, the oxidation of substances occurs with the help of other, reserve oxidized compounds, and not oxygen.
The meaning of breathing
A person lives while he breathes. The length of life depends on the depth and frequency of breathing. If the physiological processes of oxygen supply are disrupted, the body wears out and ages faster.
On average, a person can hold their breath for less than one minute. Although some trained people are able to hold it for up to 5-6 minutes, in particular pearl seekers under water. World record for holding your breath - more than 22 minutes! Respiratory arrest is a critical condition in which death can occur within 5 minutes.
At birth, we breathe correctly, deeply. The diaphragm has a large amplitude, the lungs are filled with good volume. But with age, the diaphragm becomes stiffer, breathing becomes frequent and shallow, and lung capacity decreases. Due to lack of oxygen, the brain functions worse, the heart begins to beat faster and wears out faster.
If there is not enough oxygen, then the decay products of the body's cells do not burn in the lungs as expected, but in the form of toxins are distributed along with the blood throughout the body, poisoning the body. Good breathing is the basis of life and health.
Biophysical mechanisms of respiration
Breathing in a broad sense occurs in every cell of the body, and therefore it is not limited by space. In a narrow sense, the breathing process involves specialized organs and tissue capillaries in which gas exchange occurs.
Ventilation of the lungs occurs due to the energy of contractions of the inspiratory and expiratory muscles. The change of inhalation and exhalation is provided by two muscle groups.
Muscles of inspiration:
- Diaphragm muscle
- External intercostal
- Intercartilaginous parts of the internal intercostal muscles
Muscles of exhalation:
- Abdominal muscles
- Interosseous parts of the internal intercostal muscles
The volume of the lungs changes passively during inhalation and exhalation. This change occurs due to variations in the size of the chest, which entails a decrease or increase in pressure in the lungs. When it is below atmospheric pressure, air enters the lungs; when it is higher, it is pushed out of them. Let's take a closer look at the mechanism.
When you inhale, the volume of the chest cavity increases, the pressure in the pleural fissure (the space between the inner and outer layers of the pleura covering the lung) drops, the lung tissue expands, and the pressure in the lungs decreases to a level below atmospheric. The resulting pressure difference ensures the penetration of air into the lungs through the airways.
When you exhale, the volume of the chest decreases, the pressure in the pleural fissure increases, the lungs compress, and the pressure in them rises to a level above atmospheric. The resulting pressure difference causes air to escape from the lungs.
Which doctor should I contact if I have shortness of breath?
If this clinical manifestation is regular, you should first visit your doctor. He will conduct an examination, collect anamnesis - and, based on the information received, send the patient to an appointment with a specialist in pulmonology, cariology, hematology, neurology or endocrinology.
If a patient has a traumatic injury to the chest, he should consult a traumatologist. In cases where shortness of breath is part of an emergency condition - it appears suddenly and sharply - you should immediately call an ambulance.
Types of breathing: chest, abdominal, mixed
Did you know that when healthy, different people breathe differently? Men, women, older people... Main types of breathing:
- Chest breathing (costal, upper). Characteristic of women. As you inhale, the chest expands and rises as a result of contraction of the intercostal muscles. As you exhale it goes down.
- Abdominal breathing (diaphragmatic, lower). Most often found in men. As you inhale, the diaphragm contracts, causing pressure to increase and the lungs to fill with air. As you exhale, the muscles relax.
- Mixed breathing. Typically for older people. It involves both the chest muscles and the diaphragm.
A change in the type of breathing in women to abdominal breathing, and in men to thoracic breathing, may indicate pathologies.
Treatment and rehabilitation of patients with lung pathology due to coronavirus infection.
08.02.2021 07:19 Author: Slugin Valery Ivanovich. Physiotherapy doctor of the highest qualification category
In order to facilitate the individual selection of rehabilitation methods for patients with lung pathology, separate approaches to solving this problem are listed. Common to all methods of rehabilitation for diseases of the respiratory system is to increase the efficiency of using the gas exchange surface of the lungs and, accordingly, to reduce energy costs for the breathing process itself and for performing respiratory movements. It is recommended that patients with COVID-19 ensure implementation of early mobilization measures. Attention is focused on increasing the duration of the antigravity position until the patient can maintain an upright position. For example, raising the bed to 60° (the lower border of the pillow should be located above the shoulder blade to avoid excessive strain on the head and neck, the second pillow should be located under the popliteal fossa to relax the stomach and lower limbs). Orthostatic procedures should be performed 3 times a day for 30 minutes, with the head positioned in the midline to prevent obstruction of venous outflow and a secondary increase in intracranial and intraocular pressure. It is recommended to start training with short intervals of aerobic exercise. For example, perform a cyclic exercise for 2 minutes, then rest for 1 minute, repeating 4-6 times. You should aim for a total workout duration of 8-12 minutes. Complicating the workout is possible by adding 1 minute to each exercise interval every 3-5 days. Passive mobilization for patients with impaired consciousness and interaction with others consists of performing passive movements in all joints within the physiological range. In each limb segment, 30 repetitions are sufficient, once every 2 hours. Instructing conscious patients on active mobilization is carried out individually and consists of explaining the rules for performing independent movements in all joints in a mode of 10 repetitions 1 time in 2 hours. It should be noted that patients receiving at least 30 minutes of daily exercise, including cyclic bicycle ergometry using bedside robotic equipment, significantly reduce the time spent on mechanical ventilation. Exercises of less than 20 minutes in patients on mechanical ventilation per session and less than 2 times a day have no effect. All rehabilitation measures at the 1st stage are recommended to be carried out taking into account contraindications and to be stopped immediately when “stop signals” appear, namely: temperature above 38 ° C, increased shortness of breath, RR above 30 breaths/min, SpO2 < 93% on oxygen therapy or FiO2 > 50% with non-invasive ventilation, increase in systolic blood pressure above 180 mmHg. or a decrease below 90 mmHg, the appearance of arrhythmia, the development of shock, a decrease in the level of consciousness.
Methods that help improve the absorption of oxygen in the body: - Normalization of the condition of the upper respiratory tract (nasal breathing). - Increasing the duration of contact of oxygen with the lung tissue (slower, deeper breathing). — Increased mobility of the chest and diaphragm (increased muscle elasticity). — Training the “breathing” muscles (strength, coordination...). Increasing air pressure in the lungs (breathing with resistance, hyperbaric chamber) - strengthening the respiratory muscles, especially resisting exhalation. — Practicing individual elements of the act of breathing.
Some features of performing breathing exercises. The breathing rate is regulated and should not be accompanied by dizziness. The depth of inhalation and exhalation may be accompanied by audible faint wheezing and a slight controlled cough. The appearance of a strong, painful, uncontrollable cough indicates an incorrectly selected inhalation/exhalation depth. Drainage positions - help to activate passive areas of the lungs and remove phlegm from them. Vibration of the chest and sound vibration of the lung tissue help improve the function of the lung tissue and remove phlegm. Resistance during inhalation and exhalation - helps to straighten collapsed lung tissue and activate the respiratory muscles.
Voluntary slowing down of respiratory movements leads to a simultaneous deepening of breathing just enough to maintain constant alveolar ventilation of the lungs in a compensatory mode and does not require special efforts. You should focus on a breathing rate of 12 - 15 times min. Breathing is slow, with pauses on inhalation and exhalation (after inhalation there is some long breath holding). This technique is most relevant when treating patients on bed rest. Its advantage is that there is no danger of hyperventilation and therefore the exercise can be carried out for a long time. As the condition improves (improved control of all phases of breathing), dynamic exercises are introduced, which must be accompanied by controlled breathing. Experience from ICU units that are staffed to provide early rehabilitation cautions against performing mobilization maneuvers that specifically provoke coughing. Alternate with dynamic exercises for the arms, movements in the ankle and knee joints. If the patient is not required to intentionally increase or excessively deepen breathing, there will be no unwanted hyperventilation (Smirnov K.M., 1964). J. Vergeret (1981) suggests 30-40 minutes. Before “breathing” gymnastics, perform hardware “breathing” therapy. Pause breathing is a technique for finding a natural rhythm where external influences are completely eliminated. Once you feel your relaxed rhythm, you can compare it in moments of tension: - Pauses after each inhalation and exhalation are the key to effective treatment. — Short pauses during inspiration (no more than 5-7 seconds) provide an inhibitory effect on the nervous system, facilitating the work of the heart (Smirnov K.M., 1964). By changing the depth of inhalation and exhalation and the speed of ventilation in different lobes and segments of the lungs, it is possible to improve the conductivity of the airways and help accelerate the resolution of the pathological process in the lungs. Regulation of breathing “by disturbance”: prevent breathing - breathe through a tube (blowing into a jar of water is more interesting); inflate balloons, blow on fluff, etc. In the acute period, it is not advisable to use forced exhalation and various inflatable toys and balls. Preference should be given to making sounds while exhaling. Fractional breathing by A.A. Streltsov. The basis of the method is inhalation, stretched for 4 counts, and exhalation for 1 (4:1). Gradually, the inhalation lengthens to 18-24-30 counts per 1 exhalation. Fractional breathing can be performed while walking: 2 pairs of steps inhale, 2 “parts” of inhalation; 2 more pairs of steps - the inhalation continues (2 more parts); the next 2 pairs of steps - exhale. The result is breathing for 6 pairs of steps.
Breathing exercises by E.A. Lukyanova. The basis of the training is exhalation, and inhalation is performed involuntarily. Breathing occurs in three phases: 1 - exhalation is performed through slightly pursed lips, 2 - pause (waiting for a “nervous order to inhale”), 3 - inhalation through the nose.
Methodology of V.V. Gnevushev (1972). Start the rehabilitation course by learning “full” breathing: 1. Lengthen the inhalation to 3-4 seconds. with a simultaneous decrease in second volumes. In this case, the abdomen protrudes with simultaneous or subsequent rise of the chest. 2. The duration of exhalation remains involuntary. The chest drops, the stomach retracts. Further improvement of the acquired skills consists of lengthening the inhalation to 10-20 seconds, with a greater decrease in second volumes than at the beginning. At the same time, the patient begins to feel that air “began to flow into the lungs in a thin stream.” As a result, DO (tidal volume) increases and MOD decreases. Autotraining allows you to learn to feel the passage of air along all the paths in the lungs. “Full breathing” - all breathing options (chest, diaphragmatic, mixed). With full breathing, there is a sequential activation of the chest and abdominal muscles. Upper chest breathing is associated with increased activity and arousal. Deep, slow breathing through the belly and lower chest promotes relaxation and calm. The “full breathing” technique begins with mastering “separate” breathing. which includes stages of learning. Training in separate breathing begins with mastering static breathing techniques: nasal, chest, diaphragmatic, and then full. "Chest breathing." Inhalation and exhalation are carried out without the participation of the abdominal muscles - the upper parts of the lungs are filled; The collarbones and upper ribs move upward. To facilitate the correct execution of the exercise (monitoring correct breathing), one hand should be placed on the chest, the other on the stomach. While sitting in IP, with your hands behind your head or on your belt, it is better to practice apical breathing. It should be taken into account that the muscles that lift the upper ribs when inhaling push the cervical vertebrae forward, which is sometimes contraindicated. Medium (thoracic or costal) breathing: the intercostal muscles are involved in filling the middle sections of the lungs, the chest expands to the sides and upwards.
Diaphragmatic breathing. During inhalation and exhalation, the chest should not rise. Lower thoracic breathing (diaphragmatic) is most effective with minimal energy expenditure (Makarova I.N. et al., 2002). It is most convenient to perform the exercise in IP. lying on your back (with your knees slightly bent) or sitting. There are many options for teaching diaphragmatic breathing, but patients learn most easily if they are first asked to “make the stomach like a watermelon (stick out)” and then inhale. Exhalation, accompanied by retraction of the abdomen, usually occurs without problems. - You can start and do the opposite: draw in your stomach and then exhale. When exhaling, the patient must pull in his stomach, and if there is difficulty, the rehabilitator presses his hand on the abdominal muscles. — Usually the lesson is carried out in an individual standing or sitting position. If there is difficulty, diaphragmatic breathing is practiced in IP. lying on your back. — While exhaling, pull your pubis up for 4-10 seconds. — For some patients, the following exercise is more convenient. In I.P. lying on your back, place a weight on your upper abdomen. As you inhale, lift the weight with your stomach. This exercise is important for hypotonic conditions. — In I.P. main stand. During inhalation, the stomach is drawn in, and during exhalation with the “stomach”, the hands are “locked” and raised behind the head. This exercise is good for hyperlordosis. In this case, while exhaling, pull your pelvis up and hold your abdominal muscles tense for 4-10 seconds. To increase the tone of the abdominal muscles, you should lightly pinch the muscles located below the navel. — IP lying on your back, put a weight on your upper abdomen. As you inhale, lift the weight. This exercise is important for hypotension. - IP lying on your back. Breathing through the nose. Bend your knees and try to fill your stomach with air. Then exhale through closed lips. Perform the exercise 10 times during the day. Gradually hold your breath after inhaling. EMG shows an increase in the activity of the abdominal muscles, especially the obliques. The exercise can be performed in IP. sitting, standing, lying on your stomach. Complicating the exercises: - Exhale through tightly compressed lips. Then you can learn to exhale air in portions, gradually increasing the speed and depth of exhalation (“locomotive”). - Perform breathing exercises with changes in the tempo of movement. Static full breathing is a combined sequential execution of “thoracic” and “diaphragmatic” inhalation and exhalation. It is easier to start training in the IP lying on your back with your legs bent. Then the patient learns to take a passive position while sitting in a chair; lotus position; lying on your back. One example of the sequence: inhale with your stomach (push it forward - “lower breathing”), then continue inhaling without interruption and open your chest (“middle breathing”), at the end raise your shoulders up, drawing in your stomach, and finish inhaling (“middle breathing”). upper breathing"). The entire inhalation is performed without jerking in the form of a smooth movement and ends with a pause with breath holding. Exhalation is carried out in the same sequence. Another option is full breathing. In I.P. lying on your back, bend your knees, breathing through your nose (can be performed in IP while sitting, standing, lying on your stomach). Try to “fill your stomach with air,” then exhale through closed lips, trying to “fill your lungs with air.” After 10 minutes of exercise, rest. It is recommended to perform the exercise 10 times during the day. Gradually learn to hold your breath after inhaling. - A deep breath begins by filling the lower parts of the lungs, then the middle part and finally the top. At the beginning of inhalation, the abdomen lowers, freeing the diaphragm, and at the end it retracts, pressing the diaphragm and ensuring the filling of the tops of the lungs. Sequence: “lower breathing” - inhale with your belly (push it forward) -> continue inhaling without interruption - open your chest (“middle breathing”) -> “upper breathing” - raise your shoulders up, pulling in your stomach - take a breath. The entire inhalation is performed without jerking in the form of a smooth movement. The end automatically turns into a breath-holding pause. Exhalation is done in the same order. After training using this method, EMG shows an increase in the activity of the abdominal muscles, especially the obliques. Dynamic full breathing - during the exercise and is consistent with it.
Exhalation muscle training (“expiratory” gymnastics) - exercises for training the exhalation muscles, increasing the mobility of the chest and diaphragm. Promotes stretching of areas of atelectasis, ensuring the depth and completeness of exhalation and voluntary control of the latter. The technique of creating resistance during breathing begins with difficulty exhaling (breathing through slightly pursed lips), and then gradually increasing resistance when inhaling. One of the effective exercises is training cough movements. Some exercises for children. — A soapy washcloth: when you blow through it, “a beard grows.” - Blow on the “spinner”, gradually moving it away from your face. - Blow away (and away from) the ball, fluff, sand. - Put out the candles. - Blow on the fluff (cotton wool) hanging on a thread - so that it stays in the air longer. - Teach how to inflate rubber toys under the obligatory condition - inflate to full volume in fewer breaths. — A game of railway with imitation of the whistle of a steam locomotive, the noise of wheels. - Competition: blow on a tennis ball (ball) on the floor. Who will roll the ball further? — In IP, lying on your back, training the abdominal muscles is “playing with your stomach.” — In IP, lying on your stomach, breathing exercises help strengthen the muscles of the lower chest. In the Vilnius hospital, children play musical wind instruments. Breathing exercises are accompanied by positive emotions.
Gymnastics by A.N. Strelnikova “paradoxical gymnastics”) - creating conditions when inhalation and exhalation are difficult: inhalation must be done with a compressed chest, and exhalation must be done voluntarily. Dynamic breathing exercises (N.M. Zaitsev, co-authors, 2009). Perform all exercises (blocks) 4 times. 1. IP standing, feet shoulder-width apart, hands on the belt: – inhale, lean back slightly; – exhale – lean forward a little, squeezing your shoulders, and lower your arms. 2. IP standing, feet shoulder-width apart, arms along the body: – inhale, raise your arms above your head, leaning back slightly; – exhale, at the same time lean forward, trying to touch the floor with your hands, without bending your knees. 3. IP standing, legs together, hands on the belt: – inhale, at the same time step your left (right) leg forward, transfer the weight of the body to it, tilt your head slightly back, right (left leg on the toe; – exhale, return to IP, head tilt slightly 4. IP standing, legs together, hands on the belt: – while inhaling, turn the torso to the left (right), spreading your arms to the sides at shoulder level; – while exhaling, bend forward and to the left (right), moving your arms back. at the end of the cycle, while inhaling, straighten up, raise your arms up; exhale calmly, while lowering your arms. 5. IP standing, feet shoulder-width apart, arms along the body: - inhale; - exhale slowly, lower your head to your chest, bring your shoulders forward, reach with your arms knees, look down; - inhale - raise your head, straighten your shoulders, spread your arms to the sides at shoulder level, look up; - exhale - IP.
“Sound” breathing exercises. Speech exhalation is always longer than normal exhalation and is equal to “breathing air “+” reserve air.” Pronouncing various sounds is accompanied by tension in various muscle groups. In this case, the muscles of the diaphragm and abdominal press are involved in the act of breathing. According to the strength of the air stream and vibration, all consonant sounds are divided into 3 groups (Epifanov V.A., 2008): 1. Maximum strength - voiceless consonants: P, T, K, F, S. 2. Average tension strength - B, D, D, V, Z. 3. The lowest force of the air stream - M, N, L, R. - During the first 2 lessons, a “cleansing exhalation” is performed: “P-F-F”, “M-M” (closed groan ). Classes are held 1-2 times/day for 5-6 minutes. Then 2 new exercises are added and the duration increases to 7-10 minutes. 2-3 times/day. It is recommended to pronounce these sounds at the end of the lesson. — Vibrating sounds (R, F, Z), hissing and whistling sounds (SH, Shch, S, F, Ch) - reduce spasm of the bronchi and bronchioles, promote fuller and deeper exhalation. - “Sound” (hissing and buzzing) - pronounced quietly, in a whisper, softly, gently. Breathing exercises in most cases reduce expiratory dyspnea. - The sounds “M”, “N” (sonants) can be pronounced with a closed mouth (“closed moan”). Effective for chronic bronchial diseases. A-A-A.. - enhances ventilation of the apices of the lungs. Combines with consonants. Not recommended for concomitant NS diseases. E-I-I.., O-O-O.. - training the respiratory muscles. Combines with consonants. S, F, C, Ch, Sh - calming effect on the vocal cords. SPEECH - after sound gymnastics, as after holding your breath, compensatory tachycardia occurs. LAUGHTER is an extended exhalation with elements of holding the breath. After it, heart rate is restored faster than during tests with breath holding.
Sound gymnastics (N.M. Zaitsev, co-authors, 2009). 1. “Cleansing exhalation” - “pfft” - 4-6 times. 2. “Closed moan” - “mmm” - 3 times and “pfft” - 1 time. 3. “Brrukh” (o, a, e, i) – 1 time each and “pff” – 1 time. 4. “Grruf” (o, a, e, i) – 1 time each and “pff” – 1 time. 5. “Drruh” (o, a, e, i) – 1 time and “pff” – 1 time. 6. “Rrr” - 3 times and “pff” - 1 time
Drainage positions - in order to remove mucus from the respiratory tract as much as possible. “...Systematic postural drainage with vibration massage and periodic courses of antibiotic therapy (especially for acute respiratory diseases) can in many cases achieve significant improvement. At the same time, it is often possible to see the normalization of the bronchological picture in a number of segments that were considered irreversibly affected” (Rachinsky S.V., 1977). The duration of the procedure should be from 10 to 20 minutes, depending on the patient’s condition. The effectiveness of postural drainage increases dramatically when combined with vibration, “forced exhalation,” and massage. During drainage, the instructor lightly taps the relevant area with his fingers; vibration massage - during exhalation. Postural drainages are performed at least 3-4 times a day, usually before meals. The child remains in the drainage position for 3-5 minutes. up to 10-30 min. Change position every 5 minutes. In the acute phase, A.G. Malyavin et al. (2004) postural drainages: used according to the following method: 3-4 hours/day lie on your healthy side with a cushion under your chest, periodically turning over onto your stomach. It is recommended to lie on your back with the affected side unloaded. All this helps prevent the formation of adhesions and improves lung ventilation. In severe cases, during drainage it is necessary to monitor the heart rhythm, because arrhythmia is the main indicator of poor tolerance of bronchial drainage in PV with the head down.
DRAINAGE EXERCISES (M.D. Didur, 2007). Drainage position Massage area. Upper lobe Apical segment Lying on your back, the head end is tilted forward 30 degrees. Upper part of the chest from behind Front IP on the back without a pillow, cushion under the knees Upper third of the chest in front Posterior IP sitting, bending forward, bolster under the stomach Upper third of the chest on the side behind Middle lobe Right and left IP lying on the opposite side, head end down 30 degrees, the affected side is tilted back 20 degrees, knees bent. Upper third of the chest from behind Lower lobe Upper IP lying on the stomach, the pelvis is raised with a pillow. The middle third of the chest is behind the Anterior IP lying on the stomach, the head end is 30 degrees lower, the knees are bent. Lower third of the chest from the side. Basal-lateral IP lying on the stomach, the head end is lowered, the affected side is slightly elevated, the hips are on a bolster. Middle third of the chest from the side. Posterior IP lying on the stomach, the head end is lowered, the pelvis is raised. The lower third of the chest is posterior.
Upper lobe. IP sitting with a slight tilt of the torso forward or backward; lying on your back; lying on the healthy side, head slightly lowered, the leg on the healthy side bent at the knee. Middle lobe (right). IP lying on your back; lying on the healthy side, head slightly lowered, the leg on the healthy side bent at the knee; on the side, head below the level of the legs, the leg end is raised 25-30 cm. Lying across the couch, knees pressed with hands to the chest, head thrown back. Lower lobe. IP lying on your back or stomach; on the healthy side; knee-elbow with maximum relaxation of the shoulder girdle; the foot end of the bed is raised by 40-50 cm. The middle and lower lobes. Lying on the couch on your stomach upside down.
Separate techniques of “drainage gymnastics”. — For infants (can also be used for adults), the “forced exhalation” technique is used in the drainage position. Squeeze the patient’s chest during the exhalation phase (when crying), and also rhythmically - with the child’s resistance, while pronouncing a long sound “A-A-A...”. It is most often used in children who do not like the procedure. — In the drainage position, take a deep (medium or maximum) breath -> pause 2 seconds -> cough 2 times - preferably short, in jerks. In this case, the effect is achieved greater than performing drainages after exercise. In adults, in each position of postural drainage, tapping is used for 2 minutes. and vibration during 5 exhalations. The total duration of the procedure is 45 minutes. (DeCesare JA et al., 1982).
An approximate set of exercises (general regimen). 1. Diaphragmatic breathing 1-1.5 minutes. The pace is slow. Exhale extended through pursed lips. 2. Hands at the shoulders. Raise your elbows up through your sides - inhale, return to IP with pressure on the chest, pressing your head to your chest - exhale. Clear your throat. 306 times. 3. Circular movements in the shoulders back, then forward. 4-5 times in each direction. The pace is average. Breathing is arbitrary and uniform. 4. Hands along the body. Raising your arms to the sides – inhale. Pulling your knees to your chest with your hands – exhale. 5-6 times. The pace is slow. The exhalation is lengthened. 5. Legs bent, support on feet. In IP - inhale, raising the pelvis and lowering it - exhale. 5-6 times. The pace is slow. 6. "Bicycle." 0.5-1 min. The pace is average. Breathing is voluntary. 7. Hands along the body. Raise your straight arms up – inhale; sit down, touching your feet with your hands - exhale. Clear your throat. 5-6 times. The pace is slow. The exhalation is lengthened. 8. Brushes in the “lock”. Stretch your arms forward and turn your body to the right, then to the left. 4-5 times in each direction. The pace is average. Breathing is voluntary. 9. Arms to the sides, fingers clenched into a fist. Circular movements with straight arms forward, then back. 4-5 times in each direction. The pace is fast. Breathing is voluntary. 10. Spread your arms to the sides - inhale, cross your arms over your chest, squeezing it with your hands - exhale. Clear your throat. 5-6 times. The pace is slow. The exhalation is lengthened. 11. Arms to the sides (for stability). Alternate rotation with straight legs 4-5 times in each direction. The pace is average. Breathing is voluntary. 12. Arms to the sides, legs wider than shoulders. Turn the upper body to the side - exhale lengthened, return to IP - inhale. Clear your throat. 4-5 times in each direction. The pace is fast.
B. IP lying on the left (right) side. 13. Raise your right (left) hand up to the side - inhale, lower it, squeezing the chest - exhale. Clear your throat. 4-5 times. The pace is slow. The exhalation is lengthened. 14. Circular rotations of the right (left) hand forward (backward). 4-5 times in each direction. The pace is fast. Breathing is voluntary. 15. Raise your right (left) arm through the side up - inhale; lower it and pull your knee to your chest - exhale. Clear your throat. 5-6 times. The pace is slow. 16. Move your straight arm to the side and turn your upper body to a supine position – inhale; return to IP - exhale, squeezing the chest. Clear your throat. 5-6 times. The pace is average. Exhale through pursed lips.
Food for thought: In the body, oxygen is absorbed in an ionized state: - Coniferous air. — Chizhevsky devices. — Mikulin ionizer. In a cool room, the need for oxygen is lower - the basal metabolism decreases. Drainage positions improve the functioning of healthy areas of the lungs. The initial position of the hand is at the top - the work of the upper - healthy - parts of the lungs is facilitated. Selection of exercises with an emphasis on difficult exhalation: in this case, the passive areas of the lungs are straightened. See methods of exercise therapy for bronchial asthma, but with correction of breath holding (pause): increase the duration of the pause after inhalation, and not the pause after exhalation - the duration of contact between air oxygen and blood increases. In case of previous coronavirus infection, forced breathing techniques are not recommended. Subcutaneous administration of oxygen. MASSAGE. Reflex chest massage, starting from the proximal part. Treat more thoroughly the areas where reflex changes are detected, as well as the areas of the deltoid muscles, sternum and collarbones. (See Some questions of the theory and practice of reflex massage. V.I. Slugin. “Exercise therapy and massage.” 2004. , N 2(11), 20-28.)
Functional control - before and after exercise according to the correspondence of average dynamic blood pressure and pulse. For this purpose, the specific average dynamic pressure is calculated and compared with standard indicators. You can learn more about this on the website “Ariadna/Center/Publications/Assessment of the functional state of the human cardiovascular system at rest and during exercise. New approach. (As amended. 2015) M.A. Slugina, V.I. Slugin. All medical rehabilitation activities should include daily monitoring of temperature, SaO2, SpO2/FiO2, cough, shortness of breath, heart rate, respiratory rate, chest mobility and anterior abdominal wall. 2021
Healthy breathing
Healthy breathing is determined by the number and rhythm of inhalations and exhalations. The breathing rate is about 18 respiratory movements per minute and their frequency is the same. Nature has designed it so that breathing is easy, imperceptible and painless.
If there is not enough oxygen, heavy breathing occurs. This difficulty breathing is called shortness of breath. It occurs during physical exertion, nervous fatigue, chronic fatigue, and also accompanies some diseases.
During examination, therapists determine the state of the respiratory system using vesicular breathing, that is, by noise in the lungs when inhaling. Based on the nature of the noise, it becomes clear whether the respiratory organs are functioning normally or with deviations.
Proper breathing is complete, in which a sufficient amount of oxygen enters the body and toxins are burned. Every cell needs it. Deep breathing has some interesting bonuses:
- Heat production from the process of burning toxins in the lungs. The lungs become a “stove” that heats the entire body and protects against colds.
- Breathing massage performed on the intestines and neighboring internal organs by expanding the diaphragmatic movements. This improves blood flow to the organs, promotes their cleansing and restoration.
Types of shortness of breath
Inspiratory
- characterized
by difficulty in breathing
and occurs with lung pathologies, in particular fibrosis (alveolitis, sarcoidosis, berylliosis), carcinomatosis, valvular pneumothorax, as well as with diaphragm paralysis and ankylosing spondylitis.
Expiratory
- recognized by
difficulty in exhaling
, mainly develops in bronchial asthma and chronic obstructive bronchitis, when the lumen of the bronchi narrows due to phlegm or inflammatory swelling of their walls.
Mixed - both inhalation and exhalation are difficult (possible with severe pneumonia).
When normal breathing is disrupted due to lack of oxygen, all body systems suffer. The provoking factor most often becomes a serious disruption of the functioning of specific organs
Shortness of breath due to diseases of the respiratory system
Occurs in diseases of the bronchi, lungs or respiratory failure due to chest pathology: dysfunction of the diaphragm, pleurisy, kyphoscoliosis.
Signs indicating problems with the respiratory system
- Difficult and long exhalation, at least twice as long as inhalation.
- Tension of the auxiliary muscles during exhalation.
- Protrusion of the neck veins during exhalation, their collapse and retraction of the intercostal spaces during inhalation indicate strong fluctuations in intrathoracic pressure during breathing.
- Dry wheezing when breathing.
- Wet cough - with bronchial asthma, shortness of breath decreases after sputum production, in contrast to heart disease. With them, after a coughing attack, the patient does not breathe easier.
- Severe shortness of breath with severe swelling of the bronchi, increased sputum production and noticeable relief depending on the condition of the respiratory tract.
If a pathology of the respiratory system is suspected, a number of examinations are prescribed, including x-ray diagnostics
Pulmonary causes of changes in breathing also include vascular diseases of the lungs - pulmonary embolism (PE), pulmonary hypertension (increased pressure in the pulmonary artery).
Signs indicating vascular pulmonary diseases
- Dependence on body position - with pulmonary embolism, in addition to tachycardia and chest pain, shortness of breath does not decrease in sitting and lying positions.
- Cyanosis - the skin and mucous membranes acquire a noticeable bluish tint. Develops when there is a significant lack of oxygen in the blood or slow blood flow. Most often combined with severe shortness of breath due to pneumonia and pulmonary embolism.
- Fainting or unilateral swelling of the leg - in combination with even slight shortness of breath often indicates pulmonary embolism (a blood clot entering a vessel) and is considered an extremely alarming symptom requiring rapid hospitalization due to the risk of developing spasm of all pulmonary artery vessels, acute respiratory and heart failure and hypoxia. If medical assistance is not provided in a timely manner, blockage of the vessel will lead to death.
Diseases of the larynx
If inhalation is accompanied by a whistling noise audible from a distance, this is a specific sign of stenosis (narrowing) of the larynx, which makes it difficult for normal air access to the respiratory tract.
Stenosis can develop due to laryngitis, an allergic attack, or when a foreign body enters the respiratory tract. The condition requires an urgent call for emergency medical assistance
Shortness of breath due to heart disease
Among extrapulmonary causes of shortness of breath, a special group includes diseases of the heart and blood vessels (except for pulmonary embolism).
Signs indicating problems with the heart and blood vessels
- Orthopnea - shortness of breath, sharply increasing in a supine position, indicates heart pathology (disturbances in the pulmonary circulation). Shortness of breath at night is considered especially dangerous. In patients with already diagnosed heart or vascular diseases, attacks indicate the development of cardiac asthma - a critical increase in pressure in the left atrium, which often precedes dangerous conditions such as heart attack, cardiac aneurysm, cardiogenic pulmonary edema, acute coronary insufficiency.
- Shortness of breath when walking. The causes of increased breathing during physical activity (running, walking, lifting) are almost always cardiovascular pathologies. The more the disease progresses, the worse even usual sports exercises will be tolerated. In critical illness, symptoms of shortness of breath persist even at rest.
- Edema combined with shortness of breath is a characteristic symptom of heart failure, since due to impaired contractile function of the heart, fluid stagnates in the vessels and tissues.
- Swelling of the neck veins when sitting and difficulty breathing is a typical sign of increased pressure in the right atrium.
Cardiac dyspnea often develops with mitral stenosis, hypertensive crisis, cardiomyopathies, post-infarction cardiosclerosis, coronary heart disease - all these conditions require mandatory treatment
In some cases, it is difficult for a non-specialist to understand what is causing shortness of breath - heart problems or lung pathology. For example, the following symptoms may appear with both coronary heart disease and pulmonary fibrosis:
- long inhalation with noticeable effort (exhalation can be half as long as inhalation);
- rapid breathing movements - a phrase lasting 10 seconds or more cannot be pronounced in one breath, involuntary short breaths are taken;
- during physical activity, even a small one (two or three squats), inhalations become sharply more frequent, and cyanosis of the skin and mucous membranes may appear.
In any situation, there is only one universal recommendation - see a doctor and get examined
Shortness of breath in severe general conditions
A sharp increase in breathing occurs not only with problems with the heart and lungs. Other possible and fairly common causes are severe poisoning, infectious diseases, acidosis, disruption of the respiratory center, allergy attack, hyperventilation syndrome. It is important to notice and recognize them in time.
Specific respiratory disorders during different conditions
- Platypnea - increased breathing when the body is in a vertical position (not only standing, but sometimes sitting), shortness of breath decreases when moving to a horizontal position. Platypnea may indicate a thrombus or tumor in the left atrium, hepatopulmonary syndrome, and also occurs with pathologies that cause prolapse of the diaphragm.
- Sudden and severe disruptions in the respiratory rhythm that occur during intoxication as a result of poisoning.
- Attacks of shortness of breath in combination with urticaria, rhinitis, conjunctivitis are possible with allergic bronchospasm.
- An episodic feeling of incomplete inspiration, a desire to “take in more air” is a common sign of hyperventilation syndrome. This is a psychoneurological pathology in which a specific respiratory rhythm is formed that increases pulmonary ventilation. If shortness of breath is not associated with physical activity, body position, time of day and occurs mainly with severe anxiety or emotional instability, this indicates increased anxiety, including panic attacks.
- Tachypnea - over 20 respiratory movements per minute: superficial, without increasing the depth of inhalation and exhalation, in any condition, including at rest. Along with fever, it develops with pneumonia. At normal or elevated temperatures within 37.5 °C, rapid breathing may indicate acidosis* - a shift in the acid-base balance in the body towards increased acidity.
*Most often, acidosis occurs in diabetic coma, extensive inflammatory processes, high fever, renal failure, intoxication (in particular, poisoning with ethyl alcohol, antifreeze and salicylic acid salts)
Shortness of breath in brain diseases
Shortness of breath is manifested not only by a change in the frequency of respiratory movements, but also by a disruption of the normal respiratory rhythm. The medical name for this phenomenon is respiratory arrhythmia. An attack almost always occurs when the blood supply to the brain or specifically the respiratory center is disrupted, when the central nervous system is affected: stroke, cerebral edema, inflammation of brain tissue, traumatic brain injury of various types.
An exception is an attack of cardiac asthma or severe physical and emotional stress in patients with heart disease. Disordered breathing quickly disappears when the cause is eliminated. In other cases, respiratory arrhythmia signals an urgent visit to a doctor.
Shortness of breath in older people
Respiratory arrhythmia that occurs regularly at rest indicates insufficient blood supply to the brain. In some cases, the breathing rate rises and falls in waves during sleep, with one wave representing 6 to 10 respiratory movements.
Such changes are often observed in cases of severe cerebral atherosclerosis, Pickwickian syndrome, and also as a consequence of a stroke. The causes of shortness of breath in an elderly person are also hypertension, cerebrosclerosis, and aortic insufficiency.
With frequently recurring respiratory arrhythmias, immediate medical attention is needed - problems with blood supply to the brain can lead to a heart attack and damage to the nervous system
External respiration pathologies
The most common dysfunction of external respiration is respiratory failure. It manifests itself in deviations from the norm in the composition of gases filling the arterial blood. Oxygen tension decreases, carbon dioxide tension increases.
What are the types of external respiration disorders:
- Alveolar ventilation disorders. This may be hypoventilation (a decrease in oxygen pressure in the air of the alveoli and the blood flowing from them due to insufficient gas exchange) or hyperventilation (exceeding the volume of ventilation required by the body for gas exchange).
- Violations of ventilation-perfusion relationships. They manifest themselves in uneven alveolar ventilation and deviations in pulmonary blood flow.
- Violation of diffusion, that is, the penetration of gases through the alveolar capillary membrane. This applies mainly to oxygen, since its ability to diffuse is 20 times lower than that of carbon dioxide.
A lack of oxygen supply to the body can be caused by a person’s habits and lifestyle:
- Improper breathing
- Smoking
- Staying in stuffy and unventilated rooms
- Rare trips to fresh air
Features of breathing in children
The breathing of children is different from the breathing of adults. A child's target organs are smaller, making them prone to diseases.
Physiological features of the respiratory system of children:
- Narrow nasal passages and difficulty breathing through the mouth due to a relatively large tongue. At 10-14 years old, nasopharyngeal diseases are common.
- The larynx is longer and narrower than that of an adult, characterized by looseness and the formation of new blood vessels. This causes swelling of the subglottic space (lower part of the larynx).
- Narrow lobar bronchi.
- Poor development of elastic lung tissue, which causes the rapid occurrence of emphysema.
- Tendency to obstruction of the respiratory tract (airway obstruction).
- Tendency to atelectasis (collapse of the lungs due to deficiency/lack of air in the alveoli).
- Tendency to inflammatory processes.
- Soft chest frame, weak muscles.
- Predominance of diaphragmatic breathing.
- Respiratory arrhythmia.
Diseases that cause lack of air
| Diseases | Causes, symptoms |
| Cardiological | Patients suffering from pathological conditions characterized by heart rhythm disturbances complain of shortness of breath and lack of air:
People suffer from it in diseases characterized by a lack of blood supply to the myocardium: angina pectoris, ischemia. The severity of the feeling of lack of air depends on the form and degree of insufficiency: in mild cases it is recorded under minor loads or in stressful situations. The problem is manifested by a lack of oxygen and rapid breathing when doing work or while walking. Other symptoms include cyanosis, chest pain, and swelling of the legs. |
| Pleurisy | A feeling of lack of air develops during inflammatory processes of the pleural layers, accompanied by the appearance of fibrin on their surface or the accumulation of exudate in the cavity. Breathing disorders occur due to severe pain of an acute stabbing or dull pulling nature: the patient tries not to inhale deeply so as not to experience them. The above is accompanied by fever, chills, and cough. |
| Laryngeal stenosis | The most common triggering factor for lack of air is pathologies that provoke obstructions and, as a result, limited oxygen supply. This is typical for acute and chronic stenosis:
|
| Lungs | Inflammatory and diffuse lesions of the lung tissue - initiate deficiency due to the fact that part of the lungs is “switched off” from the breathing process. This happens when:
|
| Foreign bodies in the respiratory tract | Blocking the airways with foreign objects can not only make breathing difficult, but also make it impossible. The person feels suffocated, restless, and takes a position in which he can at least somehow breathe. The symptom develops suddenly after accidentally inhaling an object and is accompanied by coughing, lacrimation, and intense salivation. |
| Pulmonary and pleural neoplasms of malignant etiology | Respiratory disorders are accompanied by a complex of specific symptoms, depending on the location of the neoplasia. Common to all are rapid fatigue, appetite disturbances, and rapid loss of body weight. A similar thing happens with pleural cancer or lung adenocarcinoma, in which malignant cells spread along the walls of the alveoli and bronchioles. |
| Traumatic injuries to the lungs and chest | This type of injury is called thoracic. These include:
|
Features of breathing in old age
In older people, pulmonary ventilation becomes less effective.
- The efficiency of oxygen use decreases by one and a half times.
- The elasticity of the lungs and negative intrathoracic pressure decrease.
- Maximum ventilation of the lungs decreases.
- Dead space (areas of the airways and alveoli in which gas exchange does not occur) increases and alveolar ventilation decreases.
- The distribution of inhaled air becomes uneven.
- Areas appear where there is no air in the alveoli.
- Impaired bronchial obstruction.
- The emergence of various compensatory reactions designed to adapt to breathing problems. For example, during exercise, breathing frequency increases, not depth.
Breathing and exercise
Good breathing is the basis for the success of physical exercise, because its effectiveness is achieved not only through muscle work, but also through increased oxygen production. It helps strengthen muscles and break down fats.
What is proper breathing during physical activity? Deep, with the diaphragm (stomach), not the chest. And it can be mastered. The usual shallow breathing used in everyday life is not suitable: with shallow breaths, not enough oxygen enters the body.
During exercise, a person begins to breathe more often to compensate for the oxygen deficiency. This is wrong, since carbon dioxide remains in the body, which simply does not have time to escape due to short exhalations. And excess carbon dioxide interferes with the absorption of oxygen and even poisons the blood.
Did you know that different sports breathe differently?
- Run. Breathing in a 2:2 rhythm, one inhalation/exhalation for every two steps.
- Power training. Inhale for effort and exhale for relaxation.
- Swimming. Inhale through your mouth, exhale through your nose.
A person can learn to breathe consciously. Such breath control, for example, is an important tool in yogic practice. They have a variety of breathing techniques (pranayama, which means “breath control” in Sanskrit), each of which promises a specific healing effect for the mind and body. They are based on mastering the diaphragmatic (male) type of breathing. Popular types of yogi breathing involve inhaling through the mouth at a certain position of the tongue and exhaling through the nose. We'll talk about the disadvantages of mouth breathing later.
How to treat cough with wheezing?
What to do when you have a cough with wheezing, as mentioned above, depends on the disease that caused this symptom. After a comprehensive examination and diagnosis, the doctor may prescribe several drugs from different drug groups.
Antibiotics
.
Prescribed for diseases caused by pathogenic bacteria. Antibacterial drugs inhibit the vital activity of these microorganisms and cause their death, but should be selected only by a doctor and solely taking into account the sensitivity of microbes to certain drugs. Antihistamines
.
This group of medications is prescribed for cough and other respiratory, skin, or gastrointestinal symptoms caused by allergies. Also, antihistamines can be part of a complex of drugs prescribed for acute respiratory viral infections. Bronchodilators
.
This group of drugs is recommended for coughs with wheezing, which are caused by a narrowing of the lumen of the bronchi. They help normalize breathing, eliminate shortness of breath, and restore the function of removing mucus from the bronchi. This group of drugs has different mechanisms of action, so the specific drug should be selected by the attending physician based on the characteristics of the situation. Mucolytic
.
These agents thin the mucus and prevent it from settling on the walls of the bronchi. This facilitates the removal of both mucus itself and pathogenic microorganisms and toxic products of their vital activity. Doctor MOM® syrup and herbal cough lozenges have pronounced mucolytic and bronchodilator effects, which are based on the action of a complex of medicinal plants. Antipyretics
. They can be recommended for elevated body temperature. An integrated approach to the treatment of cough with wheezing of any origin is important, since it is only one of the symptoms of the disease.