Pneumonia - symptoms and treatment
Which doctor treats the disease?
Pneumonia is treated by a general practitioner or pulmonologist.
When to see a doctor
You should consult a doctor if you have trouble breathing, chest pain, persistent fever (above 38°C) and cough, especially with phlegm.
Indications for the disease
Treatment of patients with CAP is complex and is based on several basic principles:
- prescription of antimicrobial drugs;
- adequate respiratory support if necessary;
- use of non-antibacterial drugs (only if indicated);
- prevention of complications.
Timely detection and treatment of decompensation or exacerbation of concomitant diseases is extremely important, since their presence/severity can radically affect the course of pneumonia.[10]
Antimicrobials
Important! Antibacterial therapy (ABT) can only be prescribed by a doctor, otherwise the risk of drug resistance (resistance) of microorganisms increases sharply.
The main groups of antimicrobial drugs used in the treatment of pneumonia:
- beta-lactam antibiotics (penicillins and cephalosporins);
- macrolides;
- respiratory fluoroquinolones.
In some cases, if there are special indications, drugs from other groups (tetracyclines, aminoglycosides, lincosamides, vancomycin, linezolid) can be used.
For viral pneumonia (usually associated with influenza virus), neuraminidase inhibitors (oseltamivir and zanamivir), which are highly active against influenza A and B viruses, are of greatest importance.
When treating outpatients, preference is given to oral antibiotics (usually in tablet form). When treating patients in a hospital, a stepwise approach is used: they begin with parenteral administration of antibiotics (the intravenous route is preferable), then, as the patient is clinically stabilized, they are transferred to oral administration (tablets).
The duration of antimicrobial therapy for non-severe CAP is determined individually; for severe CAP of unspecified etiology, it lasts at least 10 days. Longer courses of ABT (from 14 to 21 days) are recommended only in case of the development of complications of the disease, the presence of foci of inflammation outside the lung tissue, infection with S.aureus, Legionella spp., non-fermenting microorganisms (P.aeruginosa).
In clinical practice, the decision about the possibility of stopping AMT at the right time is very important. For this purpose, sufficiency criteria have been developed:
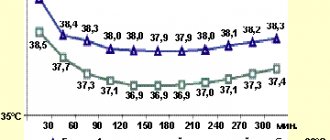
- persistent decrease in body temperature < 37.2ºС for at least 48 hours;
- absence of manifestations of intoxication syndrome;
- normalization of respiratory rate (<20/min);
- absence of purulent sputum;
- decrease in the number of leukocytes in the blood (< 10·109/l), neutrophils (< 80%), young forms (< 6%);
- absence of negative dynamics on the radiograph.[3]
Respiratory support
Acute respiratory failure (ARF) is the leading cause of death in patients with CAP, so adequate respiratory support is an essential component of the treatment of such patients (in conjunction with systemic antibiotic therapy, of course). Respiratory support is indicated for all patients with CAP with PaO2 < 55 mmHg. or SpO2 < 88% (when breathing air).[4]
Oxygen therapy is carried out in case of moderate lack of oxygen in the blood using a simple nasal mask or a mask with a dispensing bag.
Artificial pulmonary ventilation (ALV) is used if, even with oxygen inhalation, the target level of blood oxygen saturation is not achieved.
Indications for mechanical ventilation for ARF due to CAP:
- absolute: respiratory arrest, disturbance of consciousness (stupor, coma), psychomotor agitation, unstable hemodynamics (system blood pressure < 70 mm Hg, heart rate < 50/min);
- relative: respiratory rate >35/min PaO2/FiO2 < 150 mm Hg, increase in PaCO2 > 20% of the initial level, impaired consciousness.
Non-antibacterial therapy
It is represented by three main classes of drugs:
- systemic glucocorticosteroids (GCS);
- intravenous immunoglobulins (IG);
- some immunostimulants.
Glucocorticosteroids
The issue of prescribing GCS is considered primarily in severe CAP, which is complicated by septic shock. GCS help limit the destructive effects of systemic inflammation through various genomic and non-genomic effects.
Immunoglobulins
The use of IG in the treatment of infections complicated by sepsis is based on a variety of effects: from neutralizing bacterial toxins to restoring cell reactivity during the phenomenon of “immune paralysis.”
In the treatment of sepsis, polyclonal IGs are most effective, reducing the relative risk of death compared to placebo. Routine use of intravenous IG in patients with severe CAP complicated by sepsis is inappropriate.
Immunostimulants
Interest in these drugs is associated with their ability to enhance phagocytosis, formation and maturation of neutrophils. However, due to the lack of a convincing evidence base, they are currently practically not used in routine practice.
Contraindications for illness
For pneumonia, self-medication is highly discouraged, especially with the use of antibiotics. Currently, there are many groups of antibacterial drugs; to select adequate therapy, the doctor will ask several questions about the history of the disease, drug intolerance, previous use of antibiotics and what other drugs the patient takes regularly. In the acute period of the disease, it is recommended to refrain from the active use of physiotherapeutic methods of treatment, especially those associated with heating the tissues.
Community-acquired pneumonia
I was advised to contact Farid Firudinovich, as an ENT surgeon, by an ENT doctor from a private clinic in Vidnoye, recommending him as a doctor with God’s hands. I was looking for a doctor for surgery to correct the nasal septum (septoplasty). I suffered for 20 years. At the local clinic and hospital they told me that they didn’t see anything serious on the x-ray of the paranasal sinuses, and that fixing it would only spoil it. But I can’t breathe normally, either on my own or on hormonal sprays, my head hurts constantly. Dryness, runny nose, snoring. Antihistamines didn't help either. Coincidentally, my husband and I did a CT scan of the jaws for the dentist, and there the septum was clearly visible. And she looks terrible. I specifically compared it with my husband’s CT scan (photos in two projections before the operation are attached to the review). I went to a private clinic that I trust. Naturally, with such a curvature and lower shells - just straighten it. As a result, I came to the Sinai clinic for a consultation with F. F. Kurbanov, taking with me a CT scan of the sinuses. And it also shows that due to the curvature of the septum, polyps began to sprout in the right sinus, and there was some kind of swelling in both sinuses (I remember the names). In general, I arrived on time. The doctor told me all this, showed me, explained. A professional who is confident in his knowledge is very important. I felt that I trusted him. It was scary, of course, because I read everything on the Internet over the years. But the doctor is sure, and I am sure. I was afraid that there might be complications, perforation, for example. Everything there is so small and fragile! But I no longer wanted to go through compulsory medical insurance, since they didn’t see the obvious what they could do during the operation - only God knows. They didn’t send me for a CT scan to clarify the diagnosis; they didn’t see the problem visually either. But Farid Firudinovich saw enough even without a CT scan, the program with a CT scan took a long time to load, and he already told me what he saw: the left eardrum, for example, began to deform (retract). Well, the rest/main picture. In general, we discussed the date, passed all the tests and arrived for the operation in two weeks. General anesthesia, a good anesthesiologist (special thanks to him, unfortunately, I forgot his last name) and an assistant, and an hour later I was already in the ward, waking up from sleep with a bandage on my nose. A couple of hours later the doctor came, cheered me up, told me how things were going and what would happen next. We were in touch all the time, which is also important. It was a hard night, it’s hard to sleep when your nose is stuffed with tampons, but it’s all over, after a week the stitches were removed. And I'm finally breathing! On her own, without drops, pills or headaches. My nose still hurts, but these are minor things; every day I feel more and more like a human being. I am writing a month after the operation. And it will only get better! I express my deep gratitude to Farid Firudinovich Kurbanov for his professionalism, experience and human attitude. Thank you! I recommend that anyone who is hesitant to take such a step should not delay. Quality of life is very important. Also, I want to thank the clinic staff for their care!
Liked: Professionalism, experience, human attitude.
I didn’t like it: In the Sinai clinic itself, the general administrative organization is a bit difficult, but the professionalism of the doctors makes up for this drawback.
Lifestyle and Home Remedies
These tips will help you recover faster and reduce the risk of complications:
Take more time to relax . Do not return to school or work until your temperature is normal and your coughing has stopped. Be careful even when you start to feel better: since pneumonia can recur, it is best not to return to daily work until you have fully recovered. In all actions, consult your doctor.
Drink plenty of fluids , especially water.
Take your medications as prescribed by your doctor. Until complete recovery.
Forecast
The mortality rate of patients with severe community-acquired pneumonia hospitalized in the ICU is high and ranges from 22 to 54%. An unfavorable prognosis may be due to the following factors:
- performing mechanical ventilation
- patient age 70 years or older
- bacteremia
- bilateral localization of pneumonia
- need for inotropic support
- sepsis
- P. aeruginosa infection
- ineffectiveness of initial (initial) antibiotic therapy
The fatality rate is high when community-acquired pneumonia is caused by Legionella spp., S. pneumoniae, P. aeruginosa, or Klebsiella pneumoniae.
Laboratory and instrumental diagnostics
Leukopenia below 3x109/l or leukocytosis above 25x109/l is considered an unfavorable prognostic sign of septic complications.
The following changes are possible in the patient's blood test:
- Leukocytosis or leukopenia
- Neutrophil shift in leukocyte formula
- Increasing ESR
- Increased acute phase reactants (CRP, fibrinogen, procalcitonin test). Other changes in the biochemical blood test may indicate decompensation in other organs and systems
Determination of arterial blood gases/pulse oximetry is performed in patients with signs of respiratory failure, massive effusion, and the development of CAP due to chronic obstructive pulmonary disease (COPD). Decrease in PaO2 below 60 mm Hg. Art. is an unfavorable prognostic sign and indicates the need to admit the patient to the intensive care unit (ICU).
A bacterioscopy of the patient's sputum is carried out to identify the pathogen, and the sputum is cultured on nutrient media to determine sensitivity to antibiotics. For severe patients, it is recommended to collect venous blood for blood cultures (2 blood samples from 2 different veins, sample volume - at least 10 ml), PCR study, serological diagnostics to identify respiratory viruses, atypical pathogens of bacterial pneumonia.
X-ray examination of the lungs usually reveals focal infiltrative changes and pleural effusion. Chest CT may be a useful alternative to radiography in a number of situations:
- In the presence of obvious clinical symptoms of pneumonia and no changes on the radiograph
- In cases where, during examination of a patient with suspected pneumonia, atypical changes are revealed (obstructive atelectasis, pulmonary infarction due to pulmonary embolism, lung abscess, etc.)
- Recurrent pneumonia, in which infiltrative changes occur in the same lobe (segment), or prolonged pneumonia, in which the duration of existence of infiltrative changes in the lung tissue exceeds 4 weeks
Fiberoptic bronchoscopy with a quantitative assessment of microbial contamination of the obtained material or other invasive diagnostics (transtracheal aspiration, transthoracic biopsy) is performed if pulmonary tuberculosis is suspected in the absence of a productive cough, as well as with bronchial obstruction by bronchogenic carcinoma or a foreign body
If the patient has pleural effusion and there are conditions for safe pleural puncture, it is necessary to conduct a study of the pleural fluid: counting leukocytes with a leukocyte formula; determination of pH, lactate dehydrogenase activity, protein content; Gram staining of smears; culture to identify aerobes, anaerobes and mycobacteria.
Classification
Today, pneumonia is classified according to the conditions of the onset of the disease:
- community-acquired pneumonia (which a person became infected with not in the hospital, but at home, on the street, etc.)
- hospital/nosocomial
- pneumonia in people with immunodeficiency conditions
- aspiration
Based on severity, community-acquired pneumonia is divided into 3 groups:
- no need for hospitalization (mortality rate 1% to 5%)
— in which hospitalization of patients in a hospital is necessary (mortality rate is 12%)
— in which hospitalization of patients in the ICU is necessary (mortality rate is 40%)
Severe community-acquired pneumonia is pneumonia that has a high mortality rate and requires the patient to be admitted to the ICU. If a person has severe sepsis or septic shock, respiratory failure and the prevalence of pulmonary infiltrates according to an x-ray examination, then we are talking about severe community-acquired pneumonia.