Pneumonia is a disease in which the patient must not only take medications, attend exercise therapy and physiotherapy, but also care, bed rest, room ventilation, and proper nutrition. Many patients with pneumonia are interested in the question of what to eat if they have pneumonia.
Pulmonologists at the therapy clinic, part of the Yusupov Hospital, are developing a special menu for patients. Products included in the patient’s diet help restore strength, remove toxins and speed up recovery.
Danger of pneumonia
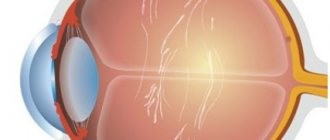
The main danger of pneumonia is that the smallest structural units of the lung tissue, the alveoli, are damaged.
Alveoli - microscopic “bubbles” - are normally filled with air, this is where the main gas exchange occurs: the blood is enriched with oxygen and gets rid of carbon dioxide.
In pneumonia, the alveoli become filled with inflammatory fluid and are unable to perform their basic functions.
If a significant part of the lung tissue is affected:
- the body stops receiving the required amount of oxygen, acute respiratory failure develops, intoxication increases - poisoning with unresolved carbon dioxide and other metabolic products.
Therefore, disruption of the lungs becomes a problem for the whole organism and can lead to the most unfavorable consequences. As doctors say: “Problems with the lungs are never easy.”
Types of physiotherapy for pneumonia
Types of physiotherapy used in the treatment of pneumonia:
- electrophoresis. Using the procedure, the drug is administered through the skin. The action of the current has an irritating effect, improves blood circulation, and enhances metabolic processes. For pneumonia, the drug is administered using electrophoresis in the desired location of the chest, which facilitates the treatment of the disease. To carry out electrophoresis, the following are used: novocaine, heparin, lidase, aminophylline and other drugs;
- UHF. The process of heating tissues using an ultra-high frequency electromagnetic field. The process can take place with continuous or pulsed current. It helps well during acute pneumonia after the condition has stabilized and the body temperature has decreased. Tissue swelling is reduced, sputum secretion is reduced, UHF negatively affects the proliferation of microorganisms;
- inhalation. Vapors containing drugs, ultrasonic exposure allows you to penetrate into the most distant parts of the patient’s respiratory system. Inhalation improves sputum discharge, relieves bronchospasm;
- magnetotherapy. Various methods of influencing body tissues using low or high frequency magnetic fields;
- wave treatment. Centimeter-wave, decimeter-wave, and ultra-high-frequency wave therapy are prescribed. This therapy is carried out in the complex treatment of pneumonia and other inflammatory processes;
- IR irradiation. Prescribed for severe congestion. Infrared irradiation helps improve blood circulation and stimulates phagocytosis;
- therapeutic chest massage. Massage is prescribed in combination with therapeutic treatment and procedures. Therapeutic massage helps restore the elasticity of organ tissue, improves blood circulation, and relieves spasms;
- inductothermy. Exposure of the affected area of the body to high-frequency magnetic radiation. Improves lymph circulation, metabolism, relieves bronchial spasms.
- breathing and therapeutic exercises. With the help of gymnastics, doctors achieve increased immunity, fight weakness, cough, and improve respiratory function.
Cause of pneumonia
The clinical picture of the development of pneumonia is very diverse. It is determined by many factors, such as the type of pathogen, the degree of its activity, the localization of the inflammatory process, the extent of its spread, the state of immunity of the sick person, his age, the presence of concomitant diseases and much more.
Pneumonia can occur as an independent disease (primary) or as a complication of other diseases (secondary). However, the cause of the disease is almost always an infection (bacteria or virus).
Pathogenic microorganisms themselves cannot cause pneumonia; for this there must be provoking factors that weaken the general immunity of the body or the local immunity of the respiratory tract.
List of causes of pneumonia
- Acute respiratory viral infection
- The presence of a chronic inflammatory process in the lungs (chronic bronchitis)
- Hypothermia
- State of prolonged stress
- Smoking
- Presence of chronic diseases
- Injuries
- Surgical interventions
- Elderly age
- Obesity
- Physical inactivity
- Alcohol abuse is also considered a risk factor for pneumonia.
Modern methods of treating pneumonia
An integrated approach to treating the disease is a fundamental aspect of therapy. Its volume depends on the severity of the patient's condition. Treatment includes the prescription of medications, both antibacterial and other drugs aimed at eliminating the cause of pneumonia and preventing complications. Non-drug treatment involves regimen, nutrition, and physical procedures. Severe pneumonia is accompanied by detoxification, hormonal anti-inflammatory and hospital therapy, and resuscitation measures. Medication
When treating pneumonia, the first choice after diagnosis is an antimicrobial drug (AMP).
At the initial stage of the disease, it is impossible to use etiotropic therapy. This means that it is not possible to prescribe a medicine that will act directly as planned on the pathogen, due to the need to identify the microorganism within at least 18-24 hours. Additionally, it is necessary to determine the sensitivity of the pathogen to antibacterial drugs. This analysis will take 5-6 days. Based on the patient’s age and complaints, medical history, severity of inflammation and the presence of complications, concomitant pathologies, the doctor selects one of the recommended regimens (according to clinical protocols). Groups of choice for antibiotic therapy are macrolides, fluoroquinolones and some β-lactams. These drugs can neutralize most bacteria that cause community-acquired pneumonia. Empirical therapy, based on the severity of the disease, can be carried out at home or in a hospital. When prescribing a list of medications at home, the following drugs are chosen: • for patients without concomitant pathologies who have not taken AMPs in the last 3 months
- amoxicillins or macrolides (medicines based on azithromycin, clarithromycin);
• in patients with intercurrent diseases, aggravated by inflammation, who have been taking AMPs for the last 3 months -
protected amoxicillins with clavulanic acid) or macrolides (azithromycin, clarithromycin), or fluoroquinolones (levofloxacin, moxisifloxacin, gemifloxacin).
Antimicrobial drugs for the treatment of pneumonia:
β-lactam antibiotics
• Unprotected amoxicillins (Amoxicillin, Amoxicar, Flemoxin solutab) • Protected amoxicillins (Amoxiclav, Augmentin, Amoclav) • Cefuroxime axetil (Zinnat, Zinacef, Axef, Cefoctam)
Macrolides
• Clarithromycin (Fromilid, Klacid, Klabax) • Roxithromycin (Rulitsin, Rulid, Romik) • Azithromycin (Azibiot, Sumamed, Azimicin)
Fluoroquinolones
(for pulmonary pathology) • Levofloxacin (Tavanic, Lebel, Levoximed) • Moxifloxacin (Moxifur, Avelox, Simoflox ) • Gemifloxacin (Faktiv)
The effectiveness of therapy is assessed after 48-72 hours. If positive dynamics are observed, treatment is continued. If the condition worsens, the doctor changes the main AMP. Important! Frequently changing antibiotics during treatment may cause the development of resistance and reduce the effect of antibiotics in the future. Complicated and severe types of pneumonia are treated only in a hospital setting, and include the injection of drugs into a muscle or into a vein in order to speed up the action of the drugs. Etiotropic
If the desired effect of treatment is not observed, and the causative agent is known, more precise etiotropic therapy is used.
The structure of the causative agents of pneumonia is diverse; microorganisms are classified as follows: 1. Pneumococci
(St. pneumoniae), Staphylococcus aureus (MRSA, MSSA), Pseudomonas aeruginosa (Ps. aeruginosa) - account for up to 60% of all cases of the disease.
2. Intracellular microorganisms
(M. pneumoniae, C. pneumoniae).
Mycoplasmas and chlamydia initiate 20-30% of pneumonia and have an atypical course. 3. Haemophilus influenzae
(H. influenzae), Klebsiella pneumoniae, Legionella pneumoniae in adults cause pneumonia in 5% of cases.
In the structure of pathogens of community-acquired pneumonia, pneumococcus is the leader. Treatment involves the appointment of protected β-lactams, for example, Augmentin, Amoxiclav, Unazin, Sulacillin. The spectrum of their activity includes staphylo- and streptococci, intestinal bacteria, Haemophilus influenzae, and anaerobes. In the absence of resistance, 3rd generation cephalosporins (cefotaxime, ceftriaxone, cefixime, ceftibuten) are used. Alternative auxiliary drugs are also used: macrolides (clarithromycin, azithromycin), fluoroquinolones for the treatment of pulmonary pathology (levofloxacin, moxifloxacin, gemifloxacin). In severe cases, reserve APMs are prescribed: vancomycin, linezolid.
Important!
The use of non-respiratory fluoroquinolones (pefloxacin, ciprofloxacin, norfloxacin, etc.) is considered irrational.
Similar principles of treatment apply to community-acquired pneumonia caused by Haemophilus influenzae or intestinal bacteria. In cases where the causative agent is Staphylococcus aureus, special attention is paid to such a factor as MRSA/MSSA (methicillin-resistant/sensitive staphylococcus). For methicillin-sensitive varieties of MSSA, standard therapy is used, and one of the following drugs is selected: amoxicillin/clavulanate (Augmentin, Amoxiclav), amoxicillin/sulbactam (Unazin, Sulacillin), 3rd generation cephalosporins (cefotaxime, ceftriaxone, cefixime, ceftibuten), lincosamides ( lincomycin, clindamycin). If the form of pneumonia is severe and MRSA is detected, then reserve drugs are used: linezolid, vancomycin. Atypical forms of pneumonia are treated with medications from the group of macrolides or tetracyclines (doxycycline), or respiratory fluoroquinolones. Pathogenetic
Specific pathogenetic therapy is relevant in identifying severe and protracted forms of community-acquired pneumonia in adults. Pathogenetic therapy involves: • immunoreplacement therapy; • detoxification therapy; • treatment of vascular insufficiency; • treatment of hypoxia or effective respiratory support; • correction of perfusion disorders; • treatment of bronchial obstruction; • anti-inflammatory therapy.
In severe cases of community-acquired pneumonia, it is advisable to strengthen protective forces. For this purpose, it can be cured using immunomodulatory drugs (interferons, Levamisole, Zymosan, Diucifon, T-activin, Timalin, Polyoxidonium, Isoprinosine). Immuno-replacement and immunomodulatory therapy is prescribed only on the recommendation of a doctor, since if the patient’s body is severely weakened, this type of drug can worsen the condition. If there is an association of bacteria and virus in the patient’s body, it is advisable to prescribe anti-influenza γ-globulin and antiviral agents (Ribavirin, interferons). Viral influenza pneumonia is treated with Tamiflu. In case of severe staphylococcal inflammation, passive immunization is carried out with serum (hyperimmune antistaphylococcal) or staphylococcal antitoxin. Among other methods of pathogenetic therapy, correction of bronchial obstruction is important. The causative agents of pneumonia contribute to the fact that the patency of the bronchi is significantly reduced due to the narrowing of their lumen, especially in atypical forms of inflammation. Berodual, Pulmicort, Berotec, Salbutamol, Atrovent are prescribed. Drugs with bronchodilator action, i.e. aimed at dilating the bronchi, it is better to administer by inhalation. This increases their efficiency. Of the tablet preparations, Teopek and Theotard are effective. They use agents that dilute sputum: ambroxol, ACC, bromhexine. The combined action agent Joset allows you to dilate the bronchi and facilitate the removal of sputum. Warm alkaline drinks also have a beneficial effect: milk, mineral water. Nonspecific therapy includes vitamins A, C, E, and group B. Adaptogens also have a beneficial effect on the restoration of the body: eleutherococcus, tinctures of lemongrass and ginseng. Detoxification
This type of therapy is carried out to eliminate the toxic effects of bacterial breakdown products on the body.
Specific procedures, such as intravenous drip infusions of saline and glucose, are carried out in severe cases. In most cases, drinking plenty of fluids is effective. Non-drug
Along with treatment with antibacterial drugs, non-drug support of the body is relevant. First of all, patients are recommended to drink plenty of alkaline fluids. You can use warm milk or mineral water. Breathing exercises are effective. They improve respiratory mobility of the chest wall and strengthen the respiratory muscles. Exercise therapy is carried out using various special devices or directly through gymnastics. Exercises, as well as other auxiliary activities, begin no earlier than 3 days after the temperature normalizes. It is possible to use massage (vibration or vacuum). These procedures are also carried out after stable improvement of the condition. Vibration massage is performed using special vibration massagers with a given amplitude. For vacuum massage, cups are used, which, by creating negative pressure, improve local blood circulation and cause reflex irritation and vasodilation. Such procedures facilitate lung drainage and reduce the inflammatory process in the alveolar tissue.
Physiotherapy
Physiotherapy is used as measures whose goal is to restore the drainage capacity of the bronchi, improve sputum discharge and normalize the body's resistance. This auxiliary treatment is prescribed only after the temperature reaches 37°C. Among the procedures, the most effective are: • inhalation of bronchodilators through a nebulizer or ultrasonic inhaler; • local UHF therapy; • local Ural Federal District; • electrophoresis of an antimicrobial drug.
How to eat when you have pneumonia
Nutrition for pneumonia should be aimed at maintaining the body's immune defense and reducing intoxication. All food should be easy to digest, not cause bloating, and contain as little saturated animal fat and cholesterol as possible. Salt intake is limited to 6-8 g per day. The amount of simple sugars is also reduced as much as possible.
It is better to take food warm, in small portions 5-6 times a day, all dishes are steamed or boiled. In the first days of illness, food should be crushed, pureed or given in semi-liquid form.
A special role in the diet for pneumonia is played by foods that are sources of calcium, primarily milk, cottage cheese, and cheese. It is very important that the diet contains a sufficient amount of protein, vitamins and microelements. To reduce intoxication, drinking plenty of fluids (1.5 - 2 liters per day) is recommended.
Treatment and nutrition for pneumonia
Timely antimicrobial therapy remains the main method of treating pneumonia. According to the Clinical Guidelines for the diagnosis, treatment and prevention of severe community-acquired pneumonia in adults, developed in 2014 by the Russian Respiratory Society and the Interregional Association for Clinical Microbiology and Antimicrobial Chemotherapy, treatment begins with parenteral administration of an antibacterial drug. In this option, there is no interaction between drugs and food, and the timing of food intake in relation to the antibacterial drug does not matter. In the future, if the dynamics are positive, when transferring the patient to oral administration of an antibacterial drug, it is necessary to take into account the time of taking the drug in relation to food intake in accordance with the instructions for the drug.
Diet plays an important role in the complex of therapeutic measures.
Features of diet therapy for pneumonia
Therapeutic nutrition should contribute to the rapid resolution of the inflammatory process, detoxification of the body, increasing its immune properties and general reactivity, sparing the organs of the cardiovascular and digestive systems, and preventing possible negative effects of pharmacotherapy.
For moderate pneumonia against the background of febrile fever, the main version of the standard diet (STD) is indicated. Calorie content is reduced, mainly due to a decrease in fat, limiting table salt to 6–8 g, and increasing the calcium content due to dairy products. Reducing sodium and increasing calcium in the diet has an anti-inflammatory effect. To maintain the body’s immune defense, it is necessary to receive a sufficient amount of protein at the rate of 1 g per 1 kg of the patient’s normal body weight, of which at least 60% is of animal origin, primarily from dairy products, eggs and fish, a dry protein composite mixture (with the OVD diet this specialized product is introduced into the medical diet in accordance with the norms of therapeutic nutrition established by Order of the Ministry of Health of the Russian Federation dated June 21, 2013 No. 395n “On approval of norms of therapeutic nutrition”, in the amount of 27 g of the mixture daily).
To reduce intoxication, drinking plenty of fluids (1.5–2 liters or more) with a high content of vitamin C is recommended: sweet and sour fruit juices diluted with water, rosehip decoction, tea with lemon, fruit drinks, compotes. It is imperative to include fermented milk drinks in the diet (including those containing probiotics and prebiotics), which help normalize the state of intestinal microflora, which is significantly affected by systemic antibacterial therapy. The daily diet is divided into 5-6 meals, in small portions; food should be mechanically and chemically gentle.
In case of severe pneumonia, during the first 1–3 days of the disease, liquid food is preferable: tea with lemon, juices, degassed mineral water, rosehip decoction, low-fat meat broth, low-fat fermented milk drinks. At the first signs of improvement and when appetite appears, soups with broth or vegetable broth, soufflé and puree of meat, eggs, boiled fish, cottage cheese, fruit and vegetable purees, baked apples, etc. are introduced into the diet. The energy value of the diet is 1500– 1600 kcal due to a sharp restriction of fats (30–40 g), a moderate reduction in carbohydrates (250 g) and proteins (60 g). The norms of therapeutic nutrition are fulfilled according to the version of the diet with reduced calorie content (low-calorie diet, LDC). The therapeutic diet includes dry protein composite mixtures in the amount of 24 g daily. Next, the diet is built in accordance with the nutritional option for moderate pneumonia.
During the period of mild pneumonia, a diet with an increased content of calcium and vitamins, fermented milk drinks, with the exception of indigestible and very fatty foods is recommended. In addition, with low appetite during the convalescence period, use moderately salty snacks (soaked herring, cheese, ham, caviar, etc.), pickled, pickled and spicy vegetables, spices, tomato and other juices.
author: V.V. Egorova, nutritionist, Federal State Budgetary Institution State Scientific Center "Federal Medical Biophysical Center named after A.I. Burnazyan" FMBA of Russia, doctor of the highest category
Where to begin
In case of mild community-acquired pneumonia, the main version of the standard diet (STD) is prescribed with the enrichment of the diet with a dry protein composite mixture of 27 g/day (for example, when using SBCS "Diso®" "Nutrinor" the patient will receive 10.8 g of protein, which has high biological value) and the inclusion of vitamin-mineral complexes (50–100% of the physiological norm introduced by Order of the Ministry of Health of the Russian Federation dated June 21, 2013 No. 395n “On approval of therapeutic nutrition standards” into the therapeutic nutrition standards).
Individual approach
As with any disease, so with pneumonia, there are general principles of diet therapy, but an individual approach cannot be ruled out.
Acute period
With pneumonia with high fever, the basal metabolism increases, and the human body becomes intoxicated with waste products of microorganisms and tissue decay. The load on the cardiovascular system increases, the functional activity of the digestive organs decreases. This should be taken into account when prescribing therapeutic nutrition.
The intended purpose of diet therapy: unloading interstitial metabolism, influencing the inflammatory process and neuro-vegetative dystonia by sharply limiting sodium chloride, carbohydrates and introducing a sufficient amount of Ca salts and vitamins.
Principles of diet therapy: full provision of the body’s energy and plastic needs; increased immunological reactivity; rapid resolution of educational processes, reduction of intoxication, sparing the organs of the cardiovascular and digestive systems; prevention of possible negative effects of pharmacotherapy.
Want more new information on nutrition issues? Subscribe to the informational and practical magazine “Practical Dietetics”!
SUBSCRIBE
For patients with pneumonia accompanied by high fever, a specialized antiviral desensitizing (alkalinizing) diet is recommended. In this case, depending on the patient’s condition, this diet is represented by four types of diets, compiled on the basis of standard diets (see Table 1), approved by Order of the Ministry of Health of the Russian Federation dated June 21, 2013 No. 395n “On approval of therapeutic nutrition standards.” These diets should include specialized food products, mixtures of dry protein composites and vitamin-mineral complexes, introduced by Order No. 395n into the norms of therapeutic nutrition. Medical nutrition standards are mandatory for all medical organizations in the Russian Federation.
Table 1. Therapeutic nutrition for a patient with pneumonia with high fever
| Type of specialized/standard diet | Based on a standard diet | Proteins, g | Fats, g | Carbohydrates, g | Energy value, kcal |
| First Alkalinizing Diet | NKD | 25 | 30 | 115 | 800–900 |
| Second diet of the alkalizing diet | NKD | 40 | 50 | 120 | 1100 |
| The third diet of the alkalizing diet | NKD | 50 | 70 | 160 | 1500 |
| The fourth ration of the alkalizing diet | ATS | 70 | 85 | 200 | 2000 |
| UBI | 110–120 | 80–90 | 250–350 | 2080–2690 |
So, on the first day of the disease, the patient is on the first and second diets, then until the 10th–12th day of the disease - on the third and fourth diets.
The diet includes a variety of foods, excluding foods with a high content of extractives and sodium chloride. Table salt is sharply limited (up to 3–5 g). Dishes are prepared taking into account mechanical sparing of the gastrointestinal tract. Decoctions of rose hips, wheat bran, fruit and berry and vegetable juices are prescribed. Diet 5-6 times a day. The diet is based on the principle of gradually increasing its nutritional value in the form of four diets.
Highly alkalizing foods include: milk, cucumbers, tomatoes, lettuce, celery, turnips, beets, raisins, fruits, citrus fruits, berries (except lingonberries). Slightly alkalizing foods include potatoes, cabbage, green peas, beans, apples, red currants.
Recovery period
During the recovery period, it is necessary to significantly increase the energy value of the daily diet (2080–2690 kcal), mainly due to the content of proteins (110–120 g), fats (80–90 g) and, to a lesser extent, carbohydrates (250–350 g) - prescribed a diet option with an increased amount of protein (high-protein diet, HPD). Enriching the diet with protein replenishes its losses during tissue breakdown, stimulates reparative processes, the production of antibodies, and prevents leukopenia. The norms of therapeutic nutrition are applied when following a high-protein diet with the inclusion of specialized food products, mixtures of dry protein composites in the volume of 36 g of the mixture (for example, when using SBKS "Diso®" "Nutrinor" - 14.4 g of protein) as part of the therapeutic diet.
An increase in the amount of table salt is allowed (up to 10–12 g); the inclusion in the diet of products that stimulate gastric secretion and exocrine activity of the pancreas (meat and fish broths, sauces, spices, seasonings, juices, etc.) is indicated. The number of meals can be reduced to 4–5 times a day.
Menu for pneumonia
In the first days of illness, as a rule, appetite is greatly reduced or completely absent. You should not force feed a patient. However, fasting is also prohibited - strength is needed to fight the disease.
Drinking for pneumonia
Drinking plenty of fluids during pneumonia is an important component of the diet. This facilitates the release of sputum, prevents dehydration, and relieves intoxication. Therefore, you need to drink at least 1.5-2 liters per day , and even more at high temperatures. The best drinks for this are those that contain vitamins and microelements.
List of healthy drinks
- Tea with lemon
- Tea with milk
- Any fruit juices
- Compotes
- Fruit drinks
- Decoctions
- Alkaline mineral water without gas
- Still mineral water
- Rose hip decoction
- Berry fruit drinks
- Compotes from fresh and dry fruits
Fruit and berry juices
Low-fat fermented milk drinks
The menu must include low-fat fermented milk products. This has a good effect on the state of beneficial intestinal microflora, which especially needs support during antibiotic treatment.
List of useful foods for pneumonia
For pneumonia, the following foods are used in the diet:
- Boiled or steamed lean meat (chicken, rabbit, turkey)
- Boiled lean fish
- Milk, cottage cheese - low fat
- Fermented milk drinks (yogurt, kefir, yogurt)
- Potatoes in any form, except fried
- Cauliflower, broccoli. White cabbage is prohibited!
- Eggs (boiled and scrambled)
- Boiled or stewed vegetables (carrots, peppers, zucchini, pumpkin)
- Fresh vegetables (tomatoes, cucumbers)
- Cereals: oatmeal, buckwheat, rice, semolina
- Fresh fruits and berries (except grapes!)
- Dried fruits: prunes, dried apricots
List of Not Recommended Products
In case of pneumonia, everything that increases the load and irritates the gastrointestinal tract is excluded from the diet:
- Fatty and fried foods
- Legumes
- Canned food
- Semi-finished meat products
- Mushrooms
- Corn porridge
- Confectionery
- Chocolate
- Coffee
- Acute
- Salty
- Pickled products
- Spicy seasonings and sauces
- Mayonnaise
List of products for improvement
- Soups with broth or vegetable broth
- Soufflé and meat puree
- Eggs
- Boiled fish
- Cottage cheese
- Fruit and vegetable purees
Recommended Products
In the future, it is recommended to widely use it in the diet for pneumonia.
- Meat
- Fish
- Dairy dishes
- Egg dishes
- Cereal dishes
- Vegetable dishes
- Fruit dishes
Nutrition for pneumonia in the acute period
The choice of food and dishes during the acute period of pneumonia depends on how long the fever lasts. With pneumonia, patients often have a decreased appetite, so you should choose foods that are easily digestible and quite nutritious.
Nutrition for pneumonia may include:
- broths. The main advantage of broths is the high content of fat-soluble vitamins, proteins and fats. Broths contain a large amount of water, which the body needs during pneumonia to restore water balance. If you have pneumonia, the ingredients for the broth must be chosen with extreme caution. For children, it is recommended to use turkey meat, fresh herbs, onions and carrots. Broths are contraindicated for children under one year of age, as well as for people with diseases of the pancreas, gall bladder and liver;
- vegetables such as bell peppers, tomatoes, cucumbers, lettuce and greens are indicated for patients with pneumonia. If the patient has no desire to eat vegetables, they can be replaced with fruits for a short period;
- cereal dishes The most useful among cereals are oatmeal and buckwheat, which can be consumed in the form of side dishes;
- dairy products. Fermented milk products during antibacterial therapy normalize the activity of the gastrointestinal tract and microflora. The most useful products are: biokefir, ayran, matsoni;
- steamed cutlets, chicken, turkey, white fish. Meat, poultry and fish dishes should be easily digestible. They contain their own proteins, such as immunoglobulins, which increase the body's resistance to fight infection.
When receiving treatment at the Yusupov Hospital Therapy Clinic, a pulmonologist, together with a nutritionist and other specialists, develop a nutrition program for the patient. The daily diet of a patient with pneumonia consists of delicious dishes prepared from fresh products that are rich in vitamins and microelements.
Nutrition for pneumonia during the recovery period is distinguished by a wide variety of products. Food for the patient should be fresh and well prepared. The main principle of the diet for pneumonia is that meals should be small and frequent, this is how food will be absorbed faster and the person will not experience a feeling of heaviness.
The importance of protein in pneumonia
To maintain the body's immune functions, it is very important that a sufficient amount of protein is supplied with food (at least 1 g per 1 kg of body weight). It is equally important that the incoming protein is complete in composition and easy to digest.
Without protein, the processes of healing and restoration of damaged lung tissue are impossible. In addition, protein is necessary for the development of protective components of the immune system, ensuring the fight against infection and a speedy recovery.
Diet therapy for COVID pneumonia.
COVID pneumonia is not like the viral and bacterial pneumonias that we most often encountered in previous years. Bacterial pneumonias are more common, they are caused by bacteria and proceed differently than viral ones. Firstly, they respond well to antibiotics. Second, resolution of bacterial pneumonia usually occurs fairly quickly. Of course, pneumonia has happened before, with which the patient was admitted to the hospital in serious condition and was even in the intensive care unit - then the treatment is more difficult and the recovery process is longer. As for viral pneumonia, this phenomenon is also not new. They had met before. For example, when they were caused by influenza infection. But “covid” pneumonia is completely different. In general, the coronavirus as such has existed for a long time; people suffered from it in the last century, but it was not the same as it is now, and did not cause such serious manifestations. COVID pneumonia does not respond to antibiotics. What complicates the situation is that there is no drug in the world to directly combat COVID-19. The course of the disease is different, it develops according to a special mechanism and affects other structural units of the lungs.
But now we are not talking about methods of treating pneumonia.
We are now talking about the patient’s recovery after suffering from pneumonia, about rehabilitation, about returning to full-time work. Since treatment of viral pneumonia is a long and difficult process, recovery does not always go smoothly. Changes in the lungs of patients may “freeze” for some time and remain in one state for a long time. After discharge from the hospital, a person may still have a slight dry cough, weakness, and increased fatigue. This, of course, frightens many patients. Imagine the situation: a person had never been seriously ill before, was strong, fit and athletic, but now he constantly experiences weakness, discomfort in the chest, and cannot breathe as usual. People with chronic respiratory diseases adapt to such symptoms over time and learn to cope with them. For those who encounter it for the first time, it causes panic. Therefore, if treatment is no longer required, but the above manifestations remain, then special attention should be paid to the patient’s rehabilitation.
We will not talk about all recovery methods; we will leave this to specialists in physical therapy and rehabilitation. Let us dwell on a more “narrow” section of rehabilitation—patient nutrition.
Nutrition for patients during pneumonia is designed to maintain the patient’s strength, increase the body’s immune properties, and prevent the negative effects of medications. And after the temperature drops, it helps to restore metabolic processes and regenerate lung tissue.
The calorie content of the food should correspond to the patient’s condition. The diet should contain a sufficient amount of protein, an increased amount of vitamins A, B1, B2, B6, B12, E, C and D, microelements, a moderately limited amount of carbohydrates, fat and table salt. The diet should contain a sufficient amount of liquid - at least 1.5 -2 liters per day. Vitamins and minerals help improve immunity and reduce the likelihood of complications.
During the period of high body temperature and intoxication, caloric intake is limited to carbohydrates and fats; it is recommended to consume a sufficient amount of liquid (2 - 2.5 liters) in the absence of contraindications. Tea with lemon, rosehip infusion, cranberry juice, and herbal teas that promote phlegm removal are a good thirst quencher and pleasant to the taste. You can add a few slices of lemon and ginger to boiled drinking water. 1 glass of rosehip decoction contains the daily requirement of vitamin C.
Many patients with pneumonia are treated at home. Here it is important to take into account that physical activity decreases, the body’s energy consumption decreases (on average by 300-400 kcal per day), and the availability of free time and easy access to food leads to the consumption of much more food than is necessary for the body’s vital functions. And this can inevitably lead to weight gain and the accumulation of visceral fat and a decrease in muscle mass. To avoid such weight gain, it is necessary to slightly reduce the energy value of the diet and increase the patient’s physical activity (according to how he feels).
The diet should contain 3 main meals and 1-2 snacks.
For breakfast you can prepare porridge, omelet, cottage cheese casserole, tea, coffee.
For lunch - various soups; side dish of boiled or stewed vegetables, porridge, pasta; from meat dishes - dishes from fish, meat or poultry (preferably lean meats); A carrot or beet salad seasoned with vegetable oil is a must. Drink – rosehip decoction, fruit drink, jelly, compote.
Dinner - a vegetable dish, a dish of cottage cheese, a dish of meat or fish, tea, tea with milk.
Snacks - second breakfast and afternoon snack - nuts, dried fruits, milk and fermented milk products with dried goods, savory cookies, bread, cereal bars, muesli.
At night, products containing probiotics (yogurt, kefir, bifidin, etc.) are recommended, which stimulate the restoration of normal intestinal microflora after drug treatment.
Therefore, it is important that the patient understands that the doctor can prescribe treatment and rehabilitation, but in order to get into the right psychological mood, you just need to work on yourself, this is a temporary phenomenon. And if the patient follows the doctor’s recommendations, everything will recover over time - just not as quickly as we would like.
How does Nutrimun help with pneumonia?
Nutrimun allows you to supply the body with food protein of the highest biological value, easy to digest and assimilate. You can now get the required amount of complete protein even in the smallest portion sizes.
It is enough to add Nutrimun to your food or drink, which will add protein to any dish: soups, casseroles, soufflés, porridges or juices.
Enriching the diet with protein helps to: replenish its large losses during the febrile period of the disease; stimulate recovery processes; prevent changes in the composition of the blood formula associated with taking antibacterial drugs
Resorption therapy for pneumonia
During pneumonia, lung tissue is damaged, a cough with sputum develops, and a high temperature rises. In addition to antibacterial drugs, vitamins, and immunity-boosting agents, the doctor prescribes physiotherapy and resorption therapy. Resorption therapy includes UHF (ultra-high frequency electromagnetic current), electrophoresis, physical therapy, chest massage and breathing exercises. Resorption therapy helps clear the bronchi from mucus, improves respiratory function, enhances metabolic processes and blood circulation in the lungs and stops the inflammatory process.