The first description of hypospadias dates back to the second century AD in the work of Galen, who first used the term. During the first millennium, the only treatment for this pathology was amputation of the penis distal to the external opening. Since then, there have been great changes in the surgical treatment of this defect for the better. More than 300 different methods for correcting this pathology are described in the medical literature. Although most of the techniques used today have been described over the past 60 years, the basic principles were proposed more than a century ago.
Modern methods of anesthesia, microsurgical instruments, sutures, dressings and antibacterial therapy improve the results of treatment of hypospadias and, in most cases, allow reconstruction to be performed in one stage during the first year of the child’s life.
What is hypospadias?
Hypospadia is underdevelopment of the urethra and penis, when the external opening of the urethra does not open in its usual place, but on the lower surface of the head, shaft of the penis, in the scrotum or perineum.
Hypospadias in most cases is accompanied by curvature of the penis, as well as splitting of the foreskin, which looks like an apron covering the head of the penis on top.
Often there is a narrowing of the outlet of the urethra - meatostenosis or narrowing of a more extended section of the urethra - dysplasia.
Indications for surgery
Meatotomy is indicated at any age if the narrowing of the external opening of the urethra causes a disturbance in the process of urination (dysuria).
Correction of hypospadias at a young age is indicated for the following reasons:
- — ensuring normal emptying of the bladder (male type) without splashing the stream of urine and its deflection;
- — ensuring normal erection and sexual intercourse in the future;
- - prevention of urinary tract infection;
- — correction of the possible occurrence of impotence and infertility;
- - achieving normal structure of the external genitalia;
- — ensuring psychosocial adaptation in society.
Timing of the operation
Until 1980, correction of pathology was carried out in children over 3 years of age due to the larger size of the organ. However, genital surgery at this age (children's awareness of genitals and self-identification as a particular gender occurs around 18 months of age) can result in significant psychological trauma, including abnormal behavior and gender identity disorder. Late surgical treatment during puberty and older leads to more frequent complications, first of all, the occurrence of fistulas occurs more often, with a probability of more than 50%. Some works by foreign authors indicate a higher number of complications in 5-year-old patients than in one-year-old patients.
Currently, most urologists try to operate on hypospadias at the age of 4-18 months, with a tendency towards earlier dates. This is associated with improved emotional and psychological outcomes. Tissue healing also occurs faster at an earlier age.
Treatment of hypospadias.
Treatment of hypospadias is carried out only by surgical methods. It is preferable to perform operations at the age of 6-18 months, and for capitate hypospadias up to 3 years. The result depends on the skill of the surgeon, his knowledge of the most advanced techniques and the healing characteristics of the patient.
Milder forms of hypospadias (capitate, coronal, distal trunk) are treated using one-stage operations.
Complex variants (trunk with pronounced curvature, scrotal, perineal) are best treated in two and sometimes in three stages.
Today we can state that the problem of treating hypospadias has been largely solved. In good hands, the positive results of primary operations are 75-90%. The best specialists have 90-95%.
Urine drainage and wound dressing
Urine is drained using a transurethral drip stent or through a drainage tube placed above the pubis. Some surgeons do not perform drainage after repair of distal hypospadias. It is common to apply a circular bandage with light pressure, as well as prescribe antibiotics for prophylactic purposes. The duration of stenting and bandaging varied significantly between studies. Due to the low level of evidence, no recommendation can be made.
Problems of surgical treatment of hypospadias.
At the same time, one should not think that treating hypospadias is not difficult. We often meet children who have been operated on 4 and 6 times without success.
Unnecessary operations waste time and health. These are anesthesia, which are not indifferent to the child. And the loss of precious plastic material - the skin of the foreskin, from which it is best to create the missing part of the urethra.
Our practice has accumulated the largest experience in Russia of modern one- and two-stage corrective operations, which have proven themselves to be the best in leading foreign centers. These methods serve as the basis for treatment. Our original developments and modifications of the technique allow us to use the individual characteristics of the patient to achieve a more complete functional and cosmetic effect and fundamentally reduce the frequency of complications.
We pay special attention to children and adolescents admitted after unsuccessful treatment, and we achieve significant improvements even in patients who have lost hope and are tired of unsuccessful surgical operations.
Treatment
Photo: b2.img.mobypicture.com
Patients with hypospadias are supervised by a urologist-andrologist. Treatment should be started as early as possible. Optimally, correction of the pathology should be performed in children aged 8-16 months – during this period there is an optimal ratio between the size of the corpora cavernosa and the supply of penile skin. In addition, early intervention helps prevent the development of psychological problems associated with penile defects and difficulties with urination, and avoid the formation of an inferiority complex. In any case, the operation is recommended to be performed before reaching 5-6 years of age.
The main goals of treatment are:
- straightening the penis;
- restoration of the missing part of the urethra;
- movement of the external opening of the urethra to the area of its normal anatomical location;
- giving a natural appearance to the penis;
- ensuring sexual function in the future.
It is impossible to cure hypospadias with medications, but medications are used after surgery. The list of medications, the method and duration of use, as well as the dosage are calculated by the attending physician, taking into account the nature of the pathology and the individual characteristics of the body. Traditional methods also do not produce results, since plant extracts cannot correct congenital disorders of the anatomical structure of the genital organs.
The prognosis if you consult a doctor in a timely manner is favorable. In 75-95% of children, a good functional and aesthetic result is observed in the long-term period.
Surgery to correct hypospadias
In patients with capitate hypospadias, surgery is indicated for narrowing of the external opening of the urethra. Urethral stricture prevents normal urination, promotes the accumulation of urine in the overlying sections, leading to the development of hydronephrosis and atony of the bladder. Taking into account the listed negative consequences, the operation should be performed early.
In infants, meatotomy is effective. In the future, conventional dissection often becomes insufficient due to the formation of scar adhesions around the urethra. In such cases, plastic intervention is required - isolation of the external opening with a circular incision, followed by dissection and suturing to the edges of the skin wound.
For other types of the disease, it is necessary to straighten the penis before dilating the urethra. The skin of the penis is mobilized, separated from the underlying tissue. The connective tissue bridges are dissected. The plastic surgery method is chosen taking into account the nature and severity of the curvature of the penis. If necessary, the skin of the scrotum and foreskin is used to create flaps. After completion of the intervention, a catheter is installed in the urethra, which is then removed after 4-5 days.
Urethroplasty can be performed in many different ways. It is possible to use distension (expansion) or tunnelization, replacing the defect with local tissues, free auto- and homografts. To form the missing section of the urethra, flaps of the oral mucosa or bladder, and skin from other parts of the body are used.
The technique is selected taking into account the structural features of the patient’s urethra. When choosing, take into account that the canal must have a stable lumen without a tendency to narrow, be extensible (this is necessary for a normal erection) and have sufficient ability to grow as the child grows older.
Currently, preference is given to tunnelization and replacement with local tissue (skin of the penis or scrotum), since these options provide better long-term results and are less likely to be complicated by rejection. Regardless of the chosen method, long-term bougienage is necessary in the postoperative period to prevent the development of stricture.
Female hypospadias
Treatment tactics are determined by the form of the pathology. Vestibular hypospadias does not manifest itself clinically and becomes an incidental finding during a gynecological examination. In the absence of complications, correction is not required. Non-surgical plastic surgery with the introduction of a special gel is indicated in the presence of recurrent cystitis caused by infection of the urethra by microorganisms from the nearby vagina. The injection of hyaluronic acid ensures a displacement of the opening of the urethra towards the clitoris and prevents repeated contamination with flora during the release of vaginal contents.
With the vestibulovaginal variant of the pathology, transposition of the urethra is performed - its surgical movement closer to the clitoris. The operation is also usually performed at a young or mature age. The only type of pathology that requires early intervention is total hypospadias. Particularly complex treatment, often involving multi-stage plastic techniques, is required in the absence of the urethra (in this case, the vagina is connected directly to the neck of the bladder) or the fusion of the vagina and urinary tract.
Causes of hypospadias. Incidence of hypospadias.
The causes of hypospadias are hormonal changes in the body of the mother and fetus, as well as genetic defects. Hormonal changes can also be genetically programmed, but can also be a consequence of external and internal influences on the body of the mother and fetus. Genetically determined variants of the defect generally constitute a more severe group.
The question of possible causes of hypospadias requires a separate discussion. We are currently doing a lot of work together with endocrinologists, geneticists and gynecologists to more accurately answer questions about the reasons for the birth of children with hypospadias and the possibility of preventing similar defects in future offspring.
Hypospadias occurs in 1:100 to 1:1500 male newborns. Capitate and coronal hypospadias occur in approximately half of the cases. Truncal hypospadias in a third of cases. Severe forms of hypospadias occur in 10-20% of patients.
After artificial insemination, children with hypospadias are born 2-3 times more often. However, according to our data, there is no direct connection with the process of artificial insemination itself, and the characteristics of pregnancy, the threat of miscarriage, the degree of maturity of the child at birth and the phenomena of hormonal imbalance are of greater importance.
Causes
All the causes leading to hypospadias have not yet been fully studied. It has been established that the leading role in the increase in the number of people suffering from this disease is played by the environmental situation, point mutations of genes, and consumption of food products containing disruptors: androgen destroyers and androgenic substitutes that change the hormonal status of the fetus in such a way that the process of sex formation is disrupted. Currently, disruptors include fungicides, phthalates, pesticides and herbicides, most of which are present in our daily lives. Often, the development of hypospadias can be caused by hormonal therapy prescribed to the mother when there is a threat of miscarriage, or hormonal contraception carried out before the expected pregnancy in less than 12 months. A fairly high risk of giving birth to a boy with hypospadias is possible with in vitro fertilization, since female sex hormones are used during pregnancy, which adversely affect the development of the child’s genital organs. Hereditary factors also play an important role. There are known cases of children being born with this diagnosis in several generations.
Forms of hypospadias.
The forms of hypospadias differ depending on the location of the external opening of the urethra - the meatus: on the head - capitate, in the area of the coronary groove - coronal, on the shaft of the penis - stem, in the area of the scrotum - scrotal or perineum - perineal.
Capitate form - at the site of the normal location of the external opening of the urethra, a urethral plate or longitudinal depression to the coronary groove is determined. The external opening of the urethra, the meatus, is often narrowed, which is called meatostenosis. Curvature of the penis is rare. Complaints arise when the external opening of the urethra narrows or when the head tilts down. The curvature of the head may increase during sexual activity.
Coronal form of hypospadias - the external opening of the urethra is located in the area of the coronary groove. More often than with the capitate form, there are complaints of impaired urination and curvature of the penis. Children urinate in a thin, tense stream. Often urine gets on your feet. Therefore, during urination it is necessary to raise the penis.
If the curvature of the cavernous bodies of the penis is pronounced, then during surgical straightening the coronal form becomes more severe - the trunk or even the scrotal-trunk, which must be taken into account when planning the operation.
Trunk form of hypospadias - in patients, the location of the external opening of the urethra is noted at different levels of the stem part of the penis. Complaints of impaired urination (the stream is directed downwards), which makes it difficult to urinate in an upright position. Children urinate while sitting on the potty or are forced to strongly lift their penis upward to correct the stream. Characteristic is curvature of the penis, sometimes with rotation and deviation to the side. As a rule, there is a narrowing of the external opening of the urethra - meatostenosis, but there are narrowings located along the urethra. Truncal hypospadias is often divided into distal trunk - the external opening of the urethra - the meatus is located on the trunk closer to the coronary groove and proximal trunk - when the meatus is located closer to the scrotum. This division is carried out to more accurately determine surgical tactics.
The penoscrotal form of hypospadias or scrotal-trunk is distinguished by the fact that the opening of the urethra is located on the border of the scrotum and the shaft of the penis.
Scrotal hypospadias is one of the most severe forms of hypospadias. The urethra opens between the halves of the split scrotum. Characterized by severe underdevelopment and curvature of the penis. The penis resembles an enlarged clitoris. The split scrotum enhances the resemblance to female genitalia. Urination is possible only while sitting. Urine gets on the skin of the scrotum, often causing irritation and inflammation. Newborns with scrotal hypospadias are often mistaken for girls or girls with adrenogenital syndrome.
Perineal form of hypospadias - The urethra opens behind the bifurcated scrotum. The penis is sharply reduced in size and sharply curved, often hidden at the base of the scrotum (transposition of the scrotum). The external opening of the urethra is wide. The head and cavernous bodies of the penis are underdeveloped. The foreskin is split.
Perineal and scrotal forms of hypospadias are often combined with undescended testicles (cryptorchidism), which makes sex determination even more difficult. Children suffer from severe complexes. After puberty, complaints appear about the inability to have sexual intercourse.
“Hypospadias without hypospadias” or hypospadias of the chord type - Underdevelopment and shortening of the urethra, manifested by downward curvature of the penis with a normal location of the external opening. The urethra, like a bowstring, bends the corpora cavernosa during erection of the urethra. There are defects with narrowing - urethral dysplasia and normal patency of the canal. There are embryonic scars around the urethra, increasing the curvature of the corpora cavernosa. The defect is very difficult to treat. The degree of curvature of the penis increases sharply during puberty and during erection.
Individual differences in patients with hypospadias include the degree and shape of the curvature of the penis, variants of narrowing of the urethra, and the shape of the scrotum. Sometimes, with the capitate and coronal form of the defect, there is no curvature of the penis or splitting of the foreskin.
Proximal hypospadias
The most common pathology of the penis in boys is undoubtedly hypospadias. The incidence of this anomaly, according to various authors, is increasing and amounts to 1:125. Proximal forms are less common with a frequency of 1:1200 newborn boys and are characterized by more pronounced curvature of the corpora cavernosa, often with dysplasia of the corpus spongiosum of the urethra. The external opening of the urethra is localized in the area of the penoscortical angle, scrotum or perineum. The foreskin is located on the dorsal surface. At an older age, such children urinate according to the female type.
Surgical treatment of proximal hypospadias is more complex than distal hypospadias. Since, in addition to moving the external opening of the urethra to the apex, it is necessary to straighten the corpora cavernosa and eliminate dysplastic tissues, which can lead to secondary curvature at an older age.
Depending on the surgeon's experience and preference, surgical correction is performed using either one-stage or two-stage techniques.
Patients with proximal forms, micropenia, or a non-palpable testicle often require a differentiated approach to treatment. Such children may require consultation with an endocrinologist, geneticist, and additional examination methods to determine the karyotype in order to exclude gender pathology.
Materials and methods
Over the past few years, a large number of patients with this pathology have been operated on. The age of the patients ranged from 5 months to 17 years. This group included patients with primary hypospadias that had not been previously operated on. Patients underwent Onlay-tube surgery and Bracka surgery using buccal mucosa. Before surgery, all patients were prescribed hormonal ointments on the glans penis and foreskin to increase the supply of plastic material. In both groups, PDS 7.0 was used for tissue suturing. The bladder was catheterized with an age-sized urethral catheter. In two-stage operations using the Bracka technique, after fixing the free flap, pressure was applied to it using a special “pellet” for the purpose of engraftment. The second stage was carried out after 5-6 months.
results
In the group of patients operated on using a one-stage technique, 10% of complications were observed. These complications included fistulas, urethral diverticula, and smegmal stones. A certain percentage of patients required a second stage, since they were able to form the urethra only up to the coronary sulcus or the size of the glans penis was insufficient for closure.
Patients operated on using the two-stage technique had about 4% complications. The vast majority of these were urethral fistulas. All patients were assessed for urodynamic characteristics, which showed a higher average urinary flow rate in patients after the Bracka procedure.
conclusions
Thus, the use of two-stage techniques for the correction of proximal forms of hypospadias allows us to obtain a lower percentage of complications and better urodynamic characteristics of urine flow.
How to make the correct diagnosis for hypospadias?
Diagnosis of capitate, coronal and truncal hypospadias does not cause difficulties for specialists. A careful examination will clear up most of the questions. To clarify the presence of narrowings in the urethra, the volumetric flow rate of urination is determined - uroflowmetry. If the rate of urination decreases, the entire urinary system is diagnosed. Impaired urine outflow caused by narrowing of the urethra during hypospadias may result in decreased sensitivity of the bladder and the occurrence of vesicoureteral reflux. Combined genitourinary anomalies also occur.
Severe cases of hypospadias are more difficult to diagnose, especially when one or both testicles are absent from the scrotum. In such cases, genetic analysis is mandatory - determination of the karyotype, ultrasound of the kidneys, bladder and internal genitalia. Cystoscopy is performed to diagnose the genitourinary sinus. For rare combined defects, magnetic resonance imaging (MRI) is performed. Laparoscopy is sometimes used as a final assessment of the internal genitalia. Examination of children with severe forms of hypospadias is possible only in multidisciplinary specialized centers.
Concomitant pathology&
Often, hypospadias in boys is combined with other developmental anomalies: inguinal hernia, cryptorchidism, hydronephrosis, vesicoureteral reflux, myelomingocele, urogenital sinus, etc. Therefore, an ultrasound of the kidneys and bladder is recommended for all children to identify concomitant pathology of the urinary system before surgery. In the presence of hydronephrosis or vesicoureteral reflux, the first step is correction of the pathology of the upper or lower urinary tract, and after that, surgical treatment of hypospadias.
Associated anomalies with hypospadias.
Hypospadias can be combined with defects of the genitourinary system - undescended testicle, inguinal hernia, kidney anomalies; as well as other organs and systems - heart defects, pyloric stenosis, anal atresia, as well as with genetic abnormalities - hereditary syndromes, variants of hermaphroditism.
Hypospadias may be an external manifestation of more severe malformations of the reproductive system. More than 120 diseases are known that include hypospadias as a component, requiring in-depth diagnosis and combined treatment together with endocrinologists and geneticists. Sometimes such children need gender reassignment at an early age. An erroneously chosen treatment approach cripples the lives of patients and leads to family tragedies. Treatment of such patients should be carried out only in multidisciplinary centers.
Several times a year we encounter patients whose gender was incorrectly assigned at birth. We are currently seeing 4 boys with hypospadias who were raised as girls. One of them was a girl under 16 years old when she was admitted to us and the correct diagnosis was made. Diagnosis of such cases is difficult and requires a detailed, complex examination followed by difficult psychological and surgical correction.
Most often, the time to achieve the best result at the time of admission in such patients is lost. Such patients at an older age often have to undergo sex reassignment surgery, since it is no longer possible to recreate a penis of a decent size.
Description
Hypospadias is an anomaly caused by clefting of the urethral opening.
Congenital pathology is characterized by an incorrect location of the exit of the urethra. In men, it can come out in the scrotum, shaft of the penis or venous groove. In women, the displacement occurs towards the vagina. Depending on the location of the exit of the urethra, hypospadias in boys can take the following forms:
- capitate;
- stem;
- coronal;
- perineal;
- scrotal;
- Chord type hypospadias.
Hypospadias is often accompanied by curvature of the penis or its abnormal development, which affects urination and sexual activity. Most often, boys suffer from the pathology (one case per 200-300 newborns); hypospadias is rare in women.
In most cases, congenital defects of the urinary system are discovered at birth. The disease is treated by a urologist, but sometimes consultation with an endocrinologist and geneticist is required, since the causes of the anomaly can be hormonal disorders or genetic predisposition.
Hypospadias: features of pathology
The main feature of the pathology is that, under the influence of certain factors, a disruption occurs in the formation of the urinary system in the womb. These disorders are manifested by the incorrect location of the urethra, it is displaced towards the trunk or scrotum.
Due to the shorter length of the urethra, curvature of the male genital organ is often observed. Depending on the form of hypospadias, other pathologies may be observed in children:
- splitting of the foreskin;
- pathologies of kidney development;
- incorrect sizes of the scrotum and genitals, and so on.
According to statistics, hypospadias in boys is one of the most common congenital defects of the genitourinary system. But hypospadias in girls is extremely rare, and in mild forms it does not require medical intervention.
Causes of hypospadias
Scientists have found that the development of pathology occurs at 10-14 weeks of pregnancy, during the period when the urinary system is formed. That is why the causes of hypospadias are most often associated with the mother’s diet, as well as taking medications, and exposure to various factors.
Among the main factors that can cause the development of pathology, it is worth noting:
- taking hormonal medications during pregnancy;
- use of hormonal contraceptives during the year before conception;
- hereditary predisposition;
- environmental factor;
- some diseases of a woman during pregnancy.
The development of the defect can be caused by chemicals contained in herbicides, pesticides, and fungicides. The increase in cases of hypospadias in children in recent years is associated with the deterioration of the environmental situation and the presence of chemicals in the life of every person.
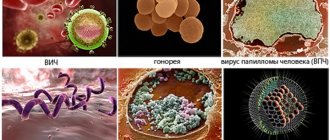
Diseases during pregnancy can also contribute to the development of pathology:
- rubella;
- flu;
- ARVI;
- AIDS;
- venereal diseases;
- nephrosis;
- toxicosis.
When there is a threat of termination of pregnancy and artificial insemination, when a woman undergoes a course of hormonal therapy, genital hypospadias in boys develops many times more often.
Forms of hypospadias
Hypospadias of the penis, depending on the characteristics of the exit of the urethra, can take different forms.
Capitate hypospadias is characterized by the fact that the urethra exits the head, but is displaced towards the venous groove. The capitate form of the pathology is considered the mildest, since it is rarely accompanied by curvature of the penis and other serious complications.
Coronal hypospadias is distinguished by the location of the urethral opening in the area of the venous groove. In most cases, with this form, there is curvature of the penis to one degree or another.
Trunk hypospadias is characterized by severe curvature of the penis, which is facilitated by the short length of the urethra. Urinating while standing causes some difficulties. To avoid getting your feet and clothes wet, you need to pull your penis towards your stomach.
Scrotal hypospadias refers to the posterior forms of pathology. The external opening of the urethra is located on the scrotum or close to it on the shaft. A man with this form of the disease can urinate only the female way, that is, while sitting.
Perineal hypospadias is one of the most complex forms of pathology. The urethra is located in the perineum. You can only urinate while sitting. Often the external genitalia are underdeveloped; they look more like huge female labia and clitoris.
Chord type hypospadias is a special form of the disease. The urethral opening is in the correct location. The presence of an anomaly is indicated by severe curvature of the penis, which complicates the sexual life of adult men.
Hypospadias in women
As practice shows, hypospadias in girls is quite rare. The pathology in women is characterized by the fact that the opening of the urethra is shifted towards the vagina. In most cases, the hole is large, but the functioning of the urinary system is not impaired.
In severe forms of the disease, urination may occur in the vagina. Urinary incontinence may also occur if the cleft affects all or most of the urethra. If a girl is diagnosed with hypospadias, the form of which is severe, concomitant pathologies may include:
- improperly developed perineum;
- double uterus;
- disturbances in the development of the vagina.
Complications and consequences of hypospadias
Boys diagnosed with hypospadias always have urinary problems. An adult man may have problems with ejaculation. In the presence of congenital pathology, inferiority complexes are formed. A psychological barrier also appears that prevents you from building relationships with the opposite sex, and so on.
Hypospadias, the consequences of which can be more serious and not limited to psychological problems, are often accompanied by disorders in the genitourinary system. Various chronic diseases develop, which significantly worsen the quality of life.
If left untreated, complications of hypospadias may develop:
- narrowing of the urethra;
- urinary retention in the kidneys, which leads to the appearance of an inflammatory process;
- infertility;
- irritation of the skin in the area of the exit of the urethra, which can turn into a purulent form;
- fistulas;
- mental disorders and depression due to lack of sex life.
Many people are concerned about the question of whether hypospadias is inherited. Unfortunately, one of the reasons for the development of pathology is a hereditary factor. In medical practice, there have been cases where the anomaly was observed in several generations. Because hypospadias can be caused by genetic mutations, genetic counseling is often necessary.
Hypospadias is a congenital disease, as it develops during the formation of the urinary system in the womb. A person cannot acquire it in the course of his life.
Is hypospadias dangerous? Why does hypospadias need to be treated at an early age?
Problems associated with hypospadias depend on the age of the patient. In the first years, complaints about urination arise - difficulty or inability to urinate while standing. At the age of 3, the child evaluates the appearance of his genitals and from that moment experiences his difference from the surrounding boys and men. In adulthood, difficulties or impossibility of sexual intercourse are added. The degree of dissatisfaction with oneself is difficult to overestimate, and many patients with hypospadias early begin to suffer from neuroses and severe chronic stress, with all the ensuing consequences for the patient himself and those around him. Incorrect position of the urethral opening in patients with hypospadias is one of the causes of infertility.
Today, with the development of surgery, it has become possible to correct hypospadias already in the first year of life. This is the best age for treatment. The child does not understand that he is in the hospital. There is no trace of the disease left in his memory! Only complete reconstruction at an early age reliably saves a child from severe moral trauma for life.
Combined pathology
Hypospadias is often combined with a narrowing of the external opening of the urethra. Undescended testicles and inguinal hernias are the anomalies most often associated with hypospadias. In 1981, Khuri's review of over 1000 patients with hypospadias reported that the incidence of cryptorchidism and inguinal hernia was about 9%. In more severe forms of hypospadias, the frequency of undescended testicles exceeded 30%, and the combination with inguinal hernia reached 20%. A combination with such pathologies as: cryptorchidism - 9%, inguinal hernia - 9%, hydrocele, urethral fistula, testicular hypoplasia, anomalies of the upper urinary tract and vesicoureteral reflux was also noted. Cardiovascular and craniofacial malformations are extremely rare.
The combination of hypospadias with undescended testicles may be associated with a violation of sex formation and requires a more complete endocrinological and genetic examination before surgery. In a 1999 study by Kaefer et al., sex formation disorder was identified in approximately 30% of patients with hypospadias and cryptorchidism. Moreover, the more proximally located the external opening of the urethra, the higher the likelihood of disorder of sex formation (DSD). If one gonad is not palpable, then the possibility of DSD increases to 50%, if both testicles are palpable, then 15%.
Frequency of occurrence
The incidence of this anomaly is 1 in 250 boys born on average in the world and is the most common disease of the urinary tract. In some countries there is a trend towards an increase in the birth of children with this problem. In general, the birth rate is fairly constant - 0.26 per 1000 children in Mexico and Scandinavia, 2.11 per 1000 births in Hungary.
The incidence of hypospadias is higher in whites than in blacks, and is more common in Jews and Italians. Familial inheritance of hypospadias is about 7%.
Should a child with hypospadias be shown to a urologist during adolescence?
With the growth of the penis during adolescence and the appearance of secondary sexual characteristics, a second wave of problems associated with previous operations often arises. Often the deformation of the penis increases due to limited growth of the created part of the urethra or preserved embryonic scars on the cavernous bodies. Hair can grow in the urethra if it was made, at least partially, from the skin of the scrotum, which contains hair follicles. Insoluble uric salts settle on the hair and form stones, which can serve as an obstacle to urination. A sharp expansion of the created urethra - a diverticulum accumulates urine and is manifested by leakage of urine after urination. Diverticula are sometimes combined with narrowing of the created urethra.
It is best to carry out examinations at the age of 13-14 years. If more than 10 years have passed from the time of the operation to the time of examination, it is likely that a hypospadiologist, having modern means and methods of correction, will find an opportunity to solve the patient’s problems. This can often be done through non-operative methods or simply advice.
Hormonal studies and spermogram analysis at the age of 16-17 years will help to correctly assess the characteristics of the reproductive system in a boy and his ability to fertilize.
Causes
The main factors that can provoke the development of pathology include:
- Genetic predisposition.
- Poor environmental situation in the area of residence.
- Taking hormonal drugs during pregnancy.
- Taking contraceptives with a high estrogen content (due to which there are not enough male hormones for the normal development of the boy).
- Harmful effects of chemicals.
- Acute infections in early pregnancy.
There is also scientific speculation that genetic changes may be caused by harmful substances contained in hairspray.
Treatment of hypospadias.
In the process of surgical treatment of hypospadias, several main tasks are solved: 1. straightening the penis and giving it a natural appearance 2. forming the urethra from an elastic plastic material devoid of hair follicles 3. Forming the glans penis. 4. Extraction of the urethra to the apex of the head with the formation of the external opening of the urethra of normal location and shape. In severe forms of hypospadias, 5. elimination of transposition and splitting of the scrotum is additionally carried out.
The difficulty of surgical treatment of hypospadias lies in both achieving good patency of the urethra and the formation of a penis that has a normal appearance, as well as in preventing possible postoperative complications.
Diagnostics
It is possible to diagnose capitate and coronal hypospadias already in adolescence, since these forms mainly appear during erection. The stem form of the disease can be detected already at the birth of the child. The scrotal and perineal forms can often cause problems in determining the sex of the child.
For a complete intrauterine analysis, genetic studies are necessary. To carry out such an analysis, it is necessary to examine the external genitalia, examine the chromosomal set of cells to determine the sex of the child, and conduct an ultrasound examination of the kidneys and bladder to identify various types of pathologies.
If a screening ultrasound reveals any pathologies, then treatment of the upper and lower urinary tract is carried out, and then the hypospadias is subject to surgical intervention.
Often other abnormalities are observed with hypospadias. The most common include inguinal hernia and cryptorchidism (undescended testicles).
Treatment of hypospadias
If this diagnosis is made at birth, then when the child reaches six months of age, it is necessary to consult with a urologist and undergo surgery in a timely manner. There is no drug treatment, the only treatment is surgery. However, it is important not to waste time and do everything on time.
The optimal time is when the child is from 6 to 18 months. The best time is six months, since if a repeat operation is necessary, you must wait six months. In the vast majority of cases, one operation is enough. It goes away within 1-4 hours.
Why is it important to have surgery at this age?
The fact is that children tolerate the operation itself much easier and go through the rehabilitation period less painfully. Children under three years of age often have no memory of the operation at all, which is important for their normal psychological development. In the period from 1 to 3 years, the size of the penis remains approximately the same. The difference between the length and width of the penis at this age is small, which is very important.
The complexity of the operation directly depends on the form of hypospadias. Treatment is carried out in one stage, but when proximal forms are identified, two-stage operations are necessary.
This type of operation belongs to the reconstructive plastic type, so specialists require a lot of experience. During surgery, doctors will have to return the opening of the urethra to its typical place and eliminate associated disorders of the genitourinary system. Thus, the penis after surgery should have a normal appearance and perform its two main functions - urination and reproductive.
The operation itself can be divided into three parts:
- Elimination of curvature of the penis.
- Creation of the missing part of the urethra (in this case, the tissue of the prepuce of the skin pouch covering the head of the penis is used) or the dorsum of the penis. Moreover, the skin for the operation is taken immediately with blood vessels, which allows it to grow along with the penis itself and change as the boy grows up and becomes a man.
- Plastic surgery of the external urethral opening, which is located in the upper part of the head of the penis and has a longitudinal direction. Thanks to this, the urine stream has a direct direction and does not splash.
During the operation, it is also important to eliminate all aesthetic defects. So, at the request of the parents, it is possible to create a foreskin. If this is not done, the penis will have a standard appearance after circumcision.
The entire operation is performed under general anesthesia. There are no sexual dysfunctions after it. However, no one can guarantee one hundred percent success. If complications occur, repeat surgery may be required.
When performing surgery at a late age, it is advisable to complete it before the boy reaches 7 years of age. If the patient is over 13 years old, the treatment results will be much worse. In this case, the child will have many different problems, including difficulty urinating, kidney inflammation, problems with the prostate gland, impotence, discomfort during sexual intercourse and much more.
Prevention of hypospadias
- Preparing for a planned pregnancy.
- Preventing the influence of harmful factors on the mother’s body during pregnancy, forming a normal regimen, optimal physical activity.
- Regular examinations during pregnancy by gynecologists.
- Timely contact a urologist if a disease is detected in a fetus or infant.
Possible complications after surgery
- A fistula is a channel between the urethra and the skin through which urine passes. Can be single or multiple. It is detected within 4 months after the operation.
- Stenosis is a narrowing of the opening of the urethra or a newly created section of the urethra. Causes painful urination or increased pressure in the kidneys and bladder.
- Dehiscence of the edges of the wound due to infection or narrowing of the new urethra. In this case, surgical correction is necessary.
- Chord is a curvature of the penis. In some cases, surgery is required.
If you find an error, please select a piece of text and press Ctrl+Enter
Stages of development of methods for treating hypospadias.
Urologists around the world have been solving the problem of treating hypospadias for more than a century. As a result, about 200 treatment methods and many options for their use were proposed. Until the mid-90s of the 20th century, almost every large clinic used its own modifications of surgical interventions, and in the hands of the authors they gave good results.
A fundamentally new stage in the treatment of hypospadias began in the 90s with the spread of digital technologies. At international urological conferences, video materials of operations and long-term results are shown. Many articles are supplied with high-quality photographic materials. Finally, it became possible to compare different treatment approaches and choose the truly best method.
If in the old days, evidence of the effectiveness of treatment for hypospadias was often words - statistically unproven statements about the advantages of certain methods, now the time has come for randomized multicenter studies and technologies that have proven their advantages in hundreds and even thousands of patients from different countries.
Urologists around the world exchange technologies and results. Today, not a single doctor can say my method is the best. Dozens of surgeons from different countries contributed to the improvement of technical techniques. The skill of a surgeon consists in mastering the entire arsenal of treatment methods and the ability to apply them creatively, in accordance with the characteristics of the pathology and the interests of the patient.
Modern principles of operations for hypospadias.
- Penis straightening
- usually performed by excision of embryonic scars on the lower (volar) surface of the penis, separating the urethra from the corpora cavernosa. Difficulty of the stage: on the one hand, it is important to prevent damage to the corpora cavernosa and shortening of the urethra; on the other hand, for complete straightening of the corpora cavernosa of the penis, it is necessary to completely excise the scar tissue.
- All subcutaneous adhesions are separated and the skin deficiency on the lower surface of the penis is eliminated.
- Sometimes, for minor curvatures, Nesbit straightening is performed by placing sutures on the tunica albuginea of the corpora cavernosa in the area of the dorsum of the penis.
- We often form the missing part of the urethra - the urethra - from the foreskin, skin of the penis and tissues of the glans. The plastic material must be free of hair follicles, so the use of scrotal skin is undesirable. If there is a lack of penile skin material, we use the mucous membrane of the lip or cheek.
Operation techniques
The general principles of the main stages are common to all methods. First, the corpora cavernosa is exposed from the skin of the penis. The fibrous cords and “notochord” present on the ventral surface are excised as much as possible. An “artificial erection” test is performed by injecting saline into the corpora cavernosa to detect any deviation of the penis. If the curvature is less than 45⁰, dorsal plication corporoplasty is performed under the neurovascular bundle. When the curvature is more than 45⁰, it is advisable to use patch corporoplasty or by applying multiple incisions on the ventral surface of the tunica albuginea of the corpora cavernosa. It is also possible to correct the curvature of the corpora cavernosa by intersecting the tunica albuginea at the point of maximum curvature and fixing a free graft (buccal mucosa, preputial skin or other grafts) to the resulting defect. This technique leads to the elimination of curvature and lengthening of the penis, in contrast to the plication method of correction.
If there is a pronounced fibrous “chord” or dysplasia of the corpus spongiosum of the urethra, it may require its intersection or excision. Various methods of urethroplasty can be used: tubularization of the urethral site itself, the use of local blood-supplied flaps, tissue grafts or urethral advancement procedures (GAP procedures).
The most commonly used technique for the correction of distal and mid-trunk hypospadias is TIP (tubularized incised plate, Snodgrass). This method allows you to create a urethra from local tissues according to the Duplay principle, but a distinctive feature is the dissection of the posterior wall of the urethra, which creates the opportunity for the formation of an artificial urethra of larger diameter. Current research shows that this technology is used by the majority of urologists worldwide to treat distal hypospadias.
Next, the wings of the head are mobilized to cover the formed urethra and give the head a more conical shape. Excess skin on the dorsal surface is mobilized to close the defect on the ventral part.
Various suture materials are used for urethroplasty, the most suitable for the requirements of modern plastic genital surgery are PDS 6-7/0 and Monocryl 6/0, as they are quite strong and quickly absorbable.
Many studies have shown that the use of additional layers of tissue (the foreskin, vaginal tunica, etc.) between the urethra and the skin reduces the risk of developing fistulas. The issue of using short urethral stents in combination with cystostomy and long-term catheterization of the bladder remains controversial. A retrospective study in 2015 showed that longer catheterizations of up to 3 weeks resulted in fewer complications than catheter placements of less than 1 week.
Repeated plastic surgeries for hypospadias, performed in conditions of insufficient plastic material, constitute a separate problem group of patients with a higher percentage of complications. To correct hypospadias in these patients, various free grafts are used: the mucous membrane of the cheek, lips, lower surface of the tongue, skin of the postauricular area, etc.
Correction of penis-scrotal transposition is usually performed as a separate stage, since additional incisions can cause ischemia of the skin flap from which the urethra is formed. It is usually performed six months after the main stage of the operation, when peripheral blood supply is restored.
Most forms of hypospadias can be corrected in one operation, but in case of severe curvature and removal of the dysplastic corpus spongiosum of the urethra, it is advisable to use a step-by-step approach. In this case, at the first stage, the penis is straightened, the urethral platform of the required diameter is created, and the urethra is formed at the second stage after 6 months. The diagram shows an algorithm for the treatment of proximal hypospadias:
Hormonal therapy before surgery
Many specialists use hormonal therapy to increase the size of the glans penis. Preoperative injections of testosterone or ointments (creams) based on testosterone or dehydrotestosterone, as well as injections of human chorionic gonadotropin are used. In a study of 182 children with distal hypospadias (mean age 30 months), Asgari et al. It has been shown that the use of parenteral testosterone can be effective in reducing the incidence of complications from 12 to 5%.
In our practice, we use Andractim Gel ointment or Androgel for preoperative preparation in patients with a small glans penis.
Own results of treatment of hypospadias. Original methods.
In our practice in the 80-90s, we went through a romantic stage of surgery, delusions and charm from our own developments. Based on the experience gained, as well as as a result of communication with colleagues from other countries and internships in foreign clinics, we have introduced the most reliable methods, which in most cases allow us to obtain perfect cosmetic and functional results.
The main components of success are an individual approach, effective methods, delicate microsurgical techniques, high-quality suture material and instruments, mastery of the entire modern arsenal of methods, extensive experience in reconstructive plastic surgery and the treatment of hypospadias, scrupulous management of the postoperative period.
Original modifications of surgical techniques allow us in some cases to significantly improve the cosmetic and functional results of treatment. For example, one of the most difficult stages of the operation is the formation of the capitate part of the urethra and especially the external opening of the urethra of a natural appearance.
| Traditional method of forming the external urethral opening according to Mathieu. The entrance to the urethra is in the form of a transverse slit. | An original technique for forming the external urethral opening. The entrance to the urethra has the natural appearance of a vertical slit. |
Price and cost of surgery for coronal (peri-coronal) hypospadias in children
| Service | Price |
| Surgical treatment of coronal hypospadias, category 1 of complexity | 83000 |
| Surgical treatment of coronal hypospadias, category 2 of complexity | 125000 |
| Surgical treatment of coronal hypospadias, category 3 of complexity | 175000 |
The price list published on the website is not a public offer agreement. The provision of services is carried out on the basis of an agreement for the provision of medical services. We ask you to check the cost of services with your attending physician in advance.
The cost of the operation includes (no additional payment for services is necessary!):
- inpatient accommodation 1 day double room with all amenities
- preoperative tests
- disposable suture material Vicryl, PDS
- application of intradermal cosmetic suture
- disposable surgical consumables
- surgical instruments Ceatec GmbH Germany
- microsurgical instruments and equipment
- constant telephone communication with the attending physician
- examination any day in the clinic within 14 days after surgery
The cost of the operation does not include: anesthesia, additional diagnostics and treatment of concomitant diseases and their complications.
Anesthesiological support: anesthesiological apparatus Drager Fabius Plus (Germany), combined general anesthesia (inhalation anesthesia, caudal/local anesthesia).
Don't waste your precious time - call!
Our specialists will be happy to answer all your questions
+7
Our advantages
Experienced surgeons
Individual approach
Without pain and fear
Comfortable conditions
Own results of operations for hypospadias
Operations for distal forms of hypospadias (capitate, coronal, stem without pronounced curvature of the penis) We have accumulated extensive experience in using various one-stage correction methods for coronary, stem and capitate hypospadias. Since 2000, we have been using our own modifications of one-stage Snodgrass-type operations for distal forms of hypospadias, which have been appreciated in recent years by leading hypospadiologists. These techniques allow you to achieve optimal functional and cosmetic results, fully preserve erectile function, while having a minimal risk of complications. At the same time, correction of curvatures and aesthetic correction of the penis is carried out.
| Truncal hypospadias before surgery | Truncal hypospadias after surgery |
The result of treatment of coronary hypospadias (with preservation of the foreskin)
Forecast
The use of modern anesthesia, suture material, microsurgical instruments, magnifying equipment, and antibacterial therapy makes it possible to perform surgical treatment of hypospadias in just one stage with minimal risk of complications and obtain an excellent cosmetic result. Compliance with the optimal timing of surgical treatment allows you to eliminate the psycho-emotional component in the child. The desire to perform surgical treatment before 2 years of age is also due to the fact that the child will not remember the very fact of treatment and hospital stay.
Studies conducted on patients who underwent surgery for hypospadias showed that they were more satisfied with their sex lives than those who did not have surgery.
It is worth noting that treatment methods for hypospadias continue to evolve. New methods of tissue adhesion are being developed: tissue adhesives and the use of laser for adhesion, which leads to improved wound healing and a reduced risk of fistula formation.
Cellular technologies are also being actively developed and will soon make it possible to create an artificial urethra, especially in patients with severe forms of hypospadias. The identification of factors and understanding of the causes leading to hypospadias continues, which allows us to develop an approach to the prevention of this condition and carry out correction in utero.
Operations for perineal and scrotal forms of hypospadias.
Surgeries for severe forms of hypospadias are the most complex and responsible. Preservation of both blood supply and erectile function to the maximum length of the penis is achieved through careful, delicate technique and a creative approach to each patient.
We have proposed a number of modifications aimed at achieving maximum penis size, its normal function, appearance and preventing complications.
| Scrotal shape before surgery | After a 2-stage operation |
Parents
The optimal age for hypospadias correction is 10 months.
Correction of hypospadias is most often performed in one operation.
You may need to use hormonal ointment before surgery. The ointment is applied 3 weeks before surgery in the morning and evening. The ointment should be applied to the penis, the size of a drop is the size of the nail plate of the parent’s thumb.
Before the operation, you need to collect the necessary tests.
In the postoperative period, 2 diapers are used, the catheter is removed into the second (external) diaper. This technique allows the child to be active throughout the entire period of hospitalization.
Antibacterial therapy is prescribed for the entire postoperative period.
After the operation, a special compression bandage is applied to the penis, and a urethral catheter is installed for 10-12 days. After this period, the bandage is removed and the catheter is removed.
To evaluate the result of the operation, it is necessary to videotape the process of urination.
Is it worth using one-stage operations for complex types of hypospadias?
We see many problems in adolescents who come to us after inadequate interventions carried out in early childhood.
The main disadvantage of one-stage interventions for complex types of hypospadias is the high risk of postoperative deformations of the penis (curvatures) due to shortening of the created urethra, as a result of impaired blood circulation in the displaced skin flaps and increased scarring. There is no escape from them, and the only way out is repeated reconstruction.
Curvature of the penis in a teenager after a one-stage operation performed at the age of 2 years. The created scarred urethra prevents erections by bending the penis downwards. A complete reconstruction is required.
Complications
Early complications include bleeding, inflammation, dehiscence, skin flap necrosis, and swelling. Late complications - urethral fistula, narrowing of the urethra, secondary curvature of the penis. The number of complications in the treatment of proximal forms of hypospadias is higher than with distal ones. Postoperative bleeding rarely occurs and is usually controlled by a compression bandage on the penis.
Urethral fistulas are long-term complications and are most often detected after removal of the catheter draining the urinary tract. The probability of fistula formation for most one-stage operations is about 10% according to world literature. When reconstructing proximal forms of hypospadias, the probability of fistula formation approaches 40%. Fistulas rarely close spontaneously and most often require reoperation after 6 months. The probability of fistula recurrence is about 10%.
Another complication is meatal stenosis, or narrowing of the urethra. Urethral strictures can occur in the long term and require bougienage; if ineffective, surgical treatment. Urethral diverticula may appear after urethral reconstruction using preputial skin. The created urethra does not have a frame base, therefore, when resistance to the flow of urine appears in the distal sections, a diverticulum-like expansion of the urethra occurs. This complication usually requires removal of excess skin tissue and suturing of the urethral tube onto an age-appropriate catheter. It is optimal to create the same diameter throughout.
One of the complications is the growth of hair in the urethra when using skin bearing hair follicles. As a result, stones appeared in the urethra, which required multiple repeated operations. Despite the fact that skin flaps with hair follicles have ceased to be used, such patients are still encountered in urologist practice.
Consultation with an endocrinologist
If a violation of sex formation is suspected in a patient with hypospadias, or if hypospadias is combined with cryptorchidism or micropenia, consultation with an endocrinologist is indicated.
How to choose a surgeon and clinic?
The choice of a surgeon is a fundamental issue for parents of a child with hypospadias. Typically, the choice of surgeon is made on a whim, recommendation or regional basis (closer to home). In developed countries, people go to the nearest large hospital, or less often to a private clinic.
However, our shortest path is not always the fastest. If you have no one to consult with, then we recommend 2-3 consultations with serious specialists to create an idea of the problem. It is important to find a doctor you trust. This simplifies relationships and understanding during the treatment process.
When there are urgent indications for treatment - narrowing of the urethra - meatostenosis, then the narrowing can be eliminated in the nearest hospital, however, only a hypospadiologist with extensive experience and constant practice can perform high-quality urethroplasty. When eliminating meatostenosis, you should not excise the foreskin, which will serve for subsequent urethroplasty.
Perhaps the best way to find a doctor is to communicate with parents of children who have already undergone surgery. But after finishing treatment, people tend to forget about solved problems, and therefore it can be difficult to find a knowledgeable interlocutor.
Folk remedies
Photo: otravilsja.ru
Correcting the location of the exit of the urethra and the curvature of the penis can only be done surgically. Traditional methods are ineffective in this case. It is also not recommended to use traditional recipes to improve healing after surgery - all necessary drugs are applied to the wound during dressings.
Unauthorized use of lotions, compresses, ointments and other local remedies can disrupt the process of tissue restoration, cause inflammation, stricture formation or transplant rejection. The only safe folk method is universal auxiliary therapy, carried out to strengthen the immune system and increase the body's defenses.
The child needs to organize proper nutrition with sufficient content of meat, dairy products and vegetables in the diet. Vitamin drinks will help improve the immune system and provide the body with useful compounds: rosehip tea, cranberry juice, infusion of sea buckthorn, honey and lemon. When choosing drinks, you should take into account the presence of an allergic predisposition and the possibility of developing diathesis. You can use any traditional methods only after consultation with your doctor.
The information is for reference only and is not a guide to action. Do not self-medicate. At the first symptoms of the disease, consult a doctor.
SEARCH FOR TREATMENT AROUND THE WORLD WITH YELLMED