Obesity is a disease that is manifested by increased deposition of fat in the subcutaneous tissue, which leads to excess body weight in the child. The diagnosis of obesity is made only if the child’s body weight exceeds normal by 10 percent or more.
The problem of obesity in children is becoming alarming and is characterized by steady growth. According to WHO statistics, about 22 million children under 6 years of age are obese.
It is worth noting that the cause of the development of obesity in adults often originates in childhood. With age, this disease contributes to the development of more serious conditions: type 2 diabetes mellitus, high blood pressure, orthopedic problems, etc. Thus, the widespread prevalence of obesity in the population and the large number of complications of this disease determine the relevance of this problem in pediatrics.
Causes of obesity in children
- Excessive quantity and improper quality of child nutrition, which leads to changes in the functioning of centers in the brain that are responsible for appetite.
- Hereditary factors.
- Traumatic brain injuries. Often such injuries occur during childbirth.
- Infections (neuroinfections).
- A tumor that affects the hypothalamus. The hypothalamus is a brain structure that performs various functions, including regulating appetite and satiety in a child.
- Chronic foci of infection in the nasopharynx and paranasal sinuses.
- Stress.
- Use of hormonal contraceptives by adolescent girls.
- Pregnancies and abortions in minor girls.
The above reasons play a role in the development of primary obesity (i.e. obesity as an independent disease). It is worth noting that there are cases when obesity develops secondary to other diseases.
There are cases when obesity develops against the background of other diseases.
Causes of obesity
Obesity is a multifactorial disease that occurs as a result of an unhealthy lifestyle, genetic predisposition, or is a manifestation of severe congenital pathology. All causes of obesity can be divided into several groups:
1. Behavioral factors:
- overeating (overfeeding);
- predominance of fast carbohydrates (flour and confectionery products) in the diet;
- lack or insufficiency of physical activity;
- suffered psycho-emotional shock.
2. Related factors (if parents have problems with excess weight, then there is a high probability of a similar condition in the child).
3. Obesity as a secondary manifestation of another disease:
- endocrinological pathology (hypothyroidism, adipose-genital dystrophy, Itsenko-Cushing disease, etc.);
- brain tumors (in particular pituitary tumors);
- lesions of the central nervous system (encephalitis, traumatic brain injury).
The structural unit of adipose tissue is the adipocyte. In childhood, fat cells actively multiply (due to hyperplasia), and after reaching puberty, they increase (hypertrophy). Adipocytes contain large amounts of triglycerides, which are a source of energy for the body. In addition, adipose tissue protects internal organs from mechanical damage, takes part in thermoregulation, and accumulates vitamins A, E, K and D. Enzymatic reactions of the formation and breakdown of lipids, metabolism of fatty acids and triglycerides continuously occur in adipocytes. In a healthy body, a balance is maintained between the synthesis and breakdown of lipids. With excessive accumulation of subcutaneous and visceral fat, the level of adipokines increases, which rearranges the child’s metabolism and leads to multiple organ dysfunction.
Classification of obesity in children
Types of obesity in children
- Primary obesity. The most common form of obesity in children. It is represented by nutritional-constitutional obesity .
- Secondary obesity. Develops against the background of other endocrine diseases.
- Diencephalic obesity. This group includes: hypothalamic, cerebral and mixed obesity. Complex terms, the essence of which boils down to the fact that the child has a disorder in the functioning of the central nervous system. This violation subsequently leads to excess weight in the child. Among this group, it is worth noting hypothalamic obesity . Hypothalamic pubertal syndrome (HSPS) is the most common form of obesity in adolescence and the most common endocrine-metabolic pathology of adolescents in general.
- Hereditary syndromes that are accompanied by excess weight. There are a huge number of them. We will not go into the essence of the problem of each of the syndromes, but will only list the most common of them: Prader-Willi, Lawrence-Moon-Bardet-Bill, Froelich, etc.).
- Mixed.
Thus, the most common forms of obesity in children are nutritional-constitutional and hypothalamic obesity.
Types of obesity in children
There are two types of obesity in children: hypertrophic and hyperplastic. Hypertrophic obesity is characterized by increased accumulation of fat in fat cells and an increase in their size. Hyperplastic is characterized by an increased number of fat cells. From the point of view of prognosis, the most favorable is the hypertrophic type of obesity, as it responds well to dietary treatment and a decrease in the size of fat cells during treatment. Hyperplastic is difficult to treat. Resistance to treatment is associated with irreversibility of the number of fat cells.
Excessive nutrition of a pregnant woman and overfeeding of a child in the first months of life stimulate the proliferation of fat cells and, therefore, contribute to the development of hyperplastic obesity.
Excessive nutrition of a pregnant woman and overfeeding of a child in the first months of life can lead to the development of hyperplastic obesity.
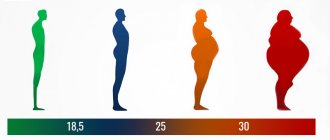
Degrees of obesity in children
The degree of obesity depends on the percentage of excess body weight:
- 1 tbsp. – 10-29%
- 2 tbsp. – 30-49%
- 3 tbsp. – 50-99%
- 4 tbsp. – more than 100%
As a rule, 3 and 4 tbsp. Obesity is almost never based on primary endocrine disorders and is observed in secondary obesity.
Complications of obesity in children
- Disorders of the musculoskeletal system.
- Pathology of the cardiovascular system, lungs, liver, kidneys, gonads.
- Metabolic disorders.
The most serious complications are: type 2 diabetes mellitus, arterial hypertension, atherosclerosis.
Obesity treatment
When treating obesity, the main measures are aimed at reducing body weight and preventing subsequent excess weight gain.
If obesity is secondary, then the doctor will begin by treating the pathology that provokes the development of obesity. But in both primary and secondary obesity, in order to reduce body weight, a change in the child’s lifestyle is necessary: correction of the diet and rational physical activity.
First of all, it is recommended to limit foods containing animal fats and fast carbohydrates in the child’s diet. Meals should be 5-7 times a day. Together with the doctor, the daily calorie intake for the child is calculated, and parents must follow it.
In parallel with changing the diet, it is necessary to change the child’s motor mode. For very young children, long walks and outdoor games are recommended; preschoolers and schoolchildren need to add age-appropriate sports activities (swimming, cycling, athletics, etc.). It is important to understand that a doctor can determine the causes of obesity and give detailed recommendations, but parents must monitor the child’s nutrition and physical activity. And you need to take this as seriously as possible!
Symptoms of obesity in children
Primary obesity (nutritional-constitutional) is characterized by:
- Uniform fat deposition.
- Increased appetite. Characterized by an almost constant feeling of hunger, which does not go away even after a large meal.
- Normal or tall height.
- Delicate, elastic skin. Sometimes pink stretch marks (skin lesions in the form of stripes) and keratosis pilaris (small raised rashes on the skin) are observed.
- Earlier or delayed sexual development.
- Girls experience early menstruation.
- Flat feet and X-shaped knee deformity.
- Increased blood pressure.
- Shortness of breath is common. It occurs even with light physical activity.
- Headaches in the morning associated with decreased oxygen at night.
- A decrease in the child’s self-esteem, the development of depression, which negatively affects the child’s education.
In more severe cases, Pickwick syndrome may develop . This syndrome is characterized by a rapid increase in body weight, narrowing of the upper respiratory tract, cardiorespiratory disorders (rapid breathing, rapid pulse, poor circulation), drowsiness or falling asleep while standing.
It is important to exclude the development of Pickwick's syndrome.
Hypothalamic syndrome of puberty is characterized by:
- The onset of obesity in early childhood. Children aged 11-13 years become especially fat, so they look older than their peers.
- Formation of uniform obesity according to the female type (deposition of fat on the hips and lower abdomen).
- Tall.
- Enlargement of the mammary glands.
- The appearance of pink stripes on the skin of the abdomen, shoulders and thighs - stretch marks.
- Increased blood pressure.
- Constant feeling of hunger. The feeling of hunger especially occurs in the second half of the day, towards night.
- Thirsty.
- Frequent and copious urination.
- Accelerated sexual development. Young men often exhibit pseudoeunuchoid body features, enlarged mammary glands, hypersexuality, and are prone to early sexual activity. Girls may experience increased male-pattern hair growth and menstrual irregularities.
Treatment
Yes, unfortunately, sometimes with our parental love we ourselves prepare fat men and women! But the worst thing is that we are dooming our children to very real suffering and psychological problems. After all, if the sight of a plump baby, as a rule, causes a smile of tenderness, then at school age the child’s plumpness is no longer so liked by parents and others.
Of course, for parents, their child is the best and most beautiful, but offensive nicknames at school and sidelong glances from strangers make them think twice. They begin to limit food, hide sweets, and, what is especially bad, they begin to scold the child for his love of sweets and starchy foods. Moreover, parents, as a rule, do not deny themselves anything.
And in some families they do nothing at all, limiting themselves to eating sweets near the TV and talking about bad heredity.
Of course, sooner or later all this becomes the cause of conflicts in the family, and what is even worse, the development of neuroses in children. Overweight children at school have a more difficult time coping with physical education classes.
They become a convenient target for jokes and pranks of their slimmer peers. An innocent little man develops an inferiority complex that is extremely difficult to get out of his head.
Later, at the age of 14-18, especially for girls, issues of appearance gradually come to the fore. The uncontrollable desire to lose weight in these cases even sometimes leads to the development of severe mental illness ( anorexia, bulimia ).
Doctors very often have to deal with such cases. Some of these patients begin to stubbornly starve themselves, thereby exposing their body to mortal danger. Parents, whose relationships are already hopelessly damaged by that time, have no idea what is happening.
Then it gets worse: stress, discomfort in everyday life, unbalanced diet, intrusive advertising of fast food, sedentary lifestyle. All this completes the work begun by the parents. As the child grows up, he is less dependent on his parents, and the correctness of his nutrition becomes increasingly difficult to control.
In the article “Unchild Weight: How We Make Our Children Sick (Part 2)” you will learn:
- what to do if your child is already fat?
- what to do to prevent your child from gaining excess weight?
How to treat:
- if the recommended body weight is exceeded by 10% ( with forms 1 and 2 of obesity ), a diet, a regimen of increased physical activity, exercise therapy, rehabilitation of chronic foci of infection, and consultation with psychologists are necessary
- for grade 3 and 4 obesity - observation by an endocrinologist, inpatient treatment, constant supervision by psychologists.
Diagnosis of obesity in children
The main condition for diagnosis is excess body weight.
To assess body weight, special tables are used that allow you to determine the ideal body weight depending on the gender, age, and height of the child.
In everyday practice, pediatricians use body mass index, which you can calculate at home. It is determined by dividing body weight in kilograms by height in meters squared (kg/m2). A BMI greater than 30 indicates the development of obesity in a child.
In addition, to make a diagnosis, the doctor may prescribe:
- General blood analysis.
- Biochemical blood test (lipid profile).
- X-ray of the hand. Allows you to determine bone age, which may differ from the passport age.
- X-ray of the skull in two projections. It will allow you to judge the pathology of the pituitary gland, as it shows the state of the anatomical structure - the “sella turcica”.
- Consultation with a neurologist.
- Consultation with an ophthalmologist.
- Determining blood sugar levels, as well as carrying out a sugar load to identify disorders in carbohydrate metabolism.
- Hormonal examination.
- Calculation of the insulin resistance index, or as it is also called the HOMA index. In healthy children and adolescents, the HOMA index is <3.5.
- Determination of leptin levels in the blood.
- Ultrasound of the thyroid gland.
- Consultation with a geneticist – according to indications.
Causes
Are the parents to blame? The question is, of course, tough and offensive, but let's call a spade a spade. So, let's look at the scientifically proven facts.
In infants
A newborn (if, of course, he is born without any congenital pathologies) is an almost ideal biochemically balanced organism. That is, all infants have optimal metabolism and a small number of fat cells.
This does not depend on the weight of the parents, unless this weight is accompanied by the presence of diabetes. Obstetricians know that patients with diabetes almost always give birth to a very large fetus.
We have already discussed this issue in the article “Broad bone: myth or reality?” and let us repeat once again: there is no such thing as hereditary completeness .
Scientists are still studying the obesity gene FTO, but a study conducted on almost 10,000 people has proven one very interesting fact. It showed that people who are confident in the presence of this gene are more likely to gain excess weight than those who are unaware.
Moreover, this turned out to be true for those who actually do not have a “predisposition” to gain weight . Of course, we are not considering isolated cases of congenital pathology.
So it doesn't matter at all whether you have this gene or not. The main thing is how you eat. Genes are generally a very convenient topic. They can justify and explain anything.
If you are always late, you can, for example, justify yourself by heredity - supposedly, this is the problem of all your ancestors right up to the 7th generation, even your great-great-grandfather was a groom and he dared to be late to his master, that’s why you are like that. And there’s nothing to be done: it’s pointless to reprimand genes. But it's all a joke, of course