Fibrosing alveolitis is a series of progressive lung diseases that are characterized by sclerosis of the interalveolar septa and inflammatory infiltration; in which diffuse pulmonary fibrosis is formed and fibrous restructuring of the lung structures occurs.
Most of the diseases combined under this term are also called interstitial pneumonia. And ordinary interstitial pneumonia is called idiopathic pulmonary fibrosis.
- Epidemiology
- Types of fibrosing alveolitis
- Idiopathic fibrosing alveolitis
- Exogenous allergic alveolitis
- Toxic fibrosing alveolitis
Epidemiology
Existing data on the prevalence of these diseases are contradictory. But in most countries there is a constant increase in cases of fibrosing alveolitis. Epidemiological patterns have been clearly identified for allergic alveolitis. Their prevalence depends on a number of factors:
- environmental
- geographical
- household
- professional
The highest numbers of cases are reported among poultry farmers, workers who handle certain types of wood, and those whose work involves flour production. Toxic fibrosing alveolitis is associated with the use of certain medications.
Symptoms
Phases of the disease:
- acute
- subacute
- chronic
The acute course of the disease develops 4-12 hours after inhalation of the allergen. The patient develops a cough, clear sputum, wheezing, shortness of breath, low-grade fever, pain in muscles and joints.
The chronic phase of the disease is accompanied by progressive shortness of breath during exercise, pneumosclerosis, and increased respiratory and heart failure.
Types of fibrosing alveolitis
The term “interstitial lung disease” also includes fibrosing alveolitis. The disease may have an unknown or established etiology. The latter include:
- drug-induced lung damage
- pneumoconiosis
- exogenous allergic alveolitis
Idiopathic fibrosing alveolitis is divided into the following forms:
- bronchiolitis obliterans with organizing pneumonia
- nonspecific interstitial pneumonia
- desquamative interstitial pneumonia
- usual interstitial pneumonia
Medicines
Photo: ipcaz.org
After cleaning the hole, apply a bandage with antiseptic agents. The patient is advised to regularly rinse his mouth, change the bandage, or lubricate the gums with antiseptic and wound-healing drugs. They can be produced in the form of gels, creams, ointments, rinses or aerosols. The basis of treatment is the following:
- Antiseptics. Sprays are used 2-3 times a day after meals. The solutions are used for rinsing the mouth and as lotions (a cotton swab is soaked in the solution and applied to the inflamed hole for half an hour). The gels are applied in a thin layer to the inflamed gum around the hole. Along with special products prescribed by a specialist, hydrogen peroxide is recommended for rinsing (1 tablespoon should be diluted in a glass of warm water).
- Antibiotics. In mild cases, the doctor prescribes an ointment with antibacterial agents. With the progression of the inflammatory process and a high risk of complications, oral antibiotics are indicated along with topical medications. Drug therapy helps stop the progression of the infection and completely stop the inflammatory process within a few days.
- Painkillers. The use of local anesthetics is considered effective. They are usually applied to cotton wool or gauze and applied to the hole. Taking analgesics in tablets is undesirable - they irritate the gastric mucosa, but are less effective than when applied locally in the form of applications. With the simultaneous implementation of other therapeutic measures, after a few days the pain significantly decreases and completely disappears.
Idiopathic fibrosing alveolitis
This is a pulmonary disease of unknown etiology, which mainly affects the alveoli and pulmonary interstitium, and which manifests progressive respiratory failure, explained by developing pneumofibrosis. The morphological variant of this disease affects the severity of symptoms and the nature of the course.
Due to the fact that the cause and pathogens cannot be detected, etiotropic treatment is impossible. It is believed that autoimmune reactions can be induced by various triggers.
The main changes in idiopathic fibrosing alveolitis develop in the area of the air-hematic barrier. These are combinations of various fibroproliferative and cellular immunoinflammatory reactions. Immunocompetent cells accumulate in the interstitial tissue area of the lungs, as do damage mediators :
- chemokines
- interleukins
- oxidants
Due to the peculiarities of pathogenesis with severe pulmonary fibrosis, lung cancer may develop in some cases.
Symptoms are mostly nonspecific:
- severe shortness of breath during physical activity in the early stages
- severe shortness of breath even at rest in the later stages of the disease
- chest pain
- dry cough
- hemoptysis (not in all cases)
Common complaints:
- weight loss
- sleep problems
- severe fatigue
Signs upon examination and auscultation:
- cyanosis of the skin (at a late stage of the disease)
- phalanges of fingers in the form of “drumsticks” and “watch glasses”
- crepitus in the basal regions of the lungs on both sides
The diagnosis of idiopathic fibrosing alveolitis is indicated by the rapid development of the disease, rapidly developing respiratory failure, the development of right ventricular heart failure and pulmonary hypertension.
Instrumental studies
X-ray of the chest organs reveals small-focal and diffuse changes in the left and right lungs, mainly localized in the basal regions. But there may be no changes on the x-ray. As the disease progresses, a “honeycomb lung” may be identified.
FVD research is also instrumental. At the onset of the disease, it is discovered that hypoxia and impaired diffusion capacity of the lungs occur only during exercise. But as the disease progresses, they are also observed at rest. The diffusion capacity of the lungs gradually decreases.
Computed tomography for idiopathic fibrosing alveolitis reveals a “ground glass” symptom and pulmonary fibrosis with a cystic deformation of the pulmonary pattern. This method also evaluates the treatment being carried out. If the area of “ground glass” disappears and there is no increase in cystic structures compared to the data of the last ECG, this indicates the effectiveness of the treatment prescribed by the doctor.
Lung biopsy is a mandatory method for diagnosing idiopathic fibrosing alveolitis. The method has a very high reliability, which makes it easier to choose treatment tactics. Today, thoracoscopic biopsy with video control is relevant. In some cases, a lung biopsy has to be used.
Treatment
Immunosuppressive therapy is the basis of therapy for the disease in question. First of all, glucocorticoids are used: prednisolone 1 mg/(kg/day), pulse therapy with methylprednisolone. Immunosuppressants are effective :
- cyclosporine
- methotrexate
- azathioprine
- cyclophosphamide
In some cases, colchicine is prescribed, which is an alternative to cytostatics and large doses of GC. To slow down the progression of pulmonary hypertension, prostacyclin analogues, endothelin-1 antagonists, and 5-phosphodiesterase inhibitors are relevant.
Forecast
Life expectancy from the onset of the disease with idiopathic fibrosing alveolitis averages 5-6 years. The most favorable course occurs with idiopratic pulmonary fibrosis with the morphological picture of ordinary interstitial pneumonia.
Second opinion on CT scan of the lungs
It must be remembered that in case of a dangerous diagnosis, it is better to consult a qualified specialist. A second opinion on a chest CT scan for fibrosing alveolitis is a re-analysis of the images by a qualified radiologist. You can get a CT scan online using the National Teleradiological Network - this system of remote consultations of radiologists brings together well-known Russian specialists from large medical centers in Moscow and St. Petersburg. Just go to the website https://rentgen-online.ru and download pictures from the disk. After 24 hours, you will receive an official and reliable description of the images, with which you can go to your doctor.
Exogenous allergic alveolitis
This is a group of diseases that arise as a result of intense and prolonged inhalation of dust, which contains proteins of animal and plant origin or inorganic compounds. The diseases are characterized by allergic diffuse damage to the alveolar and interstitial structures of the lungs.
The etiological factor is most often some microorganisms or foreign proteins, large quantities of simpler chemicals. The causative agent of “farmer's lung” is the spores of thermophilic actinomycetes, which are found in moldy hay. “Poultry farmer's lung” is caused by feather antigens, proteins from the droppings of parrots, pigeons, and chickens. The source of the pathogen for “malt worker’s lung” is moldy malt and barley.
Also distinguished in this group are such forms of the disease as “cheese maker’s lung”, “granary worker’s disease” and exogenous allergic alveolitis. The latter is observed among workers in the following industries:
- woodworking
- textile
- pharmaceutical
- chemical
Three processes are important in the pathogenesis of exogenous allergic alveolitis:
- interstitial fibrosis
- interstitial inflammation
- interstitial edema
The stages of the disease are divided into acute and chronic. In acute cases, capillaries and alveolar epithelial cells are affected, intra-alveolar and interstitial edema increases, and then hyaline membranes form. The disease may fade or progress. In the chronic stage, the process progresses to extensive lung damage and collagen deposition. The alveolar spaces, which are lined with atypical cells, are torn.
Symptoms and diagnosis
The entry of an allergen into a weakened body leads to the development of exogenous allergic alveolitis after 4-8 hours. But much more time may pass from the moment of contact (in rare cases). The following symptoms are typical:
- increase in body temperature
- chills
- dry cough
- dyspnea
- joint pain
- chest pain
- headache
- vasomotor rhinitis (not always)
In chronic forms, shortness of breath slowly worsens, fatigue and low-grade fever increase. The first symptoms of exogenous allergic alveolitis sometimes resemble an exacerbation of chronic bronchitis or bilateral pneumonia. In the acute phase, when coughing, it is difficult to separate sputum. The doctor listens for small- and medium-bubble wheezing, and with the development of broncho-obstructive syndrome, dry wheezing. In half of the cases there may be crepitus. As the disease progresses, as with idiopathic fibrosing alveolitis, respiratory failure develops with signs of “cor pulmonale.”
Instrumental studies
Chest X-ray is a mandatory method of investigation for the diseases under consideration. In most cases, inhomogeneous shadowing is found mainly in the lower lobes of the lungs. With swelling of the interalveolar septa, the shading becomes homogeneous. Computed tomography finds consolidation of air spaces, interstitial changes, and a ground glass sign. This method also determines the affected area from which a biopsy is taken.
A study of respiratory function reveals signs of bronchial obstruction in the acute phase and an increase in restriction in the later stages. The following methods are also used:
- Echocardiography
- Electrocardiography
- Open lung biopsy
- Bronchoscopy
Laboratory research
In the acute phase of the disease, pronounced leukocytosis is detected (up to 20x109/l), an increase in ESR to 50 mm/h, and an increase in the content of eosinophils in the peripheral blood.
Differential diagnosis
Exogenous allergic alveolitis is differentiated from:
- eosinophilic infiltrates
- pneumonia
- Wegen granulomatosis
- systemic connective tissue diseases
- disseminated tuberculosis
- sarcoidosis
- pneumoconiosis
- miliary carcinomatosis
- idiopathic hemosiderosis
- alveolar proteinosis
- lymphangioleiomyomatosis
- primary amyloidosis
- Goodpasture's syndrome
Treatment
A mandatory component of treatment is complete elimination of contact with the provoking factor. In some cases, the doctor prescribes glucocorticoids. In the vast majority of cases, cytostatics are not used.
General principles of treatment
Therapy for alveolitis is aimed at eliminating the causes of their occurrence. The child may be prescribed glucocorticosteroids, anti-inflammatory drugs, immunostimulants, and antihistamines. Sometimes physiotherapy is added, as well as spa treatment.
The early stages of alveolitis are easy to treat. Once the fibrotic process has begun, it cannot be stopped; the tissue will not recover. The disease becomes chronic, and the predicted life expectancy is 2-6 years.
Toxic fibrosing alveolitis
This is a pathological process in the lungs, which occurs as a result of the influence of toxic substances on the parenchyma, including some drugs and their metabolites.
The reasons may be production factors:
- metals in the form of fumes, vapors, oxides and salts
- irritating gases (ammonia, etc.)
- plastics
- herbicides
Medicines that most often cause fibrosing alveolitis:
- nitrofurans
- most cytostatics
- penicillamine
- sulfonamides
- hexamethonium benzosulfonate
- amiodarone
- chlorpropamide
- carbamazepine
- hydralazine
Pathogenesis
The pathogenesis of this disease involves damage to the capillary bed of the lungs, impaired diffusion of gases through the alveolar-capillary membrane, disruption of the airborne barrier due to massive necrosis of type 1 alveolocytes, collapse of alveoli due to metaplasia of type 2 alveolocytes and loss of their ability to produce surfactant. Alveolocytes are toxic to both drugs and their active metabolites.
Symptoms and diagnosis
With toxic fibrosing alveolitis, a person experiences shortness of breath. When the causative factor affects the body, shortness of breath becomes stronger. Recovery is likely only when the damaging factor stops. But even under this condition, pathological changes in the lungs can remain and develop; in some cases, severe fibrosis develops.
For diagnosis, it is important to collect a household, professional and allergological history. Often, people with the disease in question exhibit a severe cough caused by irritation by toxic agents in the upper respiratory tract. Possibly pulmonary edema. Percussion methods detect a percussion sound, and crepitus can be heard on auscultation. At the stage of fibrosis, changes in the lungs are almost the same for all types of toxic lung damage.
Treatment
It is important to detect and eliminate the cause, the damaging factor. When signs of acute lung damage appear, the following remedies are effective:
- bronchodilators
- glucocorticoids
- symptomatic cardiotropic drugs
- mucolytics and antioxidants
Oxygen therapy is not always used and only when there is a threat of pulmonary edema. Prevention of gastroesophageal reflux is mandatory. After eliminating the main manifestations of toxic lung damage, monitoring the status of functional pulmonary tests is important. If respiratory dysfunction persists, broncho- and mucolytics should be prescribed.
In all cases, secondary prevention of bronchopulmonary infection is carried out. Physiotherapeutic procedures and breathing exercises are effective in this regard. In case of lung damage caused by drugs, it is necessary to stop taking the corresponding drug.
Causes of the disease
Alveolitis of an allergic nature develops in response to the penetration of inhaled allergens into the respiratory tract. These include mold spores, plant or house dust, and medicinal or protein substances suspended in the air.
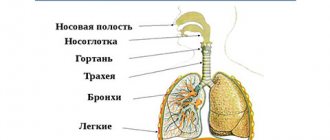
Typically, inhaled particles settle on the mucous membrane of the nasal cavity, trachea and bronchi. But inhaled allergens penetrate deeper, reaching the alveoli due to their small size - less than 5 microns. Upon first contact with them, no reaction occurs. Sensitivity to antigens usually develops after repeated exposure and is accompanied by an allergy.
Folk remedies
Photo: ekonomim24.ru
Treatment using traditional recipes is carried out in accordance with the doctor’s recommendations. At the same time, prescribed drugs from official medicine are used. At the pharmacy you can purchase dried and crushed medicinal plants with antiseptic properties. If after tooth extraction the hole becomes inflamed, infusions of the following herbs are suitable for rinsing:
- chamomile;
- sage, plantain;
- marshmallow, St. John's wort;
- big burdock, elecampane;
- oregano, peony.
You can choose other plants that inhibit the proliferation of pathogens. It is not advisable to rinse your mouth with alcohol tinctures; water infusions have a milder effect. How to infuse herbs:
- take 5 ml (teaspoon) of dry raw materials;
- pour 250 ml of boiling water;
- After cooling to a temperature of 38-39 degrees, strain;
- use as a rinse solution.
When rinsing, certain rules must be followed. Do not rinse your mouth vigorously. A blood clot forms in the hole, and if it is damaged, bleeding occurs. You just need to take the liquid into your mouth, hold it for 1-2 minutes and spit. It is forbidden to use solutions that are too hot; they can cause bleeding and contribute to the spread of the inflammatory process.
Along with the recipes listed above, baking soda is used - it draws out pus well and reduces inflammation. The rinse solution is prepared from 5 ml of soda per 250 ml of hot water. You can rinse your mouth every hour. After rinsing, you should not drink or eat food for at least 15 minutes. If inflammation of the hole occurs due to infection, you need to support the immune system. Recipes to stimulate the immune system:
- Rhodiola rosea. The tincture is sold ready-made at the pharmacy, the recommended dose is 15-20 drops three times a day.
- Echinacea purpurea. Pour 10 ml of dry herb with a glass of boiling water, leave for 15 minutes, strain before use. Drink 100 ml throughout the day.
- Ginseng. The tincture is taken 10-20 drops at a time. The product has a tonic effect, so it is used only in the first half of the day.
If the general condition deteriorates, the temperature rises, pain intensifies or changes in localization, or progressive swelling of the face, folk remedies are ineffective. The listed symptoms indicate the spread of infection and the possible development of complications. It is necessary to urgently contact a specialist.
The information is for reference only and is not a guide to action. Do not self-medicate. At the first symptoms of the disease, consult a doctor.